Anatomy, physiology
The periodontium
is a complex organ of the oral cavity surrounding the teeth, formed from specialized tissues. It is located on the jaws and its main functions are to support (support) the teeth and their nutrition and innervation.
Nutrition (trophism) is provided by blood and lymphatic vessels that supply oxygen and metabolic products to the periodontal tissue.
There are four main anatomical and functional elements of the periodontium:
- gum,
- periodontium,
- alveolar bone with periosteum,
- root cement
The gum is a soft tissue - a mucous membrane covering the alveolar processes, with an underlying connective tissue layer.
It contains lymphatic vessels (they are involved in regulating fluid pressure in tissues and protecting against microbial agents).
Through the periodontium - the ligament of the tooth, the latter is fixed in the jaw bone.
Periodontium
(otherwise known as desmodont) is a connective tissue formation surrounding the tooth and located between the root cement and the inner cortical plate of the alveolar bone.
This ligament, consisting of the main substance, fibers and cellular elements, like an elastic gasket, absorbs the load on the tooth, giving it minimal mobility. When periodontal disease and death occur, fusion of the bone with the tooth – ankylosis – can occur.
The next element of the periodontium is cement, which is also a hard tissue covering the root of the tooth. It is formed by collagen fibers directed along the root and an adhesive substance.
Bone
The alveolar process, in which the tooth is strengthened by periodontium, is composed of outer and inner dense plates and a spongy part between them.
Spongy bone consists of trabecular septa, the direction and shape of which is determined by the load on the jaws and teeth, and bone marrow.
Bone tissue contains mainly crystals of hydroxylapatite (inorganic) and small amounts of water and organic substances.
The cellular elements of bone - osteoblasts, osteoclasts and osteocytes, under the influence of the nervous and humoral system, determine changes in the shape, volume and quality of this tissue.
The bone tissue of the alveolar process is covered with a dense connective tissue structure - the periosteum; it, with the vessels located in it, plays a significant role in the blood supply to the bone.
The blood supply provides tissues and anatomical formations with organic and mineral substances.
At the level of the enamel-cement junction (neck of the tooth), an anatomical formation stands out in the marginal part of the gum - a vascular cuff, which, like an elastic band, ensures a tight fit of the gum to the tooth due to hydrostatic pressure.
The main source of blood supply to periodontal tissue is the external carotid artery with the maxillary and mandibular arteries branching from it.
Venules and veins collect blood into the internal jugular vein. The periodontium is innervated by the trigeminal nerve and the superior cervical sympathetic ganglion.
Among others, there is an anatomical formation - the dentogingival junction
. This is the connection between the gum epithelium and the neck of the tooth.
It is physicochemical: molecules of epithelial cells adhere to cement structures through gingival fluid cells.
Gingival fluid produced by periodontal tissue plays the role of a protective barrier against microorganisms through the activity of phagocytes and its chemical properties. It should be noted that the periodontium is washed by saliva. It is secreted by the major and minor salivary glands.
In addition to water (99.42%), saliva contains organic substances, salts and trace elements. Organic substances enter the oral fluid from blood serum and are secreted by the salivary glands and microorganisms present in the mouth.
Of the inorganic substances, calcium phosphate and calcium bicarbonate (they take part in the formation of tartar), phosphate and sodium chloride are important.
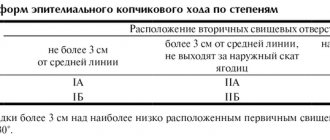
Diagram 1: periodontium
. a – submucosal layer with lymphatic vessels; b — mucous membrane of the attached gum; c - spongy bone of the alveolar process between the plates of the compact substance; d – periodontal fibers are woven into the root cement; e – gingival margin with vessels of the gingival cuff; e – dentogingival junction; g – tooth enamel; h – dental pulp; and – root cement; j – root dentin.
Age-related changes in periodontium
In the periodontium, with age, there is a decrease in the number of collagen fibers and a decrease in their quality. The epithelial layer of the mucosa becomes thinner, and keratinization is disrupted.
The bone tissue of the alveoli becomes less dense, the cortical layer atrophies.
Papillitis
Papillitis is the inflammation of the gingival papilla, which fills the interdental space. Inflammation of the papilla occurs due to exposure to traumatic factors, temperature irritants, viral or bacterial agents, or as a result of an allergic reaction. In rare cases, the cause of the pathology is metabolic disorders, exacerbation of diseases of internal organs, hormonal disorders, etc.
Types and symptoms of the disease
Inflammation can be of several types depending on its course: acute and chronic. The acute form of papillitis is of two types:
Catarrhal - characterized by simple inflammation of tissues;
Ulcerative – accompanied by the formation of small lesions – ulcers, the appearance of acute pain;
Chronic papillitis occurs:
Catarrhal - simple inflammation becomes chronic. It is characterized by hyperemic, bluish papillae, which are slightly enlarged in size. With prolonged existence, resorption of the bone interdental septum is possible;
Ulcerative - characterized by the formation of ulcers and erosions that do not heal for a long period of time;
Hypertrophic - accompanied by the growth of gingival papillae and an increase in their size. In this case, pain may be absent.
Papillitis is manifested by inflammation of one or more interdental papillae on one or both sides of the dentition (internal and external). Symptoms of the disease are redness, swelling of the tissues, an increase in the size of the papilla, pain, discomfort, and unpleasant sensations. The pain may increase while eating. With severe inflammation, the gingival papilla can interfere with the closure of teeth.
Diagnosis and treatment
Diagnosis of the disease is based on clinical examination and patient history. X-ray examination for papillitis is rarely performed, since the disease almost never affects the bone. In some clinical cases, x-rays are necessary to differentiate papillitis from gingivitis and periodontitis.
Treatment is aimed at eliminating the cause of the pathology, healing the gums, and eliminating discomfort. Inflammation of the papilla caused by a household injury or during eating often goes away on its own within 2-5 days. Other types of disease require consultation with a doctor and professional treatment. Therapy includes simple procedures: professional cleaning, medication applications, mouth baths and rinses. Treatment depends on the cause and is selected individually in each specific case. The prognosis for papillitis is favorable, recovery is complete. In difficult cases and in the absence of therapy, inflammation can spread and develop into gingivitis and periodontitis.
Classification of periodontal diseases.
Gingivitis
Gingivitis is an inflammatory superficial disease of the gum tissue.
With gingivitis, there is no disruption of the periodontal junction and bone. Based on the form of manifestation of periodontal disease, the following are distinguished:
- catarrhal gingivitis,
- hypertrophic gingivitis,
- ulcerative gingivitis.
According to the type of course, gingivitis is divided into acute, chronic, aggravated and remission. According to the distribution, gingivitis can be localized and generalized. Without active treatment, gingivitis progresses to periodontitis.
Periodontitis.
Periodontitis is a deep inflammatory disease of the periodontium with destruction of the periodontal junction and bone tissue of the alveoli.
There are acute, chronic course of periodontitis, exacerbation of the disease and remission. Periodontitis can be mild, moderate or severe.
According to the prevalence, this gum disease is divided into generalized and localized periodontitis.
Photo 1. X-ray picture of severe periodontitis. The roots of the teeth are exposed by two-thirds.
2. 1.
Additionally, there is a condition known as
an aggressive form of periodontitis.
This diagnosis can be made by a doctor based on the presence of a set of signs of gum disease. In this case, periodontal destruction is generalized and rapid.
Such periodontitis is typical for ages from adolescence to 35 years. Often the aggressive form of periodontitis is accompanied by gum growth and granulation. During the period of remission, inflammatory manifestations may subside and even disappear.
Periodontal disease
Periodontal disease is a chronic degenerative periodontal disease.
In European and American classification as a separate gum disease
doesn't stand out. Periodontal disease is characterized by a long-term, benign course and almost does not lead to loosening and loss of teeth.
Periodontal diseases - as symptoms of other diseases
There are idiopathic periodontal diseases with progressive destruction of periodontal tissue (periodontal syndrome).
Such conditions can occur when exposed to physical factors (radiation), poisoning, immunodeficiency, diabetes mellitus, eosinophilic granuloma, Papillon-Lefevre syndrome, neutropenia, etc.
Periodontomas. Epulis (epulid) and gingival fibromatosis
Periodontomas are tumors and tumor-like conditions of the gums. The most common of them are epulis (epulid) and gingival fibromatosis.
Gingival fibromatosis is characterized by the proliferation of periodontal tissues, which causes tumor-like damage to the gum tissue. Gingival fibromatosis is most common in adults, but is sometimes diagnosed in children.
The diagnosis of gingival fibromatosis is made by a specialist based on the patient’s complaints, examination data, radiography, and histological examination.
The main reason for the growth of gum tissue, as a rule, is a violation of metabolic processes; drug-induced fibromatosis of the gums is also identified. Treatment of the disease is surgical and consists of excision of the overgrown gum to the periosteum.
Photo 2. Gingival fibromatosis
Treatment at home
Treating gums at home is only possible if simple gingivitis or papillitis occurs. For this purpose, the mouth is rinsed with decoctions of medicinal herbs and a salt-soda solution. It is impossible to treat flux on the gums and other diseases on your own. If any symptoms occur, you should consult a doctor, undergo professional therapy, and follow the instructions of a specialist at home.
The dentist recommends performing the following procedures at home:
Carry out thorough hygienic brushing of teeth;
Rinsing with a salt-soda solution, which is effective against inflammation;
Rinsing with a decoction of medicinal herbs. The decoction has anti-inflammatory, antiseptic, antimicrobial, deodorizing and wound-healing properties;
Apply medications.
Etiology and pathogenesis (causes and development) of periodontal diseases
Calculus
The main point in the development of gum diseases such as gingivitis and periodontitis is dental plaque (plaque), which turns into tartar (calculus).
Photo 3. Soft plaque (plaque). Marginal periodontitis.
It is believed that organic soft dental plaque, which is formed from food debris due to poor hygiene, is gradually saturated with calcium from saliva and serum exudate of the gum pockets and is converted into hard tartar.
The latter can be of different hardness and color, which is determined by its composition. It consists of 18-25% organic matter (microbes and dead cells) and 75-82% inorganic matter (calcium, phosphorus, metal salts).
Tartar causes traumatic compression of the gums and prevents the cleaning of the periodontal pocket, promoting the development of microbial agents.
Microorganisms diffuse deep into periodontal tissues, lingering on the surface of the basement membrane and further into the bone tissue of the alveolar process.
Traumatic closure of teeth
In the absence of part of the teeth, in case of violation of the position of the teeth, in case of partial destruction of teeth and other traumatic factors, the remaining teeth are subjected to excessive and inadequate load. The latter, in turn, destroys the periodontium of the teeth.
Improper functioning of the temporomandibular joint (TMJ).
The ANS may be a significant factor in the development of gum disease.
Treatment
Depending on the cause of the disease, professional therapy includes the following treatment methods:
1. Removal of dental plaque using ultrasound and Air-flow device. This stage of treatment is the main one and is carried out first. Eliminate subgingival and supragingival tartar, plaque, soft and hard plaque, pigmentation;
2. Treatment of a fistula on the gum includes treatment of root canals and elimination of the root cause of the disease. After eliminating inflammation at the root apex, the fistula heals on its own;
3. Treatment of gum inflammation using anti-inflammatory drugs in the form of pastes, gels, solutions;
4. Antiviral agents are used for herpetic tissue damage;
5. Antimicrobial drugs are prescribed for the formation of ulcers, erosions and other elements of lesions on the gums;
6. Wound healing medications are necessary in the presence of ulcers or necrotic changes in the mucous membrane;
7. General restorative therapy includes immunostimulating agents and vitamins;
8. Consultation and treatment with other specialists (general practitioner, endocrinologist, gastroenterologist, etc.).