Cleft lip and palate: the defect can be corrected
Cleft lip and palate is one of the most common congenital malformations of the upper jaw: it occurs in a third of patients with congenital malformations. In Moscow, 1 in 800 babies are born with this developmental defect.
The anomaly is usually detected by ultrasound in the 1st-2nd trimester of pregnancy. Such news is a huge stress for future parents. But in most cases, thanks to timely and qualified treatment, cosmetic and functional defects in the baby can be eliminated.
At what age is surgical treatment most effective and how a complex anomaly is treated, Elvira Sergeevna Mkrtumyan, a maxillofacial surgeon and plastic surgeon at the Morozov Children's Hospital, told.
What influences the formation of a defect?
The defect is formed in the first two months of the child’s intrauterine development, when the formation of the facial skeleton occurs. The cause of the development of pathology is a chromosome abnormality.
The development of the defect is influenced by both hereditary factors (7%) and external factors (40%). External ones include infectious and viral diseases, smoking, drugs, alcoholism, the use of certain medications, lack of vitamin folic acid, poor ecology, and so on.
What types of clefts are there?
Clefts can occur in both the lips and palate. They, in turn, can be isolated (only the lips or only the palate) and through, when the defect extends to the upper lip, alviolar process and palate. Each type has varying degrees of severity. In addition, the defect can be either unilateral (usually on the left) or bilateral.
With an isolated cleft lip, as a rule, the deformation may be minor, or may be accompanied by deformation of the nasal septum, alar cartilage and alveolar cleft, which subsequently leads to dental problems.
With cleft palates (from minor clefts of the soft palate only to severe bilateral lesions of the soft and hard palates), children may have problems with eating, breathing, sucking, and subsequently with sound pronunciation. Thanks to timely surgical intervention, it is possible to obtain an ideal treatment result.
The most severe form is bilateral through cleft lip and palate. But even in this case, timely treatment and rehabilitation give the baby a chance for recovery.
If, during intrauterine diagnostics, a cleft is discovered in the baby, what should parents do?
The most important thing I would like to say to parents who are faced with this problem is that there is no need to worry. It is important to immediately consult with maxillofacial surgeons involved in the treatment of pathology.
We advise future parents even before the baby is born. We tell you how to feed your child correctly - it is better with a spoon or a bottle with special nipples in order to preserve swallowing reflexes, because with prolonged tube feeding they can fade.
Often this defect can be accompanied by pathology of the bone and cardiovascular systems, kidneys. Therefore, it is important to undergo tests immediately after birth to rule out these diseases. If the baby does not have other serious concomitant diseases, we prescribe planned surgical treatment to eliminate the defect.
At the request of the parents, after the maternity hospital, the child can be transferred to the neonatology department of our hospital, where the mother will be taught how to feed the child, examined and given recommendations for management before a planned operation.
At what age is surgical treatment most effective?
The optimal age for surgery to correct a cleft lip and eliminate nasal deformity, if there is no gross pathology among other systems, is 3 months. Earlier plastic surgeries do not provide the opportunity to obtain the best aesthetic result.
If the child has a severe form of cleft, correction can be carried out in two stages. At six months, if it concerns the palate, it is the soft palate; from one to two years, it is the hard palate. If surgical treatment is carried out in one stage, then it is performed at the age of 9 months to 1.5 years. This has a number of advantages: the child endures one rather than two anesthesia, the tissues are more mature, which means the treatment result will be more effective. We recommend palate plastic surgery for children under two years of age, until the child’s brain—the center of speech—has formed incorrect speech.
If the child has a severe form of cleft, correction can be carried out in two stages. At six months, if it concerns the palate, it is the soft palate; from one to two years, it is the hard palate. If surgical treatment is carried out in one stage, then it is performed at the age of 9 months to 1.5 years. This has a number of advantages: the child endures one rather than two anesthesia, the tissues are more mature, which means the treatment result will be more effective. We recommend palate plastic surgery for children under two years of age, until the child’s brain—the center of speech—has formed incorrect speech.
What operations are performed for cleft lip and palate?
Correction of a congenital anomaly requires an integrated approach. It is aimed not only at eliminating a cosmetic defect, but also at reconstructing functional disorders, eliminating problems with swallowing, breathing and sound pronunciation. The volume and type of operational benefit depends on the characteristics of each child and is selected individually.
If the cleft looks like an isolated lip or palate, surgical treatment will be performed in one stage. In the most difficult cases, correction is carried out in several stages.
For isolated cleft lip without significant deformation of the nose, cheiloplasty is performed. The vestibule of the oral cavity (the space located under the upper lip) is created, the integrity of the orbicularis muscle of the upper lip is restored, and a red border is formed. If the upper lip defect is more severe, then a one-stage cheilorhinoplasty (lip and nose surgery) is performed. We perform lip plastic surgery and place the alar cartilages of the nose in a symmetrical position. On the 7th day, postoperative sutures are removed and the children are discharged from the hospital with recommendations for further management of the child.
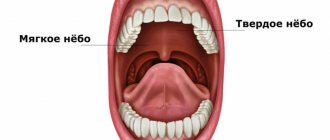
An isolated cleft palate manifests itself as an anatomical damage to the soft palate (mobile palate) or the soft and hard palate. The pathology is accompanied by impaired swallowing, breathing and sound pronunciation. Palate plastic surgery involves restoration of the hard palate and soft tissues of the velum, and closure of the alveolar process. After the operation, when children reach 3 years of age, classes with a speech therapist are recommended to prevent speech disorders, manifested by nasality and unintelligibility of speech.
If speech disorders are not eliminated through the efforts of speech therapists alone, then there is a surgical correction - elimination of velopharyngeal insufficiency. The operation involves transplanting flaps on a pedicle in the area of the pharyngeal ring.
From the age of 5, a child is sent for treatment to an orthodontist to eliminate defects in the dentofacial system. At the end of orthodontic treatment, the next stage of surgical treatment is performed - bone grafting of the alveolar cleft to eliminate the bone defect of the alveolar process.
The Morozov Children's Hospital has accumulated extensive experience in the effective treatment of cleft lip and palate. Every year, doctors perform up to 200 operations to correct these congenital malformations.
Features of caring for a baby with facial clefts
Carefully clean the nose using damp cotton swabs soaked in oil (sterile olive, sea buckthorn) or herbal infusions (chamomile).
With cleft lips and palate, part of the oral mucosa is in constant contact with air. This leads to the formation of cracks and crusts on the mucous membrane of the upper lip. Toilet your upper lip, especially in the cleft area: carefully remove pre-soaked crusts and treat the surface with sterile oil.
When walking in the cold season, use gauze masks on the area of the wide cleft of the upper lip to warm the incoming air.
Risks of the procedure
When performing an operation to restore the soft palate, complications such as complete dehiscence of the suture, slit-like or perforated defects, malocclusion (oblique or mesial bite), immobility of the palate, rough scars, and tissue necrosis are possible. In case of improper care or poor quality of surgery, infectious complications are possible.
When eliminating snoring through conventional surgery, laser therapy or cryotherapy, complications such as loss of function of the soft palate are possible, which may include impaired swallowing and nasal breathing, cicatricial stenosis of the pharynx, nasal speech, and lack of obturator function of the palate. The most modern and safe method of treating snoring is somnoplasty.
How to prepare for the procedure
To perform veloplasty for congenital defects, the patient undergoes clinical and laboratory tests to determine the general health of the body (general blood tests, urine tests, biochemistry, blood clotting, HIV tests, determination of the Rh factor and blood group, immunological blood tests). Impressions and X-rays of the jaw, endoscopy, echography, etc. are made. Before the operation, the child must undergo a consultation with a pediatrician, maxillofacial surgeon, otolaryngologist, orthodontist, speech therapist, anesthesiologist, dental therapist and psychologist.
Preparation for plastic surgery of the soft palate for people suffering from snoring involves conducting general tests and accurately confirming the relationship between night breathing problems and changes in the palate.
results
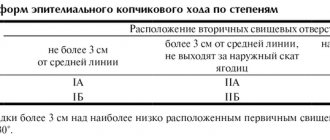
In patients with RHN, elements of bulbar syndrome were most often detected, and somewhat less frequently, pseudobulbar syndrome; signs of brainstem dysfunction were common; signs of dysraphic status, including vertebral anomalies, were often detected (Table 1).
Table 1. Features of the neurological status in patients with RHN
Elements of bulbar syndrome in varying degrees of severity were found in 100% of patients with RHN and had their own characteristics. First of all, attention was drawn to disturbances in the innervation of the tongue (Fig. 1): deviation of the tongue was detected in 13 (61.9%) patients; hypotrophy of the tongue - in 18 (85.7%) patients (central - in 13 (61.9%) patients, regional - in 2 (14.3%), general - in 3 (9.5%) patients); fasciculations and motor restlessness of the tongue - in 5 (23.8%) and 4 (19.0%) patients examined with RGN, respectively.
Rice. 1. Language of a child with RGN.
Sagging of the soft palate and deviation of the uvula of the soft palate (uvula) were noted in 7 (33.3%) patients of the main group. At the same time, swallowing and the pharyngeal reflex were preserved in almost all patients. Only in 1 (4.8%) case were there minor swallowing disorders.
17 (81.0%) patients of the main group had speech disorders: isolated dysarthria - 5 (23.8%), isolated dys- and nasophonia - 3 (14.3%). Severe speech disorders in the form of a complete bulbar speech syndrome - severe dysarthria in combination with disturbances in voice sonority (naso- and dysphonia), as well as with features of the speech flow (slow, less often - 3 (14.3%) cases - scanned speech) were identified in 9 (42.9%) patients. Severe speech disorders were more often noted in younger patients - their average age was 9.9 ± 2.0 years.
Somewhat less frequently in patients with RHN, neurological symptoms were detected from other cranial nerves (III, IV, V, VI, VII pairs): facial innervation - perioral fasciculations - 6 (28.6%), hypomimia - 5 (23.8%) , “fast and furious” facial expressions - 3 (14.3%), facial asymmetry - 2 (9.5%); weakness of the masticatory muscles and/or deviation of the lower jaw were detected in 2 (9.5%); signs of dysfunction of the oculomotor nerves - strabismus and nystagmus - in 3 (14.3%) and 4 (19.0%), respectively. Several patients had sensory organ disorders: congenital hearing loss - 2 (9.5%), congenital progressive myopia - 1 (4.8%).
Disorders of facial innervation were in 2nd place in frequency of occurrence in patients with RHN after elements of bulbar syndrome: in the group as a whole, specific features of facial expressions in the form of hypomimia, less often a kind of “forced” emphasized facial expressions were identified in 7 (33.3%) patients with RGN.
Also, very often in patients with RHN, a static disorder was detected (Fig. 2), mainly from the cervicothoracic spine - 16 (61.9%) of those examined in the main group. In patients of the main group, different shoulder heights were detected - 13 (50.0%) patients, chest asymmetry with unilateral muscle wasting - 3 (14.3%), kyphoscoliosis - 12 (57.1%) patients, limited spinal mobility - 3 (14.3%) patient.
Rice. 2. Disturbance of statics (a variant of the development of the cervicothoracic spine) in a child with RHN.
Manifestations of facial dysraphism were frequent: eye difference - 11 (52.4%) patients, hypo- and hypertelorism - 7 (33.3%) patients, facial asymmetry with underdevelopment of one half of it - 7 (33.3%) patients, various height of the ears - 3 (14.3%) patients.
Thus, it is possible to create a kind of “neurological portrait” of a patient with RGN: specific elements of bulbar syndrome (mainly affecting the tongue muscle), features of facial expressions, facial and spinal (mainly from the cervicothoracic region) dysraphism. As the age of the subjects increased, the severity of dysarthria and brainstem dysfunction (from the III-VII pairs of cranial nerves) decreased, but mild speech disorders (dysphonia and/or nasophonia) persisted even in adult patients. In older patients, vertebral problems (back pain, recurrent radicular syndromes, early degenerative changes in the spine) and signs of autonomic dysfunction came to the fore. For this reason, 6 out of 10 (60%) patients with RHN over 12 years of age were observed by a neurologist.
In addition to the characteristics of cranial innervation, microfocal neurological symptoms were found in 9 (42.9%) patients with RHN. It was predominantly represented by elements of cerebellar syndrome (nystagmus, muscle hypotonia, minimal coordination disorders) - 4 (19.0%) patients, autonomic-vascular disorders in older patients - 5 (23.8%) in patients aged 15-17 years. In 2 (9.5%) elements of akinetic-rigid syndrome were identified.
It is important to note that cognitive impairment was not typical for patients in the main group: signs of mild cognitive impairment (not limiting social adaptation) were detected in only 2 (9.5%) of the examined patients with clefts.
In several patients with RGN, the examination revealed signs of a neurological disease, which required more in-depth additional examination (MRI of the brain and spine, ultrasound examination of the brachiocephalic arteries, consultation with a pediatrician and geneticist). According to such additional examination, carried out in 5 (23.8%) patients of the main group, anomalies in the development of the brain stem and posterior cranial fossa, craniovertebral junction and neural tube were identified, in 2 patients genetically determined diseases were identified: incomplete Dandy-Walker anomaly ( underdevelopment of the cerebellum, expansion of the greater and inferior cerebellar cisterns without signs of hydrocephalus) in the structure of Stickler syndrome - 1 patient; aplasia of the corpus callosum (Fig. 3) and brainstem anomaly in the structure of Mobius syndrome - 1 patient; Chiari malformation type I in combination with characteristics of the vessels of the vertebrobasilar system (kinking syndrome of the basilar artery) - 1 patient; Chiari malformation type II in combination with spina bifida
— 1 patient; 1 patient showed signs of parahypocampal sclerosis with epileptic syndrome (Table 2).
Table 2. Developmental anomalies and diseases of the nervous system in patients with RHN
Rice.
3. MRI picture of aplasia of the corpus callosum in a girl R., 12 years old, with ROP. On sagittal FSE T1WI (a, b) the corpus callosum is not differentiated; attention is drawn to the enlarged foramen of Maugendie (a) with a relatively preserved volume of the cerebellum; its tonsils are slightly lowered (b) - to the entrance to the foramen magnum. In this case, there is a slight widening of the interhemispheric fissure and a typical “butterfly” of the lateral ventricles on FSE T2WI in the coronal projection (c). On axial FSE T1WI (d) and TE2WI (e), FLAIR T2WI (f), instead of the corpus callosum, a slightly widened interhemispheric fissure is visible with a change in the configuration of the ventricles characteristic of aplasia of the corpus callosum. In the control group, signs of bulbar syndrome and disorders of facial innervation were not recorded ( p
<0.001).
Microfocal neurological symptoms of other localization (asymmetry and/or revival of tendon reflexes, mild coordination disorders) were detected significantly ( p
<0.01) less often in controls than in patients with RHN - in 3 (27.3%) of the examined patients.
Signs of spinal dysraphism (different shoulder heights, kyphoscoliosis) were detected in 6 (54.5%) patients in the control group, facial dysraphism (different palpebral fissure heights, facial asymmetry) - in 4 (36.3%), less frequently than in the main group. but without statistically significant differences with it. It is important to note that based on clinical examination, only so-called minor developmental anomalies, often detected in practically healthy people, were recorded. At the same time, relatively gross disturbances in the statics of the cervicothoracic region detected in patients with RHN (underdevelopment of one half of the chest, high grade kyphoscoliosis, fixed torticollis) were not found in the control group.
How does the procedure work?
Palatoplasty to remove clefts is performed using a standard set of surgical instruments. This technology is called Z-plasty or Furlow plastic. It consists of sequentially isolating and stitching triangular flaps of the mucous membranes of the oral and nasal cavities, taking into account all the anatomical features of the structure of these structures. Veloplasty is usually accompanied by other types of surgical operations aimed at the correct formation of the hard palate and lips.
A surgical solution to snoring problems involves the surgeon excision of part of the soft palate and removal of the uvula, but more advanced methods are now being used to solve this problem.
Using a laser after preliminary anesthesia, the doctor makes small wounds, which, as they heal, lift the soft palate. The essence of cryotherapy is exactly the same, except that the operation is performed using a cryoapplicator. Radio wave therapy is the most gentle and effective method. All these procedures usually do not require hospitalization and are carried out within 10-15 minutes. The rehabilitation period is individual.