Teeth are hard tissue formations with high strength that last for a long period of time. The shape and location of individual units affects their functions:
- primary mechanical processing of food is carried out with the help of saliva (chewing, formation of a food bolus);
- formation of sounds (diction);
- protection of the body (prevent harmful microorganisms from entering internal organs).
Many external and internal factors influence when a person’s teeth begin to erupt and until how many years they grow. Among them are the nature of nutrition, the quality and composition of drinking water in the region of residence, hot (cold) climate.
The structure of the dentition
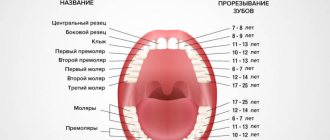
The total number of primary teeth is 20, each jaw has 4 incisors (the central part of the upper and lower rows), as well as 4 molars (“chewing” 4th and 5th units). Adults normally have between 28 and 32 dental units. So, on the upper and lower jaws there is a symmetrical location:
- 4 incisors each;
- 2 fangs;
- 4 premolars;
- 6–8 molars.
Until what age do wisdom teeth grow? You may never wait for the “birth” of the notorious “eights” - congenital adentia of the third molars is considered the norm. Another clinical picture may develop: the wisdom tooth is “embedded” in the jaw, but does not erupt due to a lack of space in the dentition. If “eights” are still born, then this usually happens until they reach a maximum of 25 years of age.
No Ads
Content:
- Why is it necessary to replace baby teeth with permanent ones?
- When do the first baby teeth fall out?
- Which baby teeth fall out first?
- Drop order
- At what age do radical units appear?
- Possible abnormalities in the child
- Why do empty spaces remain unoccupied for a long time?
As the child grows, the baby teeth are replaced by permanent ones. This is a natural process, without which the full functioning of the dentofacial apparatus is impossible. But parents should treat it with the utmost responsibility, since very often violations in the sequence of loss of temporary units cause serious malocclusions that have to be treated in the future.
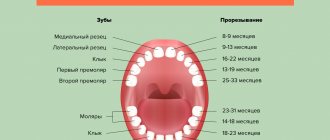
General principles of growth
Baby teeth begin to grow from 6-8 months of age. As a rule, by the first anniversary of his life, the baby has already “acquired” four upper and lower units. By the age of 2 years, the first canines and molars “come into the world”; after another six months, the second molars are added. The final appearance of the primary dentition (20 units) can be observed in three-year-old children.
As a rule, by the end of the first year of life, the baby “acquires” 4 anterior milk units
What to do if by 9 months the baby has not yet acquired a single tooth:
- carefully examine the oral cavity; the gums, as a rule, look slightly swollen and reddened; upon palpation, the tooth edge can be felt;
- in order to speed up the process of “birth” of the first units, pediatric dentists recommend that young parents purchase growth stimulants for baby teeth at the pharmacy - rubber ring toys;
- A light massage of the gums with a clean finger or a cold tablespoon will also only benefit the baby.
Important! Delayed growth of primary teeth can be either a variant of the physiological norm (for example, in boys this process usually begins later than in girls) or a symptom of various pathologies associated with growth retardation (in particular, rickets).
No ads 2
In the latter case, parents should seek help from a pediatrician - perhaps he will prescribe vitamins or calcium supplements to the child to normalize “healthy” mineral metabolism and improve metabolism in general. In rare cases, the absence of signs of teething up to a year indicates edentia (the rudiments of the milk units have simply not formed). In such a situation, the help of a pediatric dentist is required - he will send the child for an x-ray, based on the resulting image, he will make a diagnosis and select treatment.
Starting from the age of 5, baby teeth are gradually replaced by permanent units
To what age do a person’s teeth grow: throughout life, 20 units are replaced at a time (deciduous – permanent), and 8–12 units initially grow as molars. General cutting scheme:
- medial lower incisors – 6–9 months;
- medial upper incisors – 7–10 months;
- lateral upper and lower incisors – 9–12 months;
- first upper permanent teeth – 12–18 months;
- first lower molars – 13–19 months;
- upper (16–20 months) and lower (17–22 months) canines;
- second lower (20–33 months) and upper (24–36 months) root units.
These figures are very relative; it all depends on the individual characteristics of a particular organism. As a rule, by the age of 3, a child has already grown all his milk teeth, and from the age of 5 they begin to gradually be replaced by molars. Why teething may be disrupted: type of feeding (instead of breastfeeding - artificial), genetic factors, loss of baby teeth due to dental problems.
Interesting Facts
Enamel color
The natural color of enamel can be absolutely anything and it is extremely rare that it is snow-white. As a rule, the enamel is slightly yellowish or grayish. In children, teeth may even have a bluish tint, which indicates the presence of a large pulp and its close location to the enamel
About a child's first teeth
Some babies may be born with one or even more teeth, which form in the womb. It also doesn’t matter the age when the baby’s first teeth appear – at three or ten months. The main thing is that, in general, the milk bite is formed completely and correctly.
About the important role of baby teeth
Milk teeth serve primarily as the basis for permanent ones - they literally pave the way for them. If the first teeth grow straight, it is not at all necessary that the subsequent ones will grow as well. However, the opposite situation is also possible, so the formation and growth of all teeth should be monitored under the supervision of the attending physician.
About wisdom teeth
Wisdom teeth may not erupt – this is a completely normal and fairly common occurrence. Whether to remove or leave grown ones depends on their condition: if they only bring discomfort, in the presence of caries or pulpitis it is extremely difficult to cure them, it is quite possible to sacrifice such teeth, since they do not bear any functional load
About oral hygiene
According to statistics, only 57% of women and 46% of men cleanse twice a day. The rest periodically skip such an important procedure, which allows you to effectively cope with plaque and thereby protect the enamel and gums from attack by harmful bacteria.
About using dental floss
According to research, today only 50% of the population flosses daily. Meanwhile, this is an excellent way to prevent many dental diseases: it is the floss that effectively cleans the interdental spaces from food debris and plaque. Today, the only alternative to thread can be an irrigator - a brush cannot cope with such narrow spaces
Growth of milk units
How to find out that your baby is getting his first teeth:
Viburkol for teething
- the gums become red, swell, a white ball can be visually identified, from which the milk unit will later “be born”;
- the child’s cheeks are burning;
- the baby becomes capricious, whiny, refuses to eat and sleeps poorly, and the body temperature may “jump” slightly.
Increased excitability is another “identifying sign” of the onset of teething. The child begins to put foreign objects into his mouth - chewing minimizes discomfort on the oral mucosa. A typical symptom is increased salivation - when the secretion gets on the skin of the face (in the cheeks, chin), it causes the appearance of foci of irritation (rash). Many parents notice limited hyperemic areas on the child’s neck (on the side where the tooth is cut).
Teething is a difficult period for a child’s body; against the background of restructuring and weakened immunity, children can be “attacked” by ARVI. So, if a child has attacks of nausea and vomiting, cough, abdominal pain, runny nose, appetite has disappeared or the body temperature has risen, it is recommended to immediately show him to a pediatrician.
After the appearance of the first milk units, young parents should take care of proper hygienic care for them
Important: you should not additionally stimulate (try to speed up) the process of eruption of baby teeth. Some parents scratch their gums with bread crust, a piece of sugar, and other irritants. Such measures will not have any effect on the “birth” of milk units, but they can provoke injuries to the oral mucosa or “contribute” to the development of a local inflammatory process.
No ads 3
Non-Hong Kong "Triad"
Now that we know so much about the origin and development of the tooth, we can move directly to the topic of interest to us - tissue engineering.
Tissue engineering is a set of methods and procedures aimed at the regeneration of biological tissues. It includes a triad of main elements (Fig. 4): stem cells, extracellular matrix or scaffold, growth factors and signaling pathways [10].
Figure 4. Tissue engineering triad. The basis of the tissue engineering triad is stem cells, growth factors and extracellular matrix.
[10]
The goal of tissue engineering is to replace lost cells, tissues and organs, or promote their regeneration, or simply restore impaired function.
Today we hear and read a lot about stem cells. This is a hotly debated branch of science. The information that goes out to consumers, as a rule, is not always objective. What exactly are stem cells, and how and which of them can be used in dental tissue engineering?
Let's get acquainted: stem cells are undifferentiated embryonic or adult (postnatal) cells that are capable of going through a huge number of cell divisions while in an undifferentiated state, as well as forming intermediate cell types - precursors that can differentiate into various cells and create full-fledged tissues and organs (Fig. 5) [10], [11].
Figure 5. Classification of stem cells according to their ability to differentiate. Based on the scale of differentiation, stem cells are divided into totipotent, pluripotent, multipotent and unipotent. Totipotent cells are capable of differentiating into any cell type of an adult organism. Pluripotent cells can produce specialized cells of the three germ layers (ectoderm, endoderm and mesoderm), but not the entire organism. Multipotent cells produce a limited range of cell types. Unipotent cells are capable of differentiation into only one type of cell [13].
[11]
The first cell line of embryonic stem cells was isolated back in 1998 [12]. In fact, not so long ago, and from the point of view of the course of history one can say quite recently, but the progress is colossal [10].
Embryonic stem cells are isolated from the blastocyst during embryonic development. They give rise to three germ layers: ecto-, endo- and mesoderm. These cells are totipotent, meaning they can develop into each of the more than 200 cell types in the adult body [10].
There are currently 3 known sources of mammalian embryonic stem cells: cells isolated from the inner cell mass of the blastocyst; teratoma cells and primary germ cells of the embryo [10].
As was previously mentioned, stem cells are not only embryonic, but also postnatal. As for “adult” stem cells, they exist in the body in various tissues, including bone marrow, blood vessels, liver, skin, adipose tissue and dental tissue. They are localized in special niches where their proliferation, migration and life span are regulated. Postnatal stem cells are multipotent, meaning they give rise to only one type of cell.
Dental stem cells are a population of postnatal mesenchymal stem cells (MSCs) that have the ability to self-renew and differentiate [4], [14]. Depending on the location of the MSC depot (Fig. 6) [15], they are divided into:
- pulp stem cells;
- apical papilla stem cells;
- stem cells from extracted baby teeth;
- dental follicle progenitor cells;
- periodontal ligament stem cells;
- MSCs obtained from the alveolar process;
- MSCs of the gums;
- progenitor cells (MSCs aimed at differentiation only into a certain type of cell) of the tooth germ.
Figure 6. Dental stem cells. Schematic representation of sources of dental stem cells. For an explanation of the abbreviations, see the box below.
[15]
Abbreviations
WHO World Health Organization MSCs mesenchymal stem cells ECM extracellular matrix ABMSCs alveolar bone-derived mesenchymal stem cells BMP bone morphogenetic protein DFPCs dental follicle progenitor cells DPSCs dental pulp stem cells FGF fibroblast growth factor GMSCs gingival mesenchymal stem cells iPSCs induced pluripotent stem cells PDGF platelet derived growth factor PDLSCs periodontal ligament stem cells SCAP stem cells from the apical part of the human dental papilla SHEDs stem cells from human exfoliated deciduous teeth TGPCs tooth germ progenitor cells germ progenitor cells)
Let's look at some of them.
Pulp stem cells can be quite easily isolated from the pulp of extracted teeth. They represent a very attractive and promising source of autologous stem cells and can be used both for the regeneration of dentin, pulp and cement, and for the restoration of bone tissue [15]. In addition, they exhibit strong neuroregenerative activity, which is of particular value in the treatment of spinal cord injuries: pulp MSCs, in addition to suppressing the early inflammatory response, inhibit the apoptosis of neurons, astrocytes and oligodendrocytes after injury, which leads to the preservation of the nerve fiber and myelin sheath. They have also been found to promote the regeneration of severed axons. Thus, scientists hypothesize that pulp MSCs could provide significant therapeutic benefits in the treatment of spinal cord injury [16].
Stem cells from extracted primary teeth are a postnatal population of stem cells with high proliferative capacity, high viability, and the potential for multilineage differentiation (e.g., into osteoblasts, neuronal cells, and odontoblasts) [15].
Gum mesenchymal stem cells are ideal for restoring damaged periodontal tissue, muscles and even tendons. But it is not yet entirely clear whether they are capable of forming dentin and pulp cells [15].
Tooth germ progenitor cells are a relatively new population of stem cells that were discovered in the mesenchyme of the third molar germ at the bell stage. They show the same multilevel differentiation as other dental MSCs, including the ability to differentiate into adipocytes, osteoblasts, odontoblasts, chondrocytes and neurons, and can also differentiate into cells with the morphological, phenotypic and functional characteristics of hepatocytes. Hence, it is assumed that this type of stem cells can be used in the future to treat liver diseases [15].
Thus, each type of dental stem cells has its own characteristics and areas of application not only in dentistry, but also in other areas of medicine.
In addition to the MSCs described above, induced pluripotent stem cells (iPSCs) derived from somatic cells are also used in tissue engineering. They were first discussed in 2006, when Japanese scientists Kazutoshi Takahashi and Shinya Yamanaka showed that somatic cells can be reprogrammed into iPSCs by increasing the expression of certain transcription factors (Oct3/4, Sox2 and Klf4) [17], [18]. These cells themselves are immunologically neutral and, just as importantly, do not raise the same ethical controversy as embryonic stem cells. However, viral agents were used to reprogram them, which could lead to the formation of neoplasms [19]. There were attempts to use chemical molecules instead of viruses [20], but, unfortunately, the percentage of successful reprogramming turned out to be small. New methods for obtaining iPSCs are now being developed, since their application looks quite attractive and very promising.
How to relieve your baby's condition
Many young parents are wondering how to relieve the unpleasant symptoms that accompany the “birth” of milk units. The simplest measure is to apply cold (a piece of ice) to the “working” gum. Dental gels or ointments can also come to the rescue, relieving pain, swelling, and stopping the inflammatory process. Important: any medications should be used only with the permission of a pediatrician (pediatric dentist).
Thus, pharmacies sell special gels with lidocaine and inert fillers (menthol, astringents, flavorings) intended for use exclusively during teething. Examples of such tools:
- Kalgel (contraindicated for diathesis).
- Dentinox.
- Kamistad.
- Holisal.
- Mundizal.
General recommendations for use: a small amount of the local drug should be applied to the “working gums” 3-4 times a day for no longer than 3 days in a row.
How do “eights” erupt?
It is impossible to give an unambiguous answer to the question of when wisdom teeth begin to grow and until what age do they grow. Third molars “come into the world” in the period from several months to 2-3 years, causing a lot of unpleasant sensations. When the “eights” begin to grow is influenced by many factors - in particular, the number of bone buds, heredity, and the anatomical features of the jaw (its shape). Due to the fact that third molars often create a certain discomfort - they affect the functioning of the TMJ, provoke sinusitis, and “displace” neighboring units of the dentition - they are often removed.
The main indications for extraction are:
- persistent hyperthermia (2–3 days) during the growth of wisdom teeth;
- acute inflammation of the gums (gingivitis) at the site of eruption;
- severe pain that makes eating difficult.
Anatomical features (shape) of the jaw, heredity and a number of other factors determine the timing of teething
What does it cost us to build a tooth?
To use stem cells in tissue engineering, the presence of a scaffold and growth factors is required (Fig. 7). An ideal scaffold should support cell attachment, migration, proliferation, and spatial organization.
Figure 7. What does it cost us to build a tooth?
website dentistry.tamhsc.edu
Basically, a scaffold as a suitable matrix for tissue reconstruction should meet the following requirements [21]:
- Ease of use.
- The presence of pores of a certain shape and size for the diffusion of cells, growth factors, nutrients and removal of waste products.
- The ability to biodegrade, which occurs at a certain time without releasing toxins.
- Biocompatibility with body tissues.
- Low immunogenicity.
- Ability to be replaced by regenerating tissue and vascularization.
- Good physical and mechanical properties.
The materials used to form scaffolds are divided into natural and synthetic (Fig. [22]. Bioactive glass, polylactic acid, various composites (multicomponent materials based on a matrix based on metal, polymer or ceramic) - all these are synthetic materials. Despite the fact that these materials make it possible to produce scaffolds of the required shape, their use is very limited due to unsatisfactory biocompatibility and toxicity. Among the biomaterials (natural materials) used to create scaffolds, collagen, chitosan, and hyaluronic acid can be distinguished. They consist of macromolecules that They are also part of the extracellular matrix, therefore they are biocompatible and highly biodegradable, but they are less durable and can cause rejection reactions [21].
[22]. Bioactive glass, polylactic acid, various composites (multicomponent materials based on a matrix based on metal, polymer or ceramic) - all these are synthetic materials. Despite the fact that these materials make it possible to produce scaffolds of the required shape, their use is very limited due to unsatisfactory biocompatibility and toxicity. Among the biomaterials (natural materials) used to create scaffolds, collagen, chitosan, and hyaluronic acid can be distinguished. They consist of macromolecules that They are also part of the extracellular matrix, therefore they are biocompatible and highly biodegradable, but they are less durable and can cause rejection reactions [21].
Figure 8. 3D scaffold of mouse and human teeth. a — Lower central incisor of a mouse. b — Human lower first molar. 3D reconstruction and bioprinting were used. Material: hydroxyapatite and polycaprolactone. Microchannels (d = 200 nm) into which MSCs and growth factors are introduced ( c and d ) are visualized.
[22]
The most suitable scaffold that meets most requirements is either a scaffold derived from extracellular matrix ( ECM scaffold ) or its analogue. Due to their identity with the extracellular matrix, such scaffolds are able to provide the best interaction with cells and growth factors. Dental MSCs, such as pulp and periodontal stem cells, when cultivated in ECM scaffolds, underwent differentiation in the odontogenic direction. After implantation of this scaffold, the pulp was formed [10], [23].
In addition to the scaffold and stem cells, a link is needed that connects them, which would regulate tissue growth. These can be growth factors, certain genes, and interfering RNAs [7].
Growth factors are peptide molecules that transmit signals to control cellular behavior and interact with specific receptors on the surface of cells [24]. They provide interconnection and interaction between cells and the extracellular matrix. Following cell damage, the secretion of growth factors begins, which subsequently trigger the processes of regeneration and angiogenesis. An example of the “work” of growth factors in a tooth is the formation of secondary and tertiary dentin, which occurs when the carious cavity is close to the dental pulp or when teeth are subject to increased abrasion. Key growth factors during tooth development include bone morphogenetic protein (BMP), platelet-derived growth factor (PDGF), and fibroblast growth factor (FGF). They are primarily used in dental tissue engineering [25–27]. Both cells and nanoparticles, as well as the scaffold itself, can be used to deliver growth factors.