Bad breath is a delicate and very unpleasant problem, which often interferes with normal communication with others. Most often, the problem of bad breath is associated with dental diseases or poor oral hygiene. But there are a number of ENT reasons that also provoke the appearance of a strong odor. Why does my breath smell? What is the most effective treatment for bad breath? You will find the answer in our new article.
Have you heard of a condition called halitosis? Most likely no. Although, according to medical statistics, a quarter of the adult population is directly faced with this problem. Behind this “strange” diagnosis lies the delicate and unpleasant problem of bad breath.
In many cases, a person gets used to this smell and stops noticing it, and tactful people around them do not want to offend the person. As a result, the patient does not even try to get rid of the problem, although strong bad breath is a symptom of pathological changes in the body.
There are also opposite situations when a person literally “lives” with his unpleasant problem: he masks the bad breath with chewing gum, refreshing sweets or special sprays. But one should not expect a strong effect from these measures. They only help to temporarily hide this deficiency. As a result, the patient becomes so fixated on his problem that he tries to avoid contact with others and spends most of his time alone. But this is a step towards severe depression.
The main thing in solving a problem is not to go to both extremes. It is necessary, first of all, to understand why your breath smells, that is, to establish the causes of the strong odor, and then carry out high-quality treatment.
Treatment of halitosis, like any other disease, must begin with a visit to the doctor. It will be extremely problematic to determine the cause of a strong odor on your own, without the help of a specialist.
The causes and treatment of strong bad breath is the topic of our new article.
Exacerbation of chronic tonsillitis: symptoms
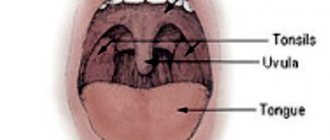
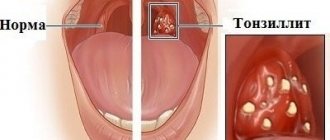
Often, for a long time, chronic tonsillitis occurs without symptoms or has scanty symptoms (in a simple form). There may be discomfort when swallowing food and liquids, a sensation of a foreign body in the throat, dry mouth, halitosis (bad odor) and tingling. Externally, the tonsils increase in size and there are signs of inflammation. The disease is characterized by exacerbations of sore throats up to three times a year, long periods of recovery, with general symptoms of asthenia and prolonged low-grade fever.
For the toxic-allergic form, more frequent exacerbations are typical, often with complications in the area of neighboring tissues (pharyngitis, peritonsillar abscesses), and the almost constant presence of asthenia and prolonged fever are typical.
The clinical picture of chronic tonsillitis during an exacerbation is as follows:
- sore throat that gets worse when swallowing;
- redness of the throat and tonsils;
- characteristic plaque;
- purulent discharge from the tonsils;
- bad breath;
- swelling of the nasopharynx;
- temperature increase;
- weakness;
- headache;
- fast fatiguability;
- arrhythmia;
- enlarged lymph nodes;
- dyspnea.
Categories
AllergistAnesthesiologist-resuscitatorVenereologistGastroenterologistHematologistGeneticGynecologistHomeopathDermatologistPediatric gynecologistPediatric neurologistPediatric urologistPediatric surgeonPediatric endocrinologistNutrologistImmunologistInfectious disease specialistCardiologistCosmetologistSpeech therapistElorologistMammologistMedical lawyerNarcologistNeurologistNeurosurgeon NephrologistNutriciologistOncologistOncourologistOrthopedist-traumatologistOphthalmologistPediatricianPlastic surgeonProctologistPsychiatristPsychologistPulmonologistRheumatologistRadiologistSexologist-AndrologistDentistTherapistTrichologistUrologistPharmacistPhytotherapistPhlebologistSurgeonEndocrinologist
Causes, main risk factors
Up to 30 different colonies of pathogenic microbes can be sown on the surface of the tonsils of patients suffering from chronic tonsillitis. But in crypts and lacunae staphylo- or streptococcus is usually determined. A key role in the pathogenesis of chronic tonsillitis is played by beta-hemolytic strains of streptococcus (type A). Other flora - gram-negative coccal, fungal, viral - have an impact on local immunity, they support inflammation.
There are a number of factors contributing to the occurrence of the disease:
- hypothermia;
- decreased immunity;
- microtrauma of the tonsils;
- foci of inflammation in the mouth and in the head area (caries, sinusitis, adenoids, etc.);
- smoking;
- poor nutrition;
- allergy.
Viruses and bacteria that cause tonsillitis can come from the external environment.
Classification
Doctors distinguish various clinical forms of chronic tonsillitis, differing in clinical manifestations, severity of the condition and prognosis, risk of complications, as well as treatment tactics.
The simple form of chronic tonsillitis is characterized by a predominance of local symptoms. If general manifestations and lymphadenitis occur, this is referred to as a toxic-allergic form of tonsillitis. It comes in two versions:
Toxic-allergic chronic tonsillitis 1st degree . Sore throats are typical for him, which can worsen after ARVI, combined with general symptoms.
Toxic-allergic chronic tonsillitis of the 2nd degree - the symptoms are more pronounced, associated with diseases that have common factors of etiology and pathogenesis.
According to the degree of compensation of the process, the disease is divided into two options:
- chronic tonsillitis, compensated form - the source of infection is in a dormant state, there are no reactions from the body, repeated sore throats do not occur; The function of the tonsils and general reactivity are not impaired.
- chronic tonsillitis is a decompensated form - relapses of sore throat occur, complications of the heart, damage to the paranasal sinuses, middle ear, and renal complications are possible.
According to pathomorphological criteria, the process is divided into the following options:
- lacunar tonsillitis with predominant damage to the area of the lacunae;
- parenchymal-lacunar, involving in addition to the lacunae also the area of the lymphoid tissue of the tonsils themselves;
- phlegmonous - inflammation is predominantly localized in the area of lymphoid tissue;
- sclerotic with abundant growth of connective tissue fibers in the area of the tonsils and surrounding tissue.
How can a doctor help?
Treatment of tonsillitis must be carried out comprehensively. Before prescribing medications, the ENT doctor will remove plugs from the tonsils using a blunt spatula or a special irrigator. This device is intended for washing the affected lacunae with a stream of medicinal solution.
After this, the patient may be prescribed the following treatment:
- Physiotherapy, phonophoresis.
- Rinse with medicinal solutions.
- Antifungal or antibacterial drugs.
If conservative therapy methods do not help, and the inflammation begins to spread to surrounding tissues, the patient is prescribed an emergency surgical operation called tonsillectomy. The tonsil removal procedure is performed under local or general anesthesia.
After the operation, the patient is prescribed a special diet that excludes foods that irritate the operated tissues and slow down their healing process. Also in the postoperative period you should avoid alcohol, taking hot baths and playing sports.
Complications of chronic tonsillitis
Against the background of a chronic inflammatory process in the tonsil area, various complications are possible. Therefore, it is important to know why chronic tonsillitis is dangerous. Thus, the tonsils themselves, losing their function as a barrier to infection, become its breeding ground. Inside them are pathogens with the products of their metabolism. The infection can spread throughout organs and tissues, affecting the renal parenchyma, joint and heart tissue, and liver. In addition, tonsillitis adversely affects the functioning of the immune system and can be a provocateur of collagen diseases - lupus, scleroderma, dermatomyositis, periarteritis. The skin and peripheral nerve fibers may also be affected. With prolonged intoxication against the background of the disease, damage to blood vessels (vasculitis) and platelets (purpura) is possible.
Diagnostics
Diagnosis of chronic tonsillitis occurs on the basis of complaints, examination of the patient, and questioning of the patient. Objective signs, manifestations of chronic tonsillitis, and the general condition of the tonsils are important; the doctor determines the stages of the process and the form.
The following diagnostic procedures are also carried out:
- throat swab for flora;
- general blood and urine tests;
- blood test for antibodies to streptococcus.
This helps determine treatments for chronic tonsillitis.
Why then wash the tonsils?
Usually the reason for washing is the so-called “plugs” or tonsillitis. Among patients and, unfortunately, often among doctors, there is a belief that these “traffic jams” are manifestations of a chronic infection. Sometimes you can hear the term “purulent plugs”. This description is incorrect. Indeed, in the lacunae (pores) of the palatine tonsils, food debris, calcium salts, dead and obsolete cells of the palatine tonsils and bacteria that normally live in the oral cavity sometimes accumulate. Together they form a white conglomerate, usually dense. Tonsilloliths themselves are not a sign of any disease. In the event that they physically interfere with the patient, as a rule, proper independent care of the oral cavity and teeth is sufficient.
Treatment methods in adults
In most cases, they resort to conservative treatment of chronic tonsillitis. Source: Modern methods of treating chronic tonsillitis. Ryazantsev S.V., Eremina N.V., Shcherban K.Yu. Medical Council, 2022. p. 68-72:
- therapy for inflammation in the head and oral cavity;
- procedures that increase immunity (hardening, taking vitamins, physical education, etc.);
- hyposensitizing drugs (to suppress allergic reactions);
- immunomodulators (normalize the immune system);
- means of reflex action (acupuncture, manual therapy);
- washing the tonsils with antiseptics;
- administration of drugs to the tonsils.
The treatment plan is complemented by physical therapy for chronic tonsillitis.
A radical method of treating chronic tonsillitis is surgical removal of the tonsils (tonsillectomy). The operation is performed in cases where inflammation occurs more than five times a year and does not respond to complex conservative treatment of chronic tonsillitis. Source: Choosing an antibiotic for exacerbation of tonsillitis. Karpishchenko S.A., Kolesnikova O.M. Medical Council, 2015. p. 40-43.
Treatment regimen for bad breath, tonsillitis and conclusions
The patient’s main question when contacting her was whether her tonsils need to be removed to solve the problem? When examining the nose, no visible nasal problems were identified. X-ray of the paranasal sinuses was performed without pathology. Consulted with a dentist, the oral cavity was sanitized. The gastroenterologist did not identify any problems with the gastrointestinal tract.
Pharyngoscopy : the pharynx mucosa is pink, the palatine tonsils are not enlarged, the anterior palatine arches are hyperemic. When rotating and pressing on the tonsils, a cheesy discharge emerged from 2 large lacunae, which, according to the patient, had exactly “that smell.”
The treatment regimen I carried out:
- The tonsils were washed with octenisept solution and Triderm ointment was injected into the tonsils for 7 days.
- Phonophoresis was performed on the submandibular region, the area of projection of the palatine tonsils.
- After cleaning the lacunae, a week later radio wave “sealing” of the lacunae was performed using the Surgitron radio wave apparatus. The purpose of the procedure was to exclude gaps from the process of accumulation and production of caseous masses by “gluing” them together.
In some patients, he used other methods: cryolakunotomy - he froze the lacunae, if the size allowed, which led to the expansion of the lacunae, the improvement of the tonsils and subsequently to their self-cleaning. In some cases, the expansion of the outlet of the lacuna was carried out by removing the “interfering” area, which led to the formation of a wide outlet.
Prevention of chronic tonsillitis in adults
Preventive measures to prevent chronic tonsillitis include:
- proper hygiene;
- hardening;
- balanced diet;
- maintaining cleanliness in the home and workplace, eliminating dust;
- timely treatment of inflammationSource: Treatment and prevention of chronic tonsillitis. Atagulova G. Zh. Medicine and ecology, 2012.
Chronic tonsillitis is a very common disease that causes a lot of inconvenience to the patient. But is it possible to cure chronic tonsillitis? If your tonsils often become inflamed, then do not self-medicate, but consult a doctor who will select the optimal treatment regimen for you and determine how to get rid of chronic tonsillitis. You can make an appointment with a medical specialist in St. Petersburg by calling the phone number listed on the website.
Article sources:
- Treatment and prevention of chronic tonsillitis. Atagulova G. Zh. Medicine and ecology, 2012
- Chronic tonsillitis in the practice of an otolaryngologist and cardiologist. Yalymova D.L., Kostyuk V.N., Vishnyakov V.V., Yalymov A.A., Shekhyan G.G., Zadionchenko V.S. Cardio Somatics, 2014. p. 60-65
- Choice of antibiotic for exacerbation of tonsillitis. Karpishchenko S.A., Kolesnikova O.M. Medical Council, 2015. p. 40-43
- Modern methods of treating chronic tonsillitis. Ryazantsev S.V., Eremina N.V., Shcherban K.Yu. Medical Council, 2022. p. 68-72
Cost of treatment
| Name | Cost, rub. | |
| 1 | Initial appointment with a doctor, doctor of medical sciences | 7500* |
| 2 | Procedures included as prescribed by a doctor: | |
| UZIS | 2700 | |
| Ozone ultraviolet sanitation | 450 | |
| Laser photoreactive therapy | 1800-2600 | |
| Application of a microcompress into the nasal cavity | 700 | |
| Application of gum-propolis suspension to mucous membranes | 600 | |
| 3 | Final examination by a doctor based on the results of treatment | 1000 |
* — When paying for the full course of treatment procedures, the cost of a doctor’s appointment is included in the amount of treatment. The course of treatment is prescribed by a doctor. The course duration is 7-12 sessions depending on the diagnosis.