What is a tooth fracture? This is damage to the integrity of the anatomical structure of the tooth. The supragingival or subgingival part of the tooth may break (break or chip), damaging dentin, cement or enamel. Most often, a tooth fracture occurs due to blows or falls, with damage to the face. Less often, this occurs due to the inclusion of small solid objects in food (small pebbles in buckwheat or rice).
Classification
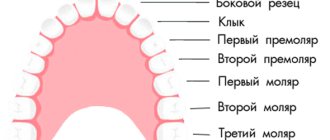
Depending on the part of the tooth in which the fracture occurred, there are:
- tooth root fracture
- fracture of the coronal part of the tooth exposing the pulp
- fracture of the coronal part of the tooth without exposing the pulp
Symptoms
When a tooth root is fractured, a sharp pain occurs when touching the tooth, the crown part of the tooth becomes mobile, the final diagnosis is made after a targeted x-ray. If there is a fracture of the coronal (visible) part of the tooth with exposure of the pulp, then the tooth becomes sensitive to thermal and chemical stimuli, but the tooth is motionless. When a tooth is fractured without exposing the pulp, an aesthetic defect in the tooth crown occurs; the tooth is stable and does not respond to cold or heat.
Treatment method
If the root is fractured in the area of the tooth neck, at the gum level, the root canals of the tooth are filled, then a stump inlay and then a metal-ceramic crown are installed in the root of the tooth. If the root fracture passes below the neck of the tooth, then the entire tooth is removed.
Deputy Chief physician Sergey Evgenievich Brodsky
Sign up for a free consultation
+7
When the coronal part of a tooth is broken off with exposure of the pulp, the tooth is depulped and the tooth is subsequently restored with composite fillings or ceramic inlays. When, as a result of a fracture of the coronal part of the tooth, the dental pulp is not exposed, the tooth is restored with ceramic inlays or composite restorations.
Just CALL US!
+7
We will answer any of your questions and will definitely help you!
Causes
There are several reasons for the occurrence of tooth crown fractures. They are caused by:
- habit of biting pens, opening bottles with teeth, etc.,
- regular consumption of very solid foods - nuts, crackers,
- temperature fluctuations - alternation of hot and very cold food,
- the presence of large fillings that do not have support,
- piercing of soft tissues of the oral cavity - tongue, cheeks, lips.
The combination of several risk factors increases the likelihood of tooth cracking. To notice damage in time, you need to undergo regular dental checkups.
Contraindications for tooth root resection
The operation of resection of the apex of the tooth root is not performed:
- If the patient has a disease such as periodontal disease, which has led to exposure of the neck or root of the tooth;
- If severe tooth mobility is detected;
- For acute periodontitis;
- In case of severe destruction of a diseased tooth;
- In case of an inflammatory process that has damaged most of the root system of the tooth.
The operation of tooth root resection is not prescribed for patients suffering from severe pathologies of the cardiovascular system; other surgical techniques are chosen to remove cysts and granulomas larger than 10 millimeters in size.
Before such a serious and complex operation as resection of the apex of a tooth root, a thorough and high-quality diagnosis is essential, helping to eliminate all possible contraindications to the technique. In our dentistry "Firadent", the highest attention is always paid to the quality of patient diagnostics; all activities are carried out using modern and ultra-precise equipment.
Resection of the apex of the tooth root is an operation carried out in four successive stages, and below we will tell you in detail about all stages of the treatment process.
Manifestations
In most cases, cracks on the tooth form gradually and at the first stage are very small in size. Violation of the integrity of the crown may be indicated by:
- hypersensitivity when eating hot and cold foods - coffee, tea, ice cream,
- discomfort when leaving a warm room into the cold,
- pain during chewing.
If these signs appear, you should not postpone a visit to a specialist. The sooner a fracture is detected, the easier it is to solve the problem and maintain dental health.
What to do after tooth extraction?
Basic recommendations after removal:
- refrain from eating for 2-3 hours after removal;
- do not take a sauna on the day of surgery;
- do not touch the hole with your tongue or any objects;
- do not eat hot food;
- You should brush your teeth the day after surgery.
Some deterioration in well-being and dizziness after the procedure are usually caused by a general stressful state of the body. A walk in the fresh air and a restful sleep for eight to nine hours will relieve you of these unpleasant sensations.
Diagnostic and treatment methods
To detect tooth crown fractures and determine their sizes, several methods are used:
- visual inspection,
- coating of enamel with dyes,
- drying of the tooth
- radiography,
- if necessary - CT.
Based on the examination results, the doctor chooses a treatment method. The choice depends on the location and depth of the crack.
- The enamel structures are covered with a composite material.
- If the crack affects the dentin, the tooth is restored. If the pulp is damaged, endodontic treatment is required.
- A large defect needs excision. The damaged tissue is removed, the tooth is prepared and covered with a crown. It is possible to install a pin.
If the fracture affects the bottom of the pulp chamber, the tooth cannot be saved. The damage in this case is accompanied by pulpitis and periodontitis. The problem can be solved by planned tooth extraction followed by prosthetics or implantation.
Vertical Root Fracture
Vertical root fracture (VRF) is a longitudinal fracture of the tooth root, which, as a rule, starts from the inner wall of the root canal and continues to the outer surface of the root. In this case, both both root surfaces and one can be involved in the process (photo 2). This complication is not as rare as it might seem at first glance. In Mortis' study, vertical root fractures were found in 3.7% of 460 endodontically treated teeth.
Alexey Bolyachin, private endodontic practice (Moscow, Russian Federation)
There is often confusion among clinicians and a vertical root fracture is mistaken for a “cracked tooth” or “split tooth”*. This can lead to misunderstandings between different specialists, and sometimes between the dentist and the patient, who is given a too optimistic or, on the contrary, too depressing prognosis.
* split tooth - split tooth or longitudinal fracture of a tooth
cracked tooth - cracked tooth
Classification of tooth cracks
The modern classification of tooth cracks is as follows:
- Enamel crack.
- Lumpy crack.
- Cracked tooth.
- Chipped tooth.
- Vertical root crack.
cracked tooth
A cracked tooth (cracked tooth syndrome) is a pathology characterized by the presence of a crack, which always begins within the coronal part of the tooth and spreads in the anteroposterior direction (photo 1). Although this is an incomplete fracture (greenstick fracture), it tends to extend deeper into the tooth and more apically, often resulting in root involvement and fracture of the tooth (Figure 3). This condition is sometimes called a longitudinal root fracture. In any case, it must be distinguished from a vertical root fracture (fracture).
Photo 1. Cracked tooth. Mesio-distal propagation of the crack. In this case, the root may not be affected
As a rule, vertical root fracture is a consequence of endodontic treatment, although cases of its occurrence in intact teeth have been described (Shu-Feng Yang et al.). Diagnosis of vertical root fractures is difficult, especially at an early stage, and the detection of this pathology often comes as a surprise to both the dentist and the patient.
Thames et al examined 92 teeth that had been extracted due to apical periodontitis and were diagnosed with vertical root fractures after extraction. The difference in the accuracy of diagnosis performed by a general dentist and an endodontist is shown. When treated by a general dentist, 66% of all cases diagnosed with vertical root fracture were missed or misdiagnosed.
The complexity of diagnosis is explained by the fact that with vertical root fractures, the complaints, clinical and radiological picture are similar to those with periodontal diseases and apical periodontitis (Tems et al.). Sometimes incorrect diagnosis causes repeated endodontic treatment, which is absolutely useless and leads to failure. And only if enough time has passed since the occurrence of a crack or fracture, a typical X-ray picture appears, although the prognosis is already unfavorable.
Causes of vertical root fracture
Among the etiological factors of vertical root fracture are the following:
- Tooth injury.
- Thinning of dentin during endodontic treatment or during preparation of the root canal for a post or investment, which significantly reduces the strength characteristics of the root.
- Inadequate (excessive) force applied to the spreader or plugger during compaction of gutta-percha.
- Inadequate (excessive) force applied to the endocanal structure (pin, inlay) during fixation in the root canal.
The most frequently affected vertical root fractures are the second upper premolars and the anterior roots of the lower molars: from 81 to 84% of all teeth. This fact was explained by laboratory studies by Rosen et al. The researchers found that one of the underlying factors was the small mesio-distal size of the root. Premolars, the anterior roots of the lower molars, and the medial buccal roots of the upper molars have these characteristics.
Fuss et al., analyzing the causes of vertical root fractures in 154 teeth that underwent endodontic treatment, showed that 95 (61.7%) of them were restored with active, screw-in Dentatus-type pins. Apparently, the depth to which the structure is fixed also matters. In 66 cases, the pin ended in the ostial third of the root canal, which created additional lateral load. Similar data were obtained by Sorens et al., Torbjorner et al., which leads to the conclusion that long pins are more preferable than short ones.
Photo 2. a) Tooth 23. A crack extending in the anteroposterior direction, which is not entirely typical for a vertical root fracture; b) both root surfaces are involved in the process. Regeneration in this case is impossible; c) the crack is painted with a caries marker based on propylene glycol
A more important factor is the force applied during installation and cementation of the post. Thames investigated the iatrogenic causes of vertical root fractures, which resulted in the conclusion that excessive force and pressure on the structure during its installation is one of the causes of complications.
Photo 3. a) Tooth 15. At the time of treatment, the patient complained of pain when biting; b) after removal of the restoration; c) a chipped tooth, or a longitudinal fracture of a tooth. Complete divergence of fragments of the coronal part and root.
The time elapsed from the moment of treatment or retreatment until the appearance of signs and symptoms leading to tooth extraction should also be taken into account. According to Fuss et al., 50% of teeth are removed within 1 to 5 years after endodontic treatment or retreatment. 18.8% of teeth were extracted within the first year, and after 5 years 28.5% of teeth were extracted. This differs from the data obtained by Testor et al., who examined 36 teeth extracted due to the presence of vertical root fractures. On average, 10 years passed from the moment of treatment to the moment of diagnosis. The time factor must be taken into account, since the prognosis of subsequent treatment will also depend on the amount of bone tissue remaining after the removal of a tooth with vertical root fracture. The more time passes from the moment the crack occurs until the tooth is removed, the more pronounced the bone destruction is, which can negatively affect subsequent prosthetics.
In addition, it was noted that vertical root fractures most often occur in patients aged 45 to 60 years. In the study by Gehr et al.3 the mean age of the patients was 40–50 years. In our practice, we have encountered younger patients.
Does the type of final restoration and the time of crowning a tooth affect the occurrence of vertical root fractures?
No relationship was found between the time elapsed from the final restoration (covering the tooth with a crown) and its removal (Fuss et al. Thames et al. Wiethe). Therefore, capping a tooth or performing another indirect restoration does not prevent the occurrence of vertical root fractures, since the crack occurs at an earlier stage.
Another factor leading to the occurrence of vertical root fractures is excessive (inappropriate) force applied to the spreader or plugger during gutta-percha condensation. The mechanism of force distribution during gutta-percha condensation was described in detail by Pitts et al. Their studies showed that a force of 7.2 kg was required to produce vertical root fractures of the upper central incisor. The less massive the root, the less force causes a root crack. In a pilot study by Holcomb et al.5, 13% of all fractures occurred with a force of less than 3.5 kg. Meister et al. showed that the cause of vertical root fractures in 32 teeth they studied was in 84% of cases due to excessive force applied to the spreader during lateral condensation.
But how can a clinician evaluate this during work? Harvey et al showed that the average force used during lateral condensation by 8 endodontists ranged from 1 to 3 kg. Does this provide evidence that lateral condensation is a predisposing factor in the occurrence of vertical root fractures?
The type of spreader used is of great importance. Steel tools are more rigid than nickel-titanium tools (photo 4), and as the tool size increases, its rigidity increases. The use of manual spreaders, which create excessive stress during condensation, should be completely avoided. Finger nickel-titanium spreaders have an undoubted advantage and are more preferable than others. This difference is especially pronounced when working in curved canals.
Photo 4. a) Finger nickel titanium and steel spreader, b) with the same diameter and taper, the steel spreader (right) is more rigid
To advance the N&T spreader to a length shorter than the working one by 3 mm, it is necessary to apply a force of 1.6 kg. To insert a steel tool at the same length - 2.4 kg (Smidt et al.). Similar results were recently reported by Peele et al.
Therefore, it cannot be stated with certainty whether lateral condensation is a predisposing factor or not. But this factor will definitely work in the presence of other additional factors.
A very important point is the thickness of the dentin remaining after preparation and especially the local, uneven thinning of one of the root walls (photo 5). Wilcox et al. determined the effect of residual dentin thickness on the occurrence of vertical root fractures in maxillary incisors at a spreader load of 3.3 kg. When the dentin thinned by 20-30% of the original thickness, no fracture occurred. A 40% loss of dentin caused vertical root fractures in 5 incisors, and a 50% loss in 7 incisors.
Complaints and diagnosis
A patient with vertical root fracture may complain of discomfort and pain when biting, swelling, the presence of a fistula, and slight tooth mobility.
If a fracture occurs during compaction of gutta-percha, the dentist will usually hear a characteristic click, which may be accompanied by pain despite anesthesia. This sound should be distinguished from the sound that occurs when the spreader jumps off a ledge or any irregularity on the wall of the root canal. At this point, blood may appear from the mouth of the root canal or on the spreader, and the number of additional gutta-percha points introduced increases. If radiography is performed at this stage, then, as a rule, no changes are detected.
Photo 5. Significant loss of dentin during the preparation process may be one of the reasons for vertical root fracture
Fig. 1. Diagram of the formation of a periodontal pocket during periodontitis (a) and vertical root fracture (b). With periodontitis, the periodontal pocket is wide and shallow. With vertical root fracture, it is narrow and deep. c,d). Typical x-ray picture. Destruction spreading along the root surface
When making a diagnosis, the 3 most characteristic signs should be taken into account:
- isolated (narrow) periodontal pocket;
- coronally located fistula tract;
- characteristic (in the form of a halo) destruction of bone tissue on an x-ray.
The pathogenesis of a vertical root fracture has been described in detail by Welton et al. It has been shown that the destruction of periodontal tissue and bone and the formation of a periodontal pocket are caused by the release of microorganisms along the entire line of the crack or fracture, which explains the characteristic clinical picture (Fig. 1).
The periodontal pocket with vertical root fracture differs from that with periodontal diseases. It occurs quite often - according to Tems et al. in 67% of cases. As a rule, the periodontal pocket is deep and narrow, that is, when probing the dentogingival groove a little distal or mesial, the pathology is not determined (photo 6). The average width is from 1 to 2 mm. The periodontal pocket can be located both vestibular and oral, and sometimes on both sides.
The next characteristic feature is a fistulous tract, which, unlike the fistulous tract in apical periodontitis, is located close to the gingival margin (photo 7). According to Temse et al., a fistulous tract located close to the crown of the tooth occurs in 35% of cases.
An additional diagnostic method is radiography. If radiography is carried out immediately after the occurrence of a vertical root fracture (appearing, for example, during the process of obturation), then radiological signs of fracture are usually absent. Sometimes you can find a shadow running parallel to the filling material, or, even more rarely, an atypical exit of the sealer onto the lateral surface of the root.
Photo 6. Examination of the periodontal pocket of tooth 36 with a diagnosis of vertical root fracture using a probe: a) normal depth; b) moving the instrument a few millimeters distally allows one to detect a narrow (1 mm) and deep periodontal pocket; c) normal depth
Photo 7. Tooth 23. Gutta-percha introduced into the coronally located fistulous tract.
Photo 8. a, b) X-ray picture with significant displacement of fragments.
Photo 9. Tooth 23. Vertical fracture was diagnosed. Involvement of the coronal part of the root in the process led to vertical loss of alveolar bone tissue. Gutta-percha is introduced into the coronally located fistula tract.
If there is a significant discrepancy between the two root segments, the x-ray picture is obvious and there are no difficulties in making a diagnosis (photo 8). According to Meister et al., fragment displacement occurs in only 3% of cases.
When the pathological process involves the coronal portion of the root, it leads to bone loss similar to that of periodontitis and a similar appearance on radiographs (Figure 9).
Most often, bone destruction occurs in the form of a halo or extending along the root surface (photo 10).
If a significant amount of time has passed since the onset of vertical root fracture, the rarefaction resembles a “pear” in shape (Fig. 2). In 12% of cases, there are no radiological signs (Temse et al.).
Figure 2. Pear-shaped bone destruction
Thus, when making a diagnosis and when planning restoration, all signs should be taken into account and caution should be exercised.
The majority of all fractures are complete fractures, that is, those that extend from one root surface to another. Recovery is impossible regardless of the type of treatment (Welton et al., 1984). In cases of single-rooted teeth, tooth extraction is indicated when the diagnosis is confirmed. In the upper molars, root amputation is performed, in the lower molars - hemisection, provided that the coronal part is not involved in the process.
Conclusion
Pin structures do not strengthen the tooth root. On the contrary, preparing the canal for fixing an inlay or pin weakens the tooth tissue, and errors in their installation can themselves cause vertical root fractures.
Photo 10. a, b) Typical x-ray picture. Destruction spreading along the root surface
Covering a tooth with a crown or making any other structure (onlay) does not prevent the occurrence of vertical root fracture, since by this moment it already exists.
To prevent the occurrence of vertical root fracture, you must follow the following recommendations:
- Avoid excessive preparation of the root canal, including when preparing it for installation of a pin structure.
- Avoid local thinning of the walls.
- Avoid excessive pressure and tension while compacting the gutta-percha.
- Avoid pressure during installation of any endocanal structure.
Literature
- Fuss Z, Lustig J, Tamse A. An Evaluation of Endodontically Treated Vertical Root Fractured Teeth: Impact of Operative Procedures. J Endodon 2001; 27:46–5.
2 Fuss Z, Lustig J, Tamse A. Prevalence of vertical root fractures in extracted endodontically treated teeth. Int Endod J 1999; 32:283–6.
- Gher ME, Dunlap RM, Anderson MH, et Clinical survey of fractured teeth. J Am Dent Assoc 1987; 174–177.
- Harvey TE, White JT, Leeb Lateral condensation stress in root canals. J Endodon 1981; 7:151–5.
- Holcomb J, Pitts D, Nicholls Further investigation of spreader loads required to cause root fracture during lateral condensation. J Endodon 1987; 13:277–84.
- Meister F Jr, Lommel TJ, Gerstein Diagnosis and possible causes of vertical root fractures. Oral Surg Oral Med Oral Pathol 1980;49:243–253.
- Meister F Jr, Lommel TJ, Gerstein H et An additional clinical observation in two cases of vertical root fracture. Oral Surg Oral Med Oral Pathol 1981;52:91–96.
- Pitts DL, Natkin Diagnosis and treatment of vertical root fractures. J Endod 1983;9:338–346.
- Rosen H, Partida–Rivera latrogenic fracture of roots rein–forced with cervical collar. Opera Dent 1986; 11:46–50.
- Tamse Iatrogenic vertical root fractures in endodontically treated teeth. Endod Dent Traumatol 1988; 4:190–196.
- Tamse A, Zilburg I, Halpern Vertical root fractures in adjacent maxillary premolars: an endodontic–prosthetic perplexity. Int Endod J 1998; 131:127–32.
- Tamse A, Fuss Z, Lustig J, Kaplavi An evaluation of endodontically treated vertical fractured teeth. J Endodon 1999;7:506–8.
- Testori T, Badino M, Castagnola Vertical root fractures in endodontically treated teeth: a clinical survey of 36 cases.
J Endod 1993; 19:87–90. ..
- Torbjorner A, Karlsson S, Odman Survival rate and failure
characteristics of two post designs. J Prosthet Dent 1995; 73:439–44.
- Vire Failure of endodontically treated teeth: classification and evaluation. J Endodon 1991; 17:338–42.
- Walton RE, Michelich RJ, Smith The histopathogenesis of vertical root fractures. J Endod 1984; 10:48–56.
- Yang S–F, Rivera E, Walton Vertical root fracture in nonen– dodontically treated teeth. J Endod 1995; 21:337–339.