The Greek word "kystis", used to refer to a condition such as a dental cyst, is translated as "blister". This name most accurately reflects the essence of this disease. With it, a cavity is formed at the root of the tooth, which is filled with liquid (bacteria and dead cells), and the comparison with a bubble in this case is most appropriate.
The consequences of untimely treatment of a cyst in the gum of a tooth can be the most unpleasant - including tooth loss. The process may also involve neighboring teeth, which will also require professional dental treatment.
Resection of the root apex (frontal group) - 6,500 rubles.
Resection of the root apex (chewing group) - RUB 9,000.
At CELT you can get advice from a dental specialist.
- The cost of a dental consultation is 1,000
- The cost of an orthodontist consultation is 2,000
Make an appointment
Cyst symptoms
In the initial stages, the cyst is almost invisible. Unlike an abscess, it does not break out, but at the same time continues its development inside, affects healthy tissue of the jaw bone and leads to loosening of the tooth. As the inflammatory process develops, the following symptoms of a cyst in the tooth appear:
- pain in the affected area;
- swelling of the gums;
- increased body temperature;
- swollen and tender lymph nodes;
- flux.
The pathology quickly develops into a chronic stage and is asymptomatic for humans. During an exacerbation, attacks of pain may occur when eating solid foods. Gradually, the tooth enamel becomes gray or yellow, and the tooth shifts. As soon as the immune system fails due to acute respiratory viral infections or exacerbation of chronic diseases, the growth of the cyst accelerates, so the appearance of a fistula, swelling, acute pain, fever and migraine is observed.
Indications
- Bite abnormalities.
- Periodontitis.
- Installation of orthodontic systems.
- Severe deformation of the ligamentous apparatus (tooth loosening).
- Hyperdontia.
Contraindications
- ARVI and weak immunity.
- Chronic and acute forms of diseases of the cardiovascular system.
- Nervous and mental disorders.
- Cancerous tumors.
Why does a cyst appear?
The causes of the appearance of a dental cyst, a photo of which can be seen in this article, are injuries due to mechanical stress or infection, which leads to the development of inflammation of the tissues surrounding the tooth. A tooth inside the gum can be injured under a variety of circumstances, for example, when the tooth is hit or when chewing nuts. As for infection, it can get into the root canal if dental treatment is performed incorrectly, in particular, if the dental canal is incompletely filled. A cyst that arose as a result of sinusitis or another infectious disease is relatively rare. In this case, pathogenic microorganisms enter the gums along with the blood flow.
LifeTime Warranty
The Microscopy Department provides treatment under the LifeTime Warranty format.
We have eliminated possible errors at each stage:
- Endodontic treatment of dental cysts is carried out only using high-precision computer diagnostic
- All work is performed under multiple magnification of a microscope - diagnostics, removal of old fillings, direct treatment and filling of canals, placement of new restorations
- The Center uses of super-tight filling materials from the world “gold standard” line - both for filling canals and for restoring the shape of teeth
When a treatment case is closed, guarantee documents are drawn up confirming the quality of the work performed without complications or relapses. The patient is invited to free annual preventive examinations.
How does the disease develop?
The process begins with periodontitis, when the tissue located between the jaw bone and the tooth root becomes inflamed. As a result, the tissues located around the root begin to grow abnormally. Initially, the size of the neoplasm does not exceed five millimeters (it is called a granuloma). Growing and enlarging, it becomes covered with a membrane and transforms into a cyst.
There are cases when the cyst grows so much that it eats away the bone around the tooth. With the next exacerbation of inflammation, it opens, forming a channel to the outside through the gum mucosa. Such a channel is called a fistula or fistula tract.
It is worth noting once again the insidiousness of this disease, which not only negatively affects the condition of the roots of the teeth, but also affects the general condition of a person. At the initial stage, the pathology develops almost imperceptibly and can only be detected during a visit to the dentist. Pronounced symptoms appear in the later stages of the disease as a result of tumor growth and destruction of bone tissue.
The main danger of a cyst is the fact that, by corroding the bone, it deprives the patient of the opportunity to install an implant in place of a lost tooth without complex manipulations.
Methods of surgical solution to the problem
There are various techniques for eliminating a cyst. The dentist decides which one is most appropriate.
- The distomy method involves resection of part of the cyst. This is the most effective method for the formation of a large cyst. It is partially removed. An obturator is left in place, which prevents the cystic tissue from fusing together. After some time, epithelial layers will cover the remaining parts of the cyst and make it safe.
- When using the cystectomy method, healthy dental tissue is completely preserved. The doctor will open the cyst, pump out the fluid from it, treat the root and gum with antiseptics and then apply stitches. In the process of fairly rapid growth of bone tissue, the emptied cyst disappears. The entire procedure takes place within half an hour.
- During hemisection, the cyst is removed from the gum and root. The surgeon will excise the root with the coronal part. To eliminate damage and restore the dentition, crowns or dentures are placed. This method is used when it is impossible to save a damaged root.
- The most modern, safest method is laser removal. This is a painless and almost bloodless procedure. It does not pose a threat of infection and has a short recovery period.
The dentist selects removal options based on the examination results. All pain is eliminated by the use of local anesthesia.
Removal of a dental cyst at the “One to One” clinic
What complications does a dental cyst lead to?
Untimely treatment or removal will lead to the following complications:
- Periostitis.
- Swelling.
- Abscess.
- Phlegmon.
- Temperature increase.
Usually the cyst does not make itself felt in any way, so complications may appear unexpectedly. To exclude serious consequences, you need to be examined by a dentist at least once every six months. The appearance of a capsule with pus can occur against the background of deep caries or severe inflammation of the gums, so do not delay a visit to a specialist.
The lack of results with conservative treatment leads to the fact that the cyst has to be removed along with the tooth.
Types of dental cyst
The type depends on the place of occurrence. A cyst forms in the maxillary sinus, gum, root or under the crown. To determine the type of capsule with pus, the specialist examines the medical history and assesses the client’s general health. There are 5 types of dental cysts:
- Follicular - formed when the tooth was unable to grow unhindered and most of it remained inside.
- Keratocyst - develops against the background of pathological processes during the growth of the body (the growth of the neoplasm is stimulated by the pharynx-forming tissue).
- Radicular - appears from a granuloma and is a serious complication of deep caries.
- Retention – is formed during the eruption of molars in children.
- Residual – appears due to complications and inflammatory processes after tooth extraction.
What does the cost consist of?
The cost of cyst treatment depends on the number of infected canals and the severity of the situation.
The standard cost of treatment includes the following items:
- x-ray examination
- diagnostic examination under a microscope
- mechanical and medicinal treatment of canals
- temporary filling with medicinal pastes
- 3D canal filling
- restoration of tooth shape using filling materials
By default the price includes:
- consultation with doctors
- local anesthesia
- using a microscope
- use of rubber dam and optagrate
Additional events:
- unsealing of canals filled with resorcinol-formalin method or cement
- removing a pin or foreign body from the canal
- treatment with sedation
- restoration of tooth shape using orthopedic structures
Please understand that the final cost of treatment for a dental cyst is difficult to predict in advance without an in-person visit and examination. Only after X-ray diagnostics and examination of the tooth under a microscope can a treatment plan be drawn up, the number of visits determined and an estimate generated.
Cyst on the root of a tooth
This species grows in the alveolar area and can appear in any area of the gum. There are no symptoms except for tingling when eating or touching. Pain appears in later stages of development. A cyst on the root of a tooth is divided into 3 types:
- Peri-root - appears in the upper part of the root.
- Interroot – formed between the roots.
- Radical - appears near the root canal and over time can cause the growth of a malignant tumor of the jaw (if not properly treated).
Conservative and surgical treatment of cysts
In the early stages, in the absence of complications, a conservative method is acceptable. The root canal is drilled and cleaned. The capsule with pus is opened and cleaned, and a composition with an antibiotic is poured inside. Next, a bone tissue regeneration paste is applied and a filling is installed. A control check after 6 months demonstrates the absence of a cyst on an x-ray in 80% of cases
Surgical treatment is prescribed if there is no result. With the help of cystectomy, the affected part of the tooth and the capsule with pus are completely removed. Cystectomy is an operation that not all dental surgeons can do. Hemisection is often used, which gives a 100% result and is prescribed for severe root damage. All affected tissue is removed, and the appearance of the tooth is restored with a crown or composite composition.
Malignant degeneration of odontogenic cyst within 10 years
Primary intraosseous cell carcinoma of the jaw is an aggressive malignant tumor that develops primarily from odontogenic epithelium. These carcinomas can be quite aggressive and can involve large areas of the jaw. External signs are not specific, and the diagnosis can only be confirmed by a biopsy. The two- to six-year survival rate is approximately 53%, and recurrence becomes a major problem in the absence of radical excision.
Malignant degeneration of odontogenic cysts occurs in approximately 0.13% - 2% of cases, with most pathologies occurring in the lower jaw.
The purpose of this article is to present a description of an intraosseous carcinoma likely arising from an odontogenic cyst.
Clinical case
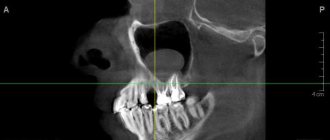
A 44-year-old man presented to the cancer center for treatment of a jaw tumor. From the medical history, in 1994 the patient underwent an x-ray examination of an impacted lower left third molar, around which a vacuum consistent with a follicular cyst was detected (Photo 1a). No symptoms appeared, so the patient and dentist decided to continue observation. After 11 years, the man developed pain in the causative area, after which the cyst and two teeth were removed. After 15 days (Photos 1b and 1c), the patient continued to experience pain, and OPTG showed the removal site with no signs of malignancy. A biopsy confirmed the diagnosis of carcinoma.
Figure 1: (a) Spot X-ray shows vacuum around the crown of the left third molar consistent with a follicular cyst. (bc) OPTG performed 15 days after removal showed the site of removal and no signs of malignant transformation.
Treatment consisted of partial manbulectomy with disarticulation and left supramyohyodine cervical dissection followed by microsurgical reconstruction using the fibula (Figure 2). Histopathological analysis confirmed intraosseous carcinoma with regional metastasis to one (level Ib) of 36 lymph nodes without capsular perforation (Photos 3a and 3b). Immunohistochemical analysis with cytokeratins 5 and 14 was performed on a sample of the primary tumor and lymph node, and in both cases the result was positive (Photo 3c-3f).
Figure 2: OPTG performed immediately after surgery. Reconstruction was performed using the fibula.
Figure 3: (a) Islands of cell carcinoma infiltrating bone trabeculae. (b) Regional metastases (NOT 200x). (c) CK5 immunohistochemical analysis in the primary tumor (d) CK5 in regional metastases (e) CK14 in the primary tumor (f) CK14 in regional metastases
Adjuvant treatment included radiotherapy (total dose 64.4 Gy) and cycles of cisplatin (100 mg/m2 every 21 days). The patient was followed up for 8 years after surgery with no recurrence (Figure 4).
Figure 4: CT scan performed 8 years after surgery (a) 3D reconstruction shows bony consolidation between the mandible and the fibula. (bc) Axial CT slices showing no recurrence
Discussion
Primary intraosseous cell carcinoma is very rare, and to make a correct diagnosis it is necessary to exclude the possibility of mucosal carcinoma, other types of odontogenic carcinomas and metastases. This clinical case clearly demonstrates an intraosseous lesion that arose from a follicular cyst 11 years later.
In most cases, the pathology involves the lower jaw, which leads to swelling, pain and paresthesia of the lower lip. The main complaint in this case was pain, which arose only 11 years after the detection of a follicular cyst on a targeted X-ray. Radiographically, carcinoma may appear as a single-cavitated or multi-cavitated formation, weakly or well demarcated with loose edges. In our clinical case, the lesion was single-banded and well-circumscribed, resembling a follicular cyst, which did not raise suspicion of malignancy.
It is a generally accepted fact that odontogenic epithelium of cysts and benign tumors can undergo malignant transformation, including the islets of malasse and the dental lamina. However, the mechanism of this process remains unclear, such cases are very rare and practically undocumented, and many aspects are still controversial. If possible, it is always necessary to identify the benign source of the resulting tumor. Unfortunately, the extracted tooth and surrounding tissue were not sent for histological examination, which is a very common case.
A wide variety of odontogenic cysts are associated with carcinoma, including residual cyst, follicular cyst, odontogenic keratocyst, calcified odontogenic cyst, and lateral periodontal cyst. In an analysis of 116 cases of carcinoma arising from an odontogenic cyst, the most common source was residual/radicular (70 cases), followed by follicular (19 cases), keratocyst (16 cases), 1 case of lateral periodontal, and 9 unclassified. Identification of a benign epithelial lining of an odontogenic cyst may characterize the carcinoma as type 1 (ex-odontogenic cyst). Unfortunately, we were unable to prove the presence of type 1 carcinoma due to lack of material, so the described tumor was classified as type 3 carcinoma (arising de novo).
Studies with cytokines in developing tooth germs may be useful for understanding the histogenesis of either odontogenic cysts or benign and malignant tumors. CK 5,7,8,14 and 19 appear in the enamel organ, CK 14 is the main intermediate filament of the dental plate, reduced enamel epithelium and enamel organ. However, these MC findings may also be characteristic of other epithelia, including the oral mucosa. In order to confirm the odontogenic nature of the formation, we conducted a test with CK 5 and 14, and both cytokines showed immunoreactivity in both the primary tumor and metastases. These data support the hypothesis of malignant transformation of the follicular cyst.
Metastases to the cervical lymph nodes are observed in 50% of carcinoma cases. They can also spread along the inferior alveolar nerve, usually requiring radical treatment to control the disease. Adjuvant radiotherapy may be indicated depending on the extent of the tumor and the extent of regional lymph node involvement. In the described clinical case, the lymph nodes were involved in the pathology. However, mortality from the disease is often associated with the main tumor rather than metastases. According to Thomas (2000), survival rates during the first three years are 75.7%, 62.1% and 37.8%, respectively, for each year, which shows a rather poor prognosis and the need for timely adequate treatment. Our patient underwent left hemimandibulectomy, suprahomiodial cervical dissection, followed by fibular reconstruction and adjuvant radiotherapy and chemotherapy. The patient was observed for 8 years, no signs of relapse were found. In summary, we described a case of possible malignancy of a follicular cyst after 11 years. Despite the fact that most odontogenic lesions are benign, all clinicians should be oncologically alert. Carcinomas often cause severe pain, involving large volumes of jaw bone tissue in the pathology, and early diagnosis of the disease is very difficult due to the lack of specific radiological signs.
This case also illustrates the importance of careful examination and regular follow-up of patients with impacted teeth associated with bone loss. In addition, to confirm the clinical diagnosis and determine the likelihood of malignant transformation of the odontogenic cyst or pericoronal tissues, we recommend performing histopathological examination.
Authors: Juliane Piragine Araujo, Luiz Paulo Kowalski, Monica Lucia Rodrigues, Oslei Paes de Almeida, Clovis Antonio Lopes Pinto, Fabio Abreu Alves