The nature of the appearance of a runny nose during teething
Parents and pediatricians always play it safe as soon as they discover any abnormalities in the baby’s condition. Therefore, even a slight runny nose is often treated like ARVI. This is correct, because babies do not yet know how to blow their nose normally, and sputum flows down the trachea into the bronchi. This can subsequently lead to complications such as bronchitis or even pneumonia.
However, it is not always necessary to rely on vasoconstrictor drugs. A runny nose during teething occurs:
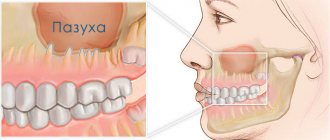
- non-infectious nature. The problem of snot during the period of teeth growth in a baby is explained by physiological reasons. The anatomical structure of the nasopharynx is as follows: the blood supply to the gums and mucous membranes of the nasal passages is carried out through a network of vessels that are closely interconnected due to their close location. During teething, the blood supply to the gums increases, so the mucous membranes begin to work more actively - saliva is produced abundantly in the oral cavity, and nasal mucus ;
- against the background of a respiratory infection. When a baby is teething, his local immunity suffers a slight disruption. Resistance to colds decreases, so the child easily picks up any virus.
If a runny nose is caused by physiology, snot on the teeth may not go away for weeks, which is not typical for ARVI.
As for nasal congestion due to a respiratory infection, excessive mucus production is not the only symptom. Other catarrhal phenomena and changes in the baby’s well-being will not be long in coming.
General recommendations for pregnant women who have symptoms of rhinitis
- Rinse the nose with a weak saline solution (2 teaspoons of sea salt per glass of water). Saline solution improves the passage of mucous discharge from the nose and reduces the feeling of stuffiness.
- Nasal douches (nasal rinsing devices) help very well. You can use regular saline solution for them.
- Ventilate the room before going to bed, use humidifiers. Dry air can increase unpleasant symptoms.
- Use a high pillow (or several pillows) to sleep so that your head is significantly higher than your torso.
- Walking in the fresh air before bed is beneficial.
- Do exercises in the morning and breathing exercises several times a day to reduce the symptoms of hypoxia.
- Don't wear perfume and try to stay away from smokers.
During pregnancy, vasoconstrictor nasal drops should not be used, as they can provoke vasomotor rhinitis.
How to distinguish a runny nose of an infectious nature from snot on teeth
Most mothers complain that it is impossible to understand what causes nasal congestion in their baby. In fact, determining why a baby has snot on his teeth is not so difficult.
Normal Teething Symptoms
In anticipation of the tooth breaking through the gum, some babies become restless, have difficulty sleeping and eating. The main symptoms of teething are:
- The baby's gums swell and become red. If you lift your lips, you can see that the crown of the tooth is already in the gum and is about to break through it;
- excessive salivation;
- refusal to eat, poor appetite;
- the child constantly chews everything that comes to hand;
- the baby looks overexcited, distracted and tired. He sleeps poorly and is often capricious;
- body temperature can either rise or fall, or constantly remain within subfebrile levels;
- the baby develops clear snot;
- Loose stools may occur - up to 4 times a day.
All these signs disappear and the child’s condition returns to normal as soon as the tooth breaks through the gums. Usually the condition improves immediately after a piece of the dental crown is cut through.
The appearance of a new tooth against the background of ARVI
If the baby has picked up some kind of infection, then all of the above symptoms will be accompanied by the following:
- elevated temperature up to 38.5C;
- profuse runny nose - the snot is initially transparent, then white or yellow;
- red throat and inflamed tonsils;
- dry cough (usual coughing is normal with a runny nose, we are talking about a deep cough);
- general lethargy and weakness;
- tearfulness.
These are signs of a typical respiratory infection, which often occurs due to a decrease in the baby's immune system during the period of the appearance of a new tooth.
Main differences
I don’t want to stuff my baby with medications one more time. Therefore, one can understand the desire of parents to understand when a runny nose on the teeth is normal, and when it is a manifestation of an illness. You can distinguish snot on your teeth from a cold by the signs given in the table below.
| Snot on teeth of non-infectious nature | Runny nose during teething due to ARVI |
| All symptoms occur suddenly and together, rather than one after another. The baby immediately develops a fever, a runny nose and other signs. | The malaise appears gradually. The first two days there is a fever and redness of the throat, then a runny nose begins. |
| The child’s throat is not red, the tonsils are not enlarged. | Obvious hyperemia of the larynx, enlarged and inflamed tonsils. |
| The snot is transparent, thin, like water. There is not a lot of mucus, and there is almost no swelling of the nose. | As the disease progresses, the snot becomes white or yellow and thick. It is difficult for the baby to breathe through his nose due to severe swelling. |
| The baby may cough slightly as mucus drains into the larynx. As a rule, this does not cause any complications, and the cough disappears along with the snot. | At the beginning of the disease, the child may have a dry, barking cough. After a profuse runny nose appears, it becomes deep and hoarse. |
| A runny nose can last for two weeks, and it will end exactly when the crown of the tooth appears on the gums. | Thick snot disappears in 7-10 days. Then they can be replaced by transparent ones, which will stop bothering you as soon as the tooth comes out. |
Interesting fact! A fever in a child’s teeth may appear for 5-7 days, whereas with ARVI it does not last more than 3-4 days in a row from the moment the first symptoms appear. You can also distinguish a fever from a cold by the marks on the thermometer. If it rises sharply and falls heavily throughout the day, this is a manifestation of teething. If it easily becomes confused and disappears completely by the evening, but the tooth does not appear, then we are talking about ARVI.
Sometimes the symptoms of the disease overlap with the natural signs of teething, so you should contact your pediatrician in any case!
Particular runny nose. What is vasomotor rhinitis and how to get rid of it?
What is vasomotor rhinitis and how to get rid of it? What consequences can result from improper treatment of vasomotor rhinitis? These and other questions are answered by the leading specialist of the National Medical and Surgical Center. N. I. Pirogova, candidate of medical sciences, associate professor, otorhinolaryngologist Oleg Aleksandrovich Golubovsky.
— Oleg Alexandrovich, what is vasomotor rhinitis? What is its feature?
— Let's start with the fact that a runny nose can be acute and chronic. Vasomotor rhinitis is a variant of chronic runny nose. If an acute runny nose is not treated adequately, it can become chronic. First, nasal breathing becomes difficult, then mucous discharge appears, which can discharge from the nose to the outside or flow down the back wall of the throat, which happens most often.
In terms of symptoms and complaints, vasomotor rhinitis is very similar to allergic rhinitis. Allergic rhinitis is also accompanied by swelling of the nasal mucosa, but this is a seasonal disease, that is, it occurs during the flowering period of plants, or if there is an allergy to house dust, library dust, animal hair, etc.
- Let's talk about the causes of vasomotor rhinitis. Why is it developing?
— There are two main reasons. The first is a consequence of untreated or undertreated acute rhinitis. And in second place is deformation of the nasal septum. If there is an arched curvature of the nasal septum to the left or right, a complex curvature of the so-called S-shape or a single ridge, then the mucous membrane is irritated by the incorrectly moving air flow. The air entering through the nose during normal breathing receives some turbulence. Thanks to this, the air is moistened, warmed, and dust from it settles on the mucous membrane of the nasal cavity. That is, the air enters the lower respiratory tract already warmed, more or less cleared of dust and humidified. And when there is a mechanical reason (deformation of the nasal septum), the air flow changes, thereby irritating the mucous membrane, the nasal turbinates swell, and a picture of vasomotor rhinitis gradually develops.
Read more about a deviated nasal septum in our article: Deviated nasal septum: leave it or fix it?
— What are the symptoms of vasomotor rhinitis?
- First of all, this is difficulty in nasal breathing and mucous secretions that flow down the back wall of the pharynx, as a result of which a picture of pharyngitis develops (inflammation of the back wall of the pharynx). A person complains of a feeling of a lump in the throat, a feeling of viscous mucus that is difficult to cough up. As the patients themselves say when they come for consultations, “a mucus factory”, mucus flows in a stream. These are all signs of vasomotor rhinitis. The sense of smell is also often impaired. Due to swelling of the mucous membrane, the olfactory zone suffers, and the person ceases to perceive odors - either all or selectively.
— How to distinguish vasomotor rhinitis from a common runny nose?
— There is no concept of a “common runny nose.” There is acute and chronic runny nose. If we say that it began suddenly and lasts, let's say, no more than a month, then this may be a condition that is considered an acute runny nose. And there is a runny nose, which becomes chronic.
Chronic rhinitis can be vasomotor and hypertrophic. Stepping back a little, I’ll explain. Each half of the nose has three conchae: inferior, middle and superior. The top one is so small that it is not visible. We see first of all the inferior nasal concha and the middle one (it is smaller in size, but visible). It is the inferior nasal concha that swells, making nasal breathing difficult. Why do nasal breathing difficulties occur? And what is the inferior nasal concha anatomically? It has a small bone base, which is covered with tissue rich in blood vessels. With the slightest inflammatory process (chronic or acute), the vessels in this area dilate, blood flow increases, and the shell swells sharply, increasing in size several times, filling the entire common nasal passage. If this is vasomotor rhinitis, then after instilling any vasoconstrictor drops, the concha contracts, the result is a short-term improvement in nasal breathing. If this is already hypertrophic rhinitis, then the concha does not shrink, remains as large and the nose breathes just as poorly.
— How is the diagnosis of “vasomotor rhinitis” made? What examinations are carried out to identify this pathology?
— First, we base it on the patient’s complaints, which we discussed above. The second is an examination of the nasal cavity. We see swollen inferior turbinates. Usually, irrigation or application (application) of a solution of adrenaline (or xylometazoline-based preparations) is carried out on the mucous membrane. If the shell has shrunk, then the condition corresponds to vasomotor rhinitis. If it has not decreased, it is already hypertrophic rhinitis. There are practically no other diagnostic options.
— Tell us about the methods of treating vasomotor rhinitis in children and adults
“The treatment of this pathology in children and adults is not much different. As a rule, this is, firstly, rinsing the nose with sea water. If it is not possible to irrigate with sea water, then you can use saline solution. What do these solutions do? They wash the mucous membrane, remove excess mucus and force the goblet cells to empty. These are cells that are part of the mucous membrane and produce mucus. They empty themselves, and due to this the mucous membrane contracts somewhat. Nasal breathing improves to a small extent.
After irrigation with sea water, we always recommend using certain hormonal drugs from the group of glucocorticosteroids. They can be used from childhood (from about two years old). Vasoconstrictor drops cause a sharp constriction of blood vessels, and the nose begins to breathe almost immediately. In contrast, a hormonal drug acts slowly, but gives a lasting effect. We do not recommend using vasoconstrictor drops for more than 7 days. At the first stage, this can be done, but if time passes, say, a week is approaching, then in any case the person needs to refuse these drops, replacing them with hormonal drugs.
In some cases, doctors resort to injecting the inferior turbinates with glucocorticosteroids. An injection is made, the tissue is saturated with a medicinal substance, and gradually, during the course of treatment, the shell contracts.
Physical therapy may also be indicated. But this is all conservative treatment. If it is ineffective, we suggest surgical treatment.
— What about traditional medicine? For example, the question is sometimes asked whether herbal treatment for vasomotor rhinitis is effective. What could you say about this?
— You can rinse your nose with a decoction of chamomile, for example, but it is not a panacea. In some cases, you can use some plant-based preparations containing, for example, eucalyptus oil, fir oil. But any oil drops are used for no more than 10–14 days, since they negatively affect the mucous membrane.
— In what cases is surgical treatment necessary? What operations are performed for vasomotor rhinitis and how are they performed?
— Surgical treatment is indicated in one hundred percent of cases when the conservative treatment we discussed is ineffective. How is surgery performed for vasomotor rhinitis?
There are quite a few types of surgical treatment. Firstly, laser destruction is carried out. A special surgical laser pulse strikes certain points of the inferior nasal concha, as a result of which the soft tissue is partially evaporated. As a result of this, the shell contracts.
Another method is ultrasonic disintegration using a special apparatus (it is produced by our industry). The electrode is inserted into the thickness of the inferior nasal concha; against the background of ultrasound, the concha is partially coagulated and partially evaporated.
The third is radio wave surgery. What is now popular and widely used. This is the impact on the sink with a radio knife (non-contact method). Coagulation occurs to some extent and plus evaporation of the soft tissues of the inferior turbinate.
And the fourth type of operation is the so-called lateropexy with vasotomy. How is this operation done? A kind of breaking of the bony base of the concha is performed and it is moved to a lateral position, i.e., from the plane of the nasal septum to the side wall of the nasal cavity. Then a vasotomy is performed: the soft tissue of the inferior turbinate is instrumentally peeled off from the bone base, which leads to a local disruption of the blood supply. Vasotomy is performed to reduce blood flow to the inferior turbinate.
— What could be the consequences if you ignore the symptoms of vasomotor rhinitis or try to treat it yourself?
— With poor nasal breathing, the brain lacks oxygen, which can lead to chronic brain hypoxia. This time. The person begins to snore at night. Because of this, his sleep suffers, and, in addition, snoring can disturb others. That's two. A person's sense of smell suffers. He ceases to perceive smells normally, which will also depress him. That's three.
In addition, with prolonged use of vasoconstrictor drops, the time of their effect is shortened, patients are forced to drip drops more often and increase the dosage. Over time, this leads to atrophy of the nasal mucosa, and the formation of perforation (defect) of the nasal septum is possible. This often manifests itself in the form of characteristic noisy or wheezing breathing through the nose. As perforation increases, deformation of the external nose in the form of subsidence of the nasal dorsum is possible.
What else could it be? Against the background of vasomotor rhinitis, sinusitis, such as sinusitis, frontal sinusitis, and ethmoiditis, can develop with any inflammation.
Read material on the topic:
How to treat sinusitis at home? What will an MRI of the sinuses show?
— Is it possible to get rid of this disease once and for all, or can it periodically bother the patient throughout his life?
— If a person has a deviated nasal septum, the symptoms of vasomotor rhinitis will persist. In such cases, we always tell the patient that it is necessary to undergo septoplasty, i.e. correction of the nasal septum. Then there will be an effect.
If the nasal septum is smooth, then courses of hormonal therapy and irrigation of the nasal mucosa with sea water can be repeated every three to six months. And there comes a time when a person has all the symptoms of vasomotor rhinitis.
If, nevertheless, there are relapses after a short period of time (a period with normal nasal breathing of no more than one month), or the conservative treatment carried out is simply ineffective, then the question of surgery is raised. After surgery, a lasting effect occurs, nasal breathing is restored. But if a person develops an acute runny nose after surgery, and he again did not treat it or treated it incorrectly, then the picture of vasomotor rhinitis may again appear. There are times when it is necessary to operate again.
It is extremely rare that postoperative complications may develop in the form of adhesions in the nasal cavity or perforation of the nasal septum. But this is a very small percentage.
— Oleg Alexandrovich, how to prevent the development of vasomotor rhinitis? Tell us about prevention
— If there is an acute runny nose, it is advisable to contact an ENT doctor so that he can examine the patient and prescribe treatment. In some cases, some drugs are used, in others, others. Treatment should be carried out comprehensively and always under the supervision of an ENT doctor. I repeat that vasoconstrictor drugs can be used for no more than seven days. If the cause of vasomotor rhinitis is a crooked nasal septum, then septoplasty is necessary.
Interviewed by Marina Volovik
The editors recommend:
Autumn ailments: allergic rhinitis in children Can’t breathe! How to treat a runny nose in children? What is ARVI?
For reference:
Golubovsky Oleg Alexandrovich
In 1986 he graduated with honors from the North Ossetian State Medical Institute, in 1988 – clinical residency in otorhinolaryngology. Currently, he is an otolaryngologist in the department of otorhinolaryngology of the National Medical and Surgical Center named after. N.I. Pirogova (Moscow), Associate Professor of the Department of the Institute of Advanced Studies of the National Medical Center, Candidate of Medical Sciences, doctor of the highest qualification category. Reception is conducted at the following addresses: Moscow, st. Nizhnyaya Pervomaiskaya, 65; at the “Clinic Expert” Vladikavkaz, Vladikavkaz, st. Barbashova, 64a (once every two months (by appointment)).
How to help a child
If at an appointment with a pediatrician it becomes clear that the baby has an acute respiratory viral infection due to teething, the doctor will immediately prescribe treatment. To be sure, you can take a blood test, which will show you what needs to be dealt with. Usually the baby is prescribed:
- vasoconstrictor droplets according to age;
- cough syrup with ambroxol to prevent sputum from stagnating;
- cough tablets - usually Septefril or Lizobact in the permitted dosage;
- saline solution for rinsing the nasal passages;
- antipyretic drugs, for example, Analdim suppositories or suspensions - Panadol, Nurofen.
All medications are prescribed by a doctor - self-medication in this case is unacceptable!
If we are not talking about ARVI, but about a normal reaction to teeth, then when the temperature rises, the baby is given antipyretics, and the nose is washed with saline solution. If the baby is too restless, the gums are smeared with a special anesthetic gel.
Snot on your teeth can be either normal or a sign of infection. It is not difficult to determine their nature - there are many signs that signal that a child has become infected with ARVI. If it is an infection, the mother’s task is to follow the pediatrician’s instructions and do the maximum to ensure that he recovers. To prevent the baby from becoming infected with the virus during the teething period, it is necessary to visit crowded places less (especially during epidemics), wash his toys more often, avoid overheating and hypothermia, and rinse his nose.
Treatment of rhinitis in pregnant women
In our clinic, a thorough diagnosis is carried out to exclude diseases similar to rhinitis in terms of symptoms. After the examination, individual treatment is prescribed depending on the severity, severity and indications.
Treatment is complicated by the fact that many drugs can cause contraction of the myometrium and impaired fetal circulation or vasoconstriction with impaired placental function. Therefore, a doctor must prescribe drug therapy; you cannot use the drugs yourself - they can cause disruption of fetal development.
Drugs for the treatment of rhinitis
Drugs to be taken during pregnancy are selected with great care and individually. Pregnant women are not prescribed oral systemic corticosteroids, although their effect on the fetus is not fully understood. In some cases, the doctor prescribes corticosteroids in the form of aerosols. Oral antihistamines are also not prescribed due to the increased risk of embryopathies. The choice of physical treatments is also limited, because most methods negatively affect the development of the fetus.
If you are suffering from rhinitis, headaches or other unpleasant symptoms, we advise you to see a doctor immediately. Timely treatment is the key to the mother’s quality of life, which is very important for bearing a fetus. It also allows you not to miss other more serious diseases that can negatively affect the health of the mother and child.
Important! You should not use medications that were prescribed to you by your doctor before you became pregnant, or medications that were prescribed to someone else.
Rhinitis during pregnancy usually does not pose a threat to either the fetus or the mother, but improper treatment can lead to unpredictable consequences.