- Author:
Naumovich Yulia Yakovlevna - Specialty:
Dentist-orthodontist - Category:
Doctor of the highest qualification category
Learn more about the doctor Get a consultation
Cleft palate is a pathology of the hard and soft palate. Occurs in approximately 1 in 1000 newborns (2 times more often in girls) and is often combined with other abnormalities of the jaw formation
SYMPTOMS OF CLEFT PALATE
Symptoms of cleft palate are noticeable immediately upon birth. Breathing in such newborns is difficult, the air does not have time to warm up, so there is a predisposition to respiratory tract diseases. Due to the inability to suck, the baby has to be fed using additional devices. Pathological changes in the maxillofacial apparatus do not allow speech development. As a result of fluid accumulation, otitis media occurs, which can lead to hearing loss. With the appearance of teeth, their curvature, malocclusion, and extra teeth overlapping each other are noted. There is no physical or mental retardation in development, but children experience psychological discomfort and withdraw into themselves.
We know how to cure Cleft Palate
In the near future, a medical coordinator will contact you and advise you on the conditions and cost of treatment, select a doctor and make an appointment for you.
| Make an appointment | Or call us +375 29 699-03-03 +375 33 319-03-03 |
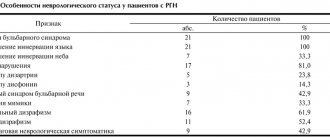
Results and discussion
Considering that this method was used in patients with the most complex forms of the disease, requiring the creation of a large wound defect, we did not have the opportunity to form a control group with conventional wound suturing, which would have been technically impossible. The average duration of surgical intervention was 47.6±9.3 minutes. An uncomplicated course of the early postoperative period with wound healing by primary intention was achieved in 38 (92.7%) patients. In 2 patients, limited suppuration of the wound occurred, which required partial spreading of its edges. Another patient had marginal necrosis of one of the “tops” of the diamond-shaped flap, and therefore the wound healed partially by secondary intention. Long-term results were monitored from 15 to 40 months after surgery. Recurrence of the coccygeal tract occurred in 1 (2.4%) patient and was limited (fistulous tract in one of the edges of the wound). The probable cause of relapse was incomplete radical excision of pathologically altered tissue. Repeated surgery in this patient consisted of excision of the recurrent fistula and suturing of the wound; there was no need for plastic surgery. In all other patients, a strong elastic scar was formed at the lowest “critical point” of the postoperative scar.
After complete wound healing, all patients noted a significant improvement in quality of life. The relocated flap created a load-resistant, full-fledged skin-fat layer that did not cause any inconvenience. Thanks to this type of plastic surgery, an increase in the angle of the intergluteal fold was achieved with a decrease in its depth, although the contour of the fold was always preserved and was not deformed.
The negative side of this method of plastic surgery was the long-term hypoesthesia of the transferred flap, which was observed in 11 (26.3%) patients. Despite the presence of scars extending beyond the sacrococcygeal region, all patients were satisfied with the cosmetic effect of the operation. The likely reason for satisfaction could be the significant predominance of men and the long existence of the disease, and the formation of scars was assessed as an inevitable price to pay for getting rid of a chronic purulent process.
In surgical treatment of the epithelial coccygeal tract, an important requirement is the radical excision of pathologically altered tissues, which are one of the causes of relapse of the disease. Treatment methods with primary restoration of the integrity of the skin have undoubted advantages [6, 9]. This ensures an early return of patients to their usual activities. Conventional wound suturing can be effective in excision of a simple fistula tract. However, with the complex location of the fistula tracts, their branching, the presence of cicatricial and inflammatory-infiltrative changes in the surrounding tissues, especially after previous attempts at surgical treatment, with radical excision quite large wound defects are formed, which cannot be closed by simply bringing the edges of the wounds together. In such situations, wounds can be left completely or partially open with prolonged healing by secondary intention, or closed using plastic movement of the skin, which, in our opinion, is preferable.
In addition, the choice of surgical method is influenced by unfavorable anatomical features such as high buttocks and a narrow deep intergluteal fold, which not only significantly worsen the quality of wound healing, but also lead to an increase in the number of relapses of the disease. Despite the controversial etiology of the epithelial coccygeal tract, almost all coloproctologists note that the most frequent occurrence of relapse of the disease is at the bottom of the intergluteal fold, which requires surgical treatment to make certain adjustments to the spatial structure of the sacrococcygeal region [3, 8].
Plastic surgery according to A.A. Limberg is attracted by the possibility of radical excision of pathologically altered tissues, preliminary planning of the size of the tissue to be moved, and a relatively simple technique. The presence of a wide, well-vascularized pedicle while preserving the subcutaneous tissue, and therefore the superficial and deep cutaneous vascular network, leads to the fact that disruption of the blood supply to the transferred flaps is quite rare [4, 5].
However, the classical implementation of this method leads to the location of the lowest point of the wound at the bottom of the intergluteal fold along the midline. A deep intergluteal fold (especially when the buttocks are closed to each other) creates conditions for the accumulation of skin secretions, skin maceration, and constant bacterial contamination due to poor aeration in this area. These factors have an adverse effect on the nature of healing of wounds located at the bottom of the fold, and also contribute to the penetration of hair into a poorly formed scar and, as a consequence, the occurrence of relapse of the disease [9, 10].
Considering the vulnerability of the symmetrical location of the rhomboid defect, we shifted the position of the “critical point” laterally, moving it from the depths of the intergluteal fold, which eliminates the impact of adverse factors on wound healing. A simple but important detail is the additional fixation of the flap to the bottom of the intergluteal recess, which helps maintain its contour and at the same time corrects the intergluteal angle, and also improves the healing of the flap.
Thus, the use of modified rhomboid plastic surgery according to Limberg in the surgical treatment of common forms of the epithelial coccygeal tract allows for radical excision of pathologically altered tissues with relatively simple skin-plastic closure of the wound defect with good early and long-term results.
TREATMENT
Treatment for cleft palate is only surgical. In early childhood, veloplasty (stitching of the soft palate) is indicated due to the small size of the oral cavity. Further, with the growth and development of the jaws, Limberg uranoplasty is performed. The postoperative regimen recommends careful oral care, eating exclusively pureed food, alkaline drinking, bed rest, and breathing exercises. After two weeks, a set of exercises and massage of the soft palate begin. To exclude postoperative infection, antibiotics are prescribed, and in case of severe pain, analgesics are prescribed.
Material and methods
Believing that the method of completing the operation should be determined depending on the extent of the pathological process, as well as on the individual anatomical features of the sacrococcygeal region, we proposed a classification of fistulous forms of the coccygeal tract according to the degree of complexity (see table). This classification facilitates a differentiated choice of the optimal method of surgical intervention and a comparable comparative analysis of treatment results. In the proposed classification, in addition to assessing the spread of the pathological process, the presence of unfavorable anatomical features of the sacrococcygeal region in the form of the so-called “high” buttocks was taken into account, the criterion of which was the depth of the intergluteal fold of more than 3 cm above the lowest located primary fistula opening with an angle of the intergluteal recess of less than 30 °.
Classification of fistula forms of the epithelial coccygeal tract by degree *The depth of the intergluteal fold is more than 3 cm above the lowest located primary fistula opening with an angle of the intergluteal recess of less than 30°.
This study included the results of treatment of 41 patients with a fistula form of the epithelial coccygeal tract of the III degree, which corresponded to the widespread prevalence of fistulas with external fistula openings outside the internal clivus of the buttocks, the presence of pronounced scars and infiltrates in the circumference of the fistulous tracts. There were 37 men, 4 women. The average age of the patients was 35.6±6.4 years. In 31 (75.6%) patients the disease was regarded as a relapse. Previously, they had made unsuccessful attempts to excise the coccygeal tract. The average duration of the disease was 7.4±2.1 years. The average body mass index of patients was 27.9±3.5 kg/m2. There were no severe concomitant diseases.
All operations were performed as planned in the absence of acute suppurative processes in the area of surgical intervention in the patient's Depage position under spinal anesthesia. After radical excision in one block of all fistula tracts, their external openings, inflammatory infiltrates, cavities and scar tissue, the wound was given a diamond shape (Fig. 1, a). At the same time, we tried to follow the classical recommendations of the ideal ratio of the angles of the rhomboid defect of 60 and 120°, although there were individual deviations depending on the prevalence of the process in the patient.
Rice. 1. Scheme of moving a diamond-shaped skin flap according to Limberg. Explanations in the text.
To replace the wound defect, a diamond-shaped flap was cut out in the adjacent gluteal region (see Fig. 1, a). According to the direction of the transverse axis of the diamond-shaped defect BD, a cut was made along the line DE, from which a cut was made parallel to the face DC along the line EF. The dimensions of the flap corresponded to the wound defect being replaced. This was easily determined by the correspondence of the axial dimensions, as well as the dimensions of the sides, i.e., the lengths of the cuts AB, AD, CD, BD, DF, FE were the same. The flap included the entire thickness of the subcutaneous fat separated from the underlying gluteal fascia. The degree of mobilization of the flap was determined by its free movement onto the wound defect without tension. After moving the flap, its edges were fixed to the edges of the wound defect with double-row sutures (see Fig. 1, b). The maximum tension of the sutures occurred at points F and D, which made it possible to eliminate tissue tension at the peripheral edges of the fixed flap.
Unlike smooth, flat areas of the skin surface, where this method of skin grafting can be easily performed, the sacrococcygeal region has a complex three-dimensional structure, which can directly affect the results of treatment.
Thus, the weak point of the classical Limberg plastic surgery when excision of the coccygeal tract is the location of the lowest part of the rhomboid defect in the depth of the intergluteal fold, which creates the precondition for complicated wound healing, especially in unfavorable anatomical conditions with “high” buttocks, practically closing with each other. It is in this place that a relapse usually occurs. In addition, if the use of the Limberg method on flat areas of the body surface does not require additional fixation of the flap to the underlying tissues, then the complexity of the three-dimensional geometry of the intergluteal region can cause incomplete adherence of the flap to the wound defect and the accumulation of exudate in the subflap space, which impairs the healing of the displaced tissues.
Taking this into account, we use a modified version of Limberg's plasty, the difference of which is the asymmetrical displacement of the lowest part of the excised rhomboid defect from the midline (Fig. 2). As a rule, the displacement was 2 cm. As a result, after moving the flap, the “critical point” of the wound was in the best conditions for healing.
Rice. 2. Scheme of modified Limberg plastic surgery.
The second feature of the modification is suturing the flap behind the subcutaneous tissue to the deepest part of the wound defect, namely to the bottom of the intergluteal fold (especially in its caudal part), for good fixation and to eliminate the possibility of accumulation of wound secretion in this area, which worsens healing conditions. This technique also made it possible to “straighten” the intergluteal angle, reducing the intergluteal depression, thereby leveling the basis for relapses of the disease. Peripheral zones of the subflap space with large defect sizes were drained, drainage tubes were connected to a device for constant evacuation of wound fluid.
Observation program after treatment method
Rehabilitation after plastic surgery usually includes a set of measures aimed at reducing swelling, eliminating hemorrhages, increasing muscle tone, and improving the quality of the skin. Rehabilitation programs should be aimed at improving the health of the body as a whole - its detoxification, improving microcirculation, increasing the intensity of metabolic processes, moisturizing and lifting the skin. On the other hand, they should be aimed at restoring the skin in the surgical area. When drawing up a rehabilitation plan, many factors are taken into account, including the patient’s health and age, the presence of chronic diseases, bad habits and other individual characteristics.