On August 9, 1974, for the only time in the history of the United States of America, a president of the country resigned before the end of his term.
***
“As the clock strikes midnight in Washington, a red-eyed creature with the legs of a man and the head of a hyena crawls out of a bedroom window in the south wing of the White House and leaps fifty feet onto the lawn. Pausing there only to strangle the watchdog, she rushes off into the darkness... to Watergate...” - this is what writer Hunter Thompson US President Richard Nixon in the midst of the famous Watergate scandal in his book “The Great Shark Hunt.”
Related article President with a boyish smile. Life of John Fitzgerald Kennedy
Nixon was initially one of the most controversial US presidents. He became the first Republican president elected after the main political tragedy in American history - the assassination of John F. Kennedy in 1963. It is on Nixon’s hands that the blood of thousands of American soldiers who lost their lives tens of thousands of kilometers from their homeland - during the failed American military campaign in Vietnam. Riots, demonstrations, and pogroms in the United States were dispersed by thousands of police officers on the orders of the president.
Against this backdrop, the 1972 election campaign took place, in which Nixon's main opponent was the unexpected Democratic candidate George McGovern . As a result, Nixon still won those elections - McGovern was a weak candidate who, among other things, also lost the support of some party leaders, and also did not find an ally in the third of the Kennedy brothers, who refused to be his vice president.
George McGovern. Photo: www.globallookpress.com
Mechanical injuries of the pharynx
Causes.
Mechanical injuries of the pharynx can be internal, external, closed, open (wounds), isolated, penetrating, non-penetrating, blind, through.
Internal wounds of the pharynx are often isolated and occur when damaged by a foreign body (pencil, stick) inserted into the oral cavity. External wounds of the pharynx are predominantly combined with damage to the neck, head, esophagus, and can be cut, stabbed, bruised, or gunshot.
Symptoms.
Injuries to the oropharynx are often combined with damage to the facial skeleton, soft palate, tongue, cervical vertebrae, retropharyngeal and peripharyngeal space. The main manifestations are the presence of a wound, pain, dysphagia, salivation, speech disorder, bleeding, swelling, emphysema of the lateral pharyngeal wall.
Injuries to the laryngopharynx are often combined with damage to the larynx and esophagus and are characterized by severe general condition, external or intrapharyngeal bleeding, dysphagia, aphagia, respiratory failure including asphyxia, subcutaneous emphysema in the neck. The flow of saliva or food from the wound indicates the penetrating nature of the wound to the pharynx or esophagus.
Complications.
Blood loss, aspiration asphyxia, pneumonia, retropharyngeal abscess, purulent mediastinitis.
First medical aid.
In case of superficial damage to the mucous membrane of the oropharynx, the wound is treated with a 3% solution of silver nitrate; in case of deep damage, tetanus toxoid, analgesics, and antibiotics are also administered. In case of severe arterial bleeding, it is temporarily stopped by digitally pressing the common carotid artery to the C-VI vertebra. They are urgently evacuated to the ENT department of the hospital.
Specialized assistance
provides for the final stop of bleeding and primary surgical treatment of the wound. Some victims, after preliminary tracheostomy, undergo pharyngeal tamponade. If tamponade is ineffective, the bleeding is stopped by ligating the main vessels along their length.
During primary surgical treatment, non-viable tissues, foreign bodies, bone fragments are removed, and hematomas are opened. A large tissue defect and severe inflammation require open treatment of pharyngeal wounds. Tracheostomy is also performed if there is a threat of decompressed laryngeal stenosis. Feeding is provided through a tube inserted through the nose (or mouth). Adequate antibacterial and infusion therapy is prescribed.
"Palevo"
Peter Romanov:
Vietnam: a medieval war of the 20th century At that time, American politics involved not only national campaigns, in which candidates went on trips throughout the country, went into the homes of ordinary Americans, visited them in the workplace, and also spoke on the podium in big and small cities. There were also dirty technologies. One of the main weapons in the hands of dishonest politicians has become wiretapping of telephone lines. Even during the party primaries, George McGovern's representatives ensured that all communication cable hatches in the area around their headquarters were sealed and no one had access to them.
On this basis, a grandiose scandal ripened, which began with a minor incident, to which no one paid much attention at first. In the Watergate complex, where Democratic candidate McGovern's campaign headquarters was located on June 17, 1972 (four months before the US presidential election), five people were detained who were trying to install listening devices.
However, this incident remained away from the media, and no fuss followed. Life went on as usual, Nixon won the presidential election, and the FBI was investigating the penetration of McGovern's headquarters, trying not to talk about its details.
Watergate Hotel. Photo is in the public domain
The storm struck in January 1973, when the trial of the burglars began. It has not yet been proven that they intended to conduct espionage for and at the behest of the current President Richard Nixon, but public opinion immediately formed a picture of a “dirty” election struggle on the part of the ruling Republican. Considering that he was not very popular among the people anyway, the case quickly became overgrown with “details.”
Article on the topic
"Honest Abe." How Abraham Lincoln Became the Conscience of the American Nation
Investigators began to cling to any lead, even if it did not relate specifically to the case with the Watergate burglars. As a result, numerous violations committed by Richard Nixon and his administration during his tenure as president were revealed, including non-payment of taxes on very large sums.
As a result, investigators, in an unprecedented judicial decision, received the right to access the recordings of all conversations that took place in the Oval Office of the White House. In one of them, a few days after the burglars were caught, Nixon called the incident, literally translated from English, a “smoking gun.” In a more accurate translation into Russian, this slang expression can be correlated with the word “palevo”. In addition, from the conversation it became clear that the president was doing his best to slow down the investigation and prevent it from proceeding.
The publication of this tape completely deprived Nixon of support in society and absolutely all supporters in the political arena. Many of his associates had already left their posts and were under investigation for a number of violations and crimes. At the same time, the impeachment process began, which was interrupted by Nixon's resignation letter on August 9, 1974.
“To the Honorable Henry A. Kissinger, Secretary of State. Dear Secretary of State, I hereby resign as President of the United States. Sincerely, Richard Nixon August 9, 1974." Photo is in the public domain
Fungal diseases of the pharynx
At the turn of the XIX-XX centuries. Almost all the main human mycoses and their causative agents have already been described. The names of Virchow, Hrubi, Remarque, Schönlein, and then Sabouraud are closely connected with the history of the development of medical mycology. Due to the widespread use of antibiotics, the second half of the 20th century. was accompanied by a significant increase in the incidence of mycoses, which currently affect from 5 to 20% of the adult population (A. Yu. Sergeev, Yu. V. Sergeev, 2003). Among all mycotic lesions of the human body, in second place after onychomycosis is candidiasis of the mucous membranes, up to 40% of cases of which, in turn, are oropharyngeal mycosis (V. Ya. Kunelskaya, 1989).
Among mycoses of the pharynx (pharyngomycosis), the most common (in 93% of cases, according to V. Ya. Kunelskaya (1989), and in 90%, according to T. N. Burkutbaeva (2002)) is candidiasis caused by the yeast fungus Candida, which combines 20 species (A. Yu. Sergeev, Yu. V. Sergeev, 2003). In patients with pharyngomycosis, as a rule, eight different types of pathogens are identified, among which four main ones “lead”: C. albicans, C. tropicalis, C. parapsilosis and C. glabrata. The first place is occupied by the disease caused by C. albicans. This species is found in the mouth and throat of 60% of healthy adults, more often in women and men who smoke. Other Candida species are significantly inferior to C. albicans in the number of discharges from healthy individuals, accounting for 10 to 20% of all cases of oropharyngeal candidiasis. In second place after C. albicans is usually C. glabrata, especially in elderly patients, less often - C. tropicalis, C. parapsilosis (in the latter case - in almost 50% of candidiasis-carrying children). With oropharyngeal candidiasis in HIV-infected people, rare species of Candida—C. sare, C. dubliniensis, C. famata, C. lipolytica and C. guilliermondii—more often appear among the pathogens. It has also been reported that C. rugosa has been isolated from diabetic patients, C. inconspicua and other yeasts from cancer patients. When treated with systemic antimycotics and antibiotics, the proportion of resistant species, C. glabrata and C. krusei, as well as C. kefyr, including those isolated simultaneously with resistant strains of C. albicans, may increase (MD Richardson, DW Warnock, 1997).
Much less often - in 5-6% of cases - mycosis of the pharynx is observed, caused by the bacterial microorganism Leptotrix buccalis and the fungi Aspergillus, Penicillium, Mucor, etc. In some cases, damage to the pharynx is caused by two or more types of fungi - Pharingomycosis mixta.
Almost all of these types of fungi are saprophytes, opportunistic microflora; they are activated and become pathogens when the body’s reactivity is impaired (I. V. Chumicheva, 2003).
The development of pharyngomycosis is provoked by diabetes mellitus, systemic diseases of the blood and gastrointestinal tract, especially intestinal dysbiosis. Deficiency of bifidobacteria and other lactic acid bacteria leads to disruption of the synthesis of B vitamins and to the unhindered colonization of fungi not only in the intestines, but also in other body cavities in contact with the external environment (nasal cavity, mouth, ear). In addition, malignant neoplasms have a negative impact, in which the balance of vitamins, carbohydrate and protein metabolism is disrupted, and the body’s general, including antimycotic, resistance suffers. Mycoses are especially common in AIDS patients, 10% of whom die from fungal infections. Often, pharyngomycosis of the pharynx and oral cavity develops with prolonged and improper use of topical glucocorticosteroids for bronchial asthma.
In the formation of pathogenetic mechanisms of fungal infection of the pharynx, the first place is taken by the restructuring of immune reactivity - the accumulation and circulation of fungal antibodies in the blood, which cause immediate and delayed reactions. Changes in cellular immunity are also important. An important link in the pathogenesis of pharyngomycosis is specific and nonspecific sensitization and allergy. Traumatic damage to the mucous membrane of the pharynx also plays a certain role here - as a factor predisposing to the development of a fungal process.
Mycotic foci in the pharynx are usually localized on the palatine tonsils, arches, velum, posterior wall, and tongue. Tissue reactions are expressed by atypical hyperplasia of the epithelium, the formation of granulomas, sometimes having a pseudotuberculous character, as well as necrotic changes of varying severity. Epithelial hyperplasia in the form of hyperkeratosis is especially pronounced in the crypts of the tonsils against the background of an inflammatory process in the stroma and can take the form of papillomatosis. In the tissues of the mucous membrane of the pharynx, tongue and stroma of the tonsils, fungal elements located subepithelially are detected.
Microscopy of a native preparation is the simplest and most reliable method for diagnosing mycoses, allowing not only to determine the presence of a fungus in the test material, but also to distinguish saprophyty from a fungal disease. With saprophyty, only single non-budding cells are found in the preparations, and with mycosis, all elements of fungi are constantly determined in each preparation: both mycelium and blastospores.
Material is collected from the pharynx for testing for fungi using ear tweezers, Hartmann ear forceps or a Volkmann ear spoon. It is unacceptable to use a cotton swab for this purpose, since the bulk of the sticky pathological content remains on the swab, and therefore a false negative result is possible during microscopic examination or culture. The collected material is carefully applied to a sterile glass slide. The material should not be rubbed on glass, as this may damage the delicate elements of the fungus, which also reduces the reliability of microscopy results. Microscopy of the unstained and Romanovsky-Giemsa-stained native preparation is performed, inoculation of the pathological discharge obtained by scraping from the tonsils or the posterior wall of the pharynx on Sabouraud's selective nutrient medium, followed by subculture of fungal cultures on Chanek's medium to identify the pathogen. When isolating a Candida culture, quantification is often required. In the case of actinomycosis, microscopy reveals a significant proliferation of granulation tissue with actinomycetes.
Immunological diagnosis is based on the detection of pathogen antigens in the blood. Serological diagnostics is a type of immunological diagnostics that makes it possible to detect antibodies to the components of the pathogen cell in the blood. A feature of immunological diagnostic methods is that serial sets of antibodies or antigenic diagnostics are developed only for a few of the most common pathogens (candidiasis, cryptococcosis, aspergillosis; diform fungi). The disadvantages of immunodiagnostic methods include insufficient sensitivity and specificity. However, with the help of immunodiagnostics it is possible, in particular, to monitor the effectiveness of treatment by reducing titers (A. Yu. Sergeev, Yu. V. Sergeev, 2003).
Mycotic lesions of the pharynx can be acute, in which case it is usually accompanied by widespread lesions of the oral mucosa and pharynx, and chronic, in which the lesion is often limited to the palatine tonsils (tonsillomycosis) or the posterior wall of the pharynx (pharyngomycosis); a distinction is made between recurrent and persistent forms of chronic pharyngomycosis. According to the clinical and morphological picture, pharyngomycosis is divided into pseudomembranous, which occurs most often in this localization; erythematous (atrophic), hyperplastic (hypertrophic, or candidal leukoplakia); erosive-ulcerative are rare (A. Yu. Sergeev, Yu. V. Sergeev, 2003).
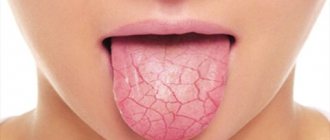
The clinical picture of pharyngomycosis is varied and is determined not so much by the type of fungus that caused the disease, but by the general and antimycotic activity of the body. The clinical picture of candidiasis, penicilliosis and aspergillosis is almost identical (M. R. Bogomilsky, V. R. Chistyakova, 2001). The disease is characterized by sore throat, fever, hyperemia of the mucous membrane, the appearance of small white plaques at first, and then extensive necrosis of the epithelium, which occurs under the influence of its infection by fungi, which persist when treated with traditional conservative methods. On the mucous membrane, multiple grayish-white plaques of irregular shape are visible, located on the tonsils, arches, palate, as well as in other places and are difficult to remove; after their removal, an eroded surface remains. In the chronic form, typical complaints appear with a characteristic cyclicity, after two to three weeks. With superficial mycosis, a mildly expressed hyperemia of the mucous membrane is determined with small areas of translucent or dense peak-shaped plaques of a grayish or white color, often having a cheesy, lumpy character. The plaque is easily removed, revealing a smooth, hyperemic mucous membrane. In some cases, plaque can merge and become denser. After their removal, the mucous membrane is exposed, bleeding at the slightest damage, which is very reminiscent of damage to the pharynx due to diphtheria. With ulcerative-membranous lesions, the process is usually localized on infiltrated, tuberous tonsils and spreads to adjacent formations. Ulcers with uneven edges are covered with a white coating that can be easily removed. Regional lymph nodes (za- and submandibular) enlarge slightly and are slightly painful (I. V. Chumicheva, 2003).
Often such lesions are found not only in the pharynx, but also in other parts of the respiratory and digestive tracts, which significantly worsens the patient’s condition. Infection of internal organs by fungi is characterized by an exceptionally severe course, similar in symptoms to sepsis (V. Ya. Kunelskaya, 1989).
Pharyngomycosis is often combined with candidal lesions of the corners of the mouth - “jams”, candidal cheilitis, glossitis. The red border of the lips is sharply hyperemic, infiltrated, has transverse striations, and is covered with a thin grayish coating. In the corners of the mouth there are cracks covered with curdled crusts, painful when opening the mouth. The disease lasts 7-12 days and often has an undulating course. Recurrence of the process is noted in 20-22% of cases (I. V. Chumicheva, 2003).
Leptotrichosis of the pharynx is expressed by the formation of spiny, pointed, very dense outgrowths (stalked films in the form of spikes) of gray or yellowish-gray color on the surface of the unchanged mucous membrane of the palatine, lingual, pharyngeal tonsils, lateral ridges and granules of the posterior wall of the pharynx, as well as on the palatine arches. These outgrowths are a consequence of keratinization of the squamous epithelium, come off with difficulty, in parts and contain Leptotrix buccalis cells. The disease is often asymptomatic and long-lasting; sometimes patients complain of a sensation of a foreign body in the throat. There are no inflammatory changes in the mucous membrane and no fever. The course of the disease is persistent (V. Ya. Kunelskaya, 1989).
Actinomycosis is characterized by the formation of dense, lumpy infiltrates of a dark red color (specific infectious granuloma), slowly growing (sometimes the process manifests itself in the form of acute phlegmon), located most often in the area of the mouth and neck, less often in the area of the tongue, tonsils, nose and larynx. Over time, the tumor suppurates and abscesses form. The surrounding tissues of the chin and cheek are involved in the process, then the tumor can open on its own to form a fistula. In the contents you can find yellow-green druses of the fungus. Due to inflammatory swelling of the masticatory muscles, their trismus appears; regional lymphadenopathy is uncharacteristic (M. R. Bogomilsky, V. R. Chistyakova, 2001).
Candidomycosis of the pharynx should be distinguished from diphtheria, fusospirochetosis and damage to the pharynx due to blood diseases (V. Ya. Kunelskaya, 1989).
A comprehensive method of treating tonsillo- and pharyngomycosis includes three fundamental principles.
- General and local use of modern antifungal drugs (previously used antibiotics are canceled).
- Restoration of disturbed intestinal microbiocenosis. In correcting changes in intestinal microbiocenosis, in turn, three factors are important: normalization of chemical processes in the intestine and the fight against opportunistic flora with the help of diet (products with a bactericidal effect), antibacterial agents, intestopan, mexaform;
- taking bacterial preparations containing live cultures (bifidumbacterin, colibacterin, lactobacterin);
- increasing nonspecific defense reactions of the body, promoting the formation of healthy microflora; For this purpose, eubiotics (atsipol, bactisubtil, hilak-forte, linex) are used in complex therapy of candidiasis from three weeks to three months.
In most cases, treatment of pharyngomycosis begins with the prescription of local therapy, and then, if necessary, systemic therapy with azole derivatives is added: fluconazole (Diflucan, Mycosist, Flucostat, Flumicon) 100 mg/day, ketoconazole (Nizoral) 200 mg/day, and also itraconazole 100 mg/day, etc. In this case, systemic drugs are taken for one to three weeks from one to three courses (LL Patton et al., 2001). The antimycotic effect of these drugs is based on disruption of the synthesis of ergosterol (mycostatic) or its binding (mycocidal) to ergosterol, the main component of fungal cell membranes.
Drugs for local etiotropic therapy are divided into antiseptics and antimycotics. The duration of treatment of acute forms with local antimycotics is usually two to three weeks, with antiseptics - somewhat longer. Treatment is carried out until clinical manifestations completely disappear, and then continues for another week (H.-J. Tietz, 2002).
Antiseptics with antifungal effects are usually prescribed in the form of lubricants and rinses. Lubrication is carried out with 1-2% aqueous solutions of brilliant green or methylene blue, applying them to the previously dried surface of the mucosa. These drugs are widespread and available, but they are inferior in effectiveness to antimycotics, resistance to them quickly develops, and their continuous use leads to irritation of the mucous membrane. Lugol's solution diluted two to three times, or a 10-15% solution of borax in glycerin, are more effective. Rinsing with solutions of potassium permanganate (1:5000), 1% boric acid is carried out two to three times a day or after each meal (M. R. Bogomilsky, V. R. Chistyakova, 2001). It is recommended to alternate local antiseptics every week. Modern antiseptics are more effective - 0.12% chlorhexidine bigluconate or 0.1% hexetidine solution, which is also available in the form of an aerosol. For rinsing, you need 10-15 ml of any of these solutions; the procedure is performed for 30-60 seconds after meals, twice a day. The aerosol is sprayed for 1-2 s. Unlike rinses with antifungals, antiseptic solutions should not be swallowed.
Antimycotics - polyene antibiotics (nystatin, levorin, amphotericin, natamycin, etc.) and imidazole derivatives (fluconazole, ketoconazole, clotrimazole) - are prescribed in the form of solutions, aerosols, drops, regular and chewable tablets. It is necessary to explain to the patient that any drug for local treatment should remain in the oral cavity as long as possible. Nystatin tablets should be chewed and the pulp should be kept in the mouth for a long time. When quickly swallowed, they have no effect on the mycotic process in the pharynx, since they are not absorbed through the intestinal wall.
There is a preliminary report of the effectiveness of the topical non-steroidal benzydamine, available as a spray and rinse. It has anti-inflammatory and local anesthetic effects, promotes epithelization. Irrigation with benzydamine is carried out three to six times a day, an hour before or an hour after meals (I.P. Petrova, A.I. Mashchenko, 2002). However, the status of this study does not allow us to make a final conclusion about the effectiveness of the drug.
In case of widespread candidiasis of the pharynx, it is not recommended to carry out surgical interventions on the lymphatic pharyngeal ring, washing the lacunae of the tonsils, UHF and microwave therapy, steam inhalations, compresses on the neck, as well as the use of penicillin and tetracycline antibiotics (M. R. Bogomilsky, V. R. Chistyakova, 2001). In case of leptotrichosis, removal, cryo- or laser destruction of pathological structures is performed only on the palatine tonsils. In the case of actinomycosis, complex treatment is prescribed: antibacterial and antifungal therapy, iodine preparations orally, wide opening, drainage and washing of inflammatory infiltrates with antiseptics, immunotherapy (actinolysate injections). In severe cases, radiotherapy is performed.
The following recommendations have been developed for the prevention of oropharyngeal candidiasis.
The duration of courses of antibiotic therapy should be sufficient to eradicate the bacterial pathogen, but no more. Antibiotics should not be prescribed prophylactically, particularly for respiratory viral infections. When prescribing repeated courses of antibiotic therapy, mandatory concomitant antifungal therapy is indicated.
It is necessary to monitor the condition of the oropharyngeal mucosa during treatment with local and systemic corticosteroids; Nebulizers are used in the treatment of bronchial asthma.
After each meal, you should thoroughly rinse your mouth with boiled water, a 2-3% solution of baking soda, a weak solution of potassium permanganate, and also brush your teeth with pastes containing antimicrobial additives.
It is necessary to promptly treat caries, periodontitis, chronic tonsillitis and other diseases of the oral cavity and pharynx (A. Yu. Sergeev, Yu. V. Sergeev, 2003).
For questions about literature, please contact the editor
I. I. Akulich, Candidate of Medical Sciences A. S. Lopatin, Doctor of Medical Sciences, Professor of the Central Clinical Hospital of the Medical Center for the Administration of the President of the Russian Federation, Moscow