Today, dentists have various diagnostic methods in their arsenal, and teleradiography is one of the most popular. The term is of Greek origin and means "remote recording". That is, teleradiography is essentially a type of radiography - an image of the internal structure of structures and tissues produced using x-rays. They only do it at a distance of about 2 m, which makes it possible to obtain a more accurate image, almost comparable to the real dimensions of the area being studied.
Teleradiography in orthodontics is of particular importance. With its help, the doctor receives the most accurate information about the location of the teeth, the degree of their displacement or inclination. Therefore, teleradiography in orthodontics allows you to plan the most effective correction.
The examination lasts several minutes. And during it there are no unpleasant sensations. Teleradiography is carried out using a special device (computer tomograph, digital cephalostat or orthopantomograph, which provides head fixation).
General characteristics of the procedure
Relatively recently, it became possible to accurately diagnose pathologies of the dental system.
This can be done using a new orthopantomograph with cephalstat. This device has two examination programs: pediatric and adult. It is distinguished by low radiation exposure and high accuracy of the resulting images. An X-ray examination carried out using such a device is called “teleradiography” (what it is and how important such an examination is in orthodontics will be described below), and such a procedure today is an integral part of orthodontic treatment.
Types of installations for teleradiography
The procedure is carried out using devices with high-power X-ray tubes that work as quickly and accurately as possible, with minimal radiation exposure:
- digital cephalostat is the best option;
- computed tomograph;
- an orthopantomograph equipped with a craniostat, that is, a device for fixing the head in a stationary state.
What can be determined?
Using a teleroentgenogram (TRG), you can obtain an X-ray image of the skull
in a lateral projection (as well as in other projections, which are described below), as close as possible to the real dimensions. Such scale and realism of the image allow us to make the most accurate calculations of the facial skull parameters and create a detailed picture of the pathology.
Determine the size of the cranial bones, their structure, location, connection
Using TRG, the exact dimensions of the jaws are determined and their location in relation to each other is assessed. This is very important when diagnosing bite pathologies. Also, a teleroentgenogram allows you to determine the size of the cranial bones as a whole, find asymmetry, disruption of their connections or other deviations from the norm. Such information may be required not only as part of dental treatment, but also, for example, when examining the skull of a patient who was injured in an accident, fell from a height and received a traumatic brain injury.
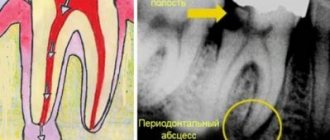
Detect a lesion with pathological tissue growth, its location
TRG allows you to identify foci of pathological tissue growth. In other words, this procedure allows you to diagnose various tumors, cysts and other disorders in the structure of bone tissue and gums. Based on the TRG image, an analysis is made of the size of the neoplasms, their localization, the cause of their occurrence is determined, and so on.
Determine the direction of tooth displacement
Using TRG, the angle of inclination of the front upper and lower teeth is determined, which helps to identify anomalies in their location.
As a rule, such a pathology is initially visible during the initial examination, but x-rays help to find out exactly how much the current position of the teeth deviates from the norm. Without such an image, the orthodontist will not be able to provide high-quality treatment. For example, when there is a strong protrusion of the front teeth, it is important to understand how much they need to be moved back. To do this, you may need to remove a couple of teeth from the front row and then install braces. After about a year of wearing braces, the teeth will move back, taking the places of the removed ones. The result is an aesthetic smile, as well as a fully functioning dental system.
Another option for correcting this pathology is to correct the type of tooth with extensions.
There are other solutions to this problem, and the TWG will help determine the most optimal one.
Determine the location of tissues in relation to the skull
A teleradiogram makes it possible to identify and study anomalies in the location of bone tissue, correlating it with the size and anatomical features of the patient’s skull.
Find the factors that affect malocclusion
TRG allows us to identify specific factors that influenced the formation of malocclusion in a patient:
- direct genetic predisposition;
- for children: long-term attachment to the pacifier, habit of thumb sucking;
- mouth or mixed breathing (for example, due to adenoids, chronic rhinitis, etc.).
Identify abnormalities that are difficult to treat
When orthodontic treatment aimed at correcting the bite does not produce results, TRG is prescribed in order to identify abnormalities that contribute to this. Perhaps these are the consequences of a birth injury or a broken jaw, etc.
Using teleradiography data to quantify dentofacial disorders
R. A. Fadeev Doctor of Medicine, Professor, Rector, Head of the Department of Orthodontics SPbINSTOM
A. N. Lanina postgraduate student of the Department of Dentistry of Novgorod State University. Ya the Wise
A. R. Andreishchev Candidate of Medical Sciences, Assistant of the Department of Surgical Dentistry and Maxillofacial Surgery of St. Petersburg State Medical University named after. acad. I. P. Pavlova
The article presents the results of an analysis of radiocephalometric parameters characterizing the morphology and aesthetics of the face, obtained as a result of a study of 135 lateral and 44 frontal teleroentgenograms of the skull of patients with various forms of dentofacial anomalies. Strong, moderate and weak connections between individual parameters were identified.
Based on the data obtained, groups of parameters recommended for assessing disorders of the facial structure in the sagittal and vertical directions were determined. The article presents a method for quantitative assessment of dentofacial anomalies. The severity of disturbances in morphology, occlusion, and aesthetics in the sagittal, vertical, and transversal directions was determined. The degrees of severity of dysfunction, tooth retention, and adentia are proposed.
Introduction
According to various data, the prevalence of dentofacial anomalies (DSFA) is more than 50% in children and 30% in adults (Yu. L. Obraztsov, 1991; Z. Raad., 1994; P. Falconi e. a., 1987). Studies conducted in 2003 among the teenage and adult population of St. Petersburg indicate an increase in the incidence of dental anomalies. Thus, according to V.N. Trezubov, R.A. Fadeev and O.V. Barchukova, it is 79% among this cohort of those examined [11].
Teleradiography plays a significant role in the diagnosis of anomalies. Teleradiography (gr. tele - into the distance, far, grapho - writing) is an x-ray research method, the principle of which is to increase the distance between the x-ray tube and the film (1.5 m) when the cassette with the film is located close to the head of the subject. Due to this, the absorbed dose of x-ray radiation is reduced and spatial distortions of the resulting image are minimized. Pacini was the first to take such photographs; in 1922, he proposed shooting from a distance of 2 m, bringing the X-ray film as close as possible to the object being photographed [2].
In 1931, B. Broadbent in the USA and H. Hofraph in Germany simultaneously and independently proposed a standardized technique for obtaining lateral images of the head using an X-ray machine and a head stand, called a cephalostat [2].
Teleradiography is an additional research method in orthodontics, orthopedic dentistry, and maxillofacial surgery, which is necessary to clarify diagnostic information obtained through examination and study of diagnostic models of the jaws.
Using this method, information about the shape and structure of the facial skeleton, various options for the location of the jaws in it, their size is detailed, and the predominant direction of growth of the facial skeleton is determined [14]. This method helps to differentiate anatomical variants and various forms of dentofacial anomalies, identify the localization of anomalies, and study the relationship of the soft tissues of the face with the facial skeleton [12, 13].
X-ray cephalometric analysis of the face includes the following elements:
- visual assessment of TRH;
- identification of anthropometric points and construction of cephalometric planes;
- X-ray diffraction;
- making a diagnosis.
PHPA are characterized by disturbances in morphology, dental relationships, facial aesthetics, as well as functional disorders. The severity of the signs of HSPA may vary. Thus, pronounced occlusion disorders can be combined with significant changes in facial aesthetics (Fig. 1) and, conversely, against the background of significant occlusal disorders, the patient may have only minor changes in facial aesthetics (Fig. 2).
Rice. 1a. The patient has severe occlusion disorders
Rice. 1b. The patient has pronounced changes in the facial profile
Rice. 2a. The patient has severe occlusion disorders
Rice. 2b. The patient has severe occlusion disorders accompanied by minor changes in the facial profile
Throughout the development of orthodontics, a large number of classifications of PCP have been proposed. The first morphological classification of occlusion belongs to E. Engle (1898). It is based on the principle of closure of the first permanent molars. Engle proceeded from the fact that the first permanent molar of the upper jaw occupies a certain place in the dentition, erupting after the second primary molar. Depending on the nature of the closure of the first permanent molars, the author identified three classes of dental anomalies (Fig. 3) [3].
Rice. 3a. Angle classification: first class
Rice. 3b. Engle's classification: second class, first subclass
Rice. 3c. Engle's classification: second class, second subclass
Rice. 3g. Angle classification: third class
Subsequently, a large number of classifications were proposed, such as the classification of P. Simon (1919), the etiopathogenetic classification of Kantorovich (1932), the classification of A. I. Betelman (1956), the clinical and morphological classification of D. A. Kalvelis (1957), the classification of anomalies occlusion of the dentition by L. S. Persin (1989).
The World Health Organization (WHO) recommends the following classification of MCL: anomalies of maxillo-cranial relationships, anomalies of the relationship of dental arches, anomalies of tooth position, unspecified malocclusion, maxillofacial anomalies of functional origin. It should be noted that none of the presented classifications makes it possible to evaluate dentoalveolar anomalies quantitatively, i.e., to answer the question to what extent this or that sign of DSPA is expressed.
In this regard, we set a goal: using teleradiography data, to develop a system for quantitative assessment of PCA. To achieve this, the following tasks were formulated:
- Using the results of x-ray cephalometric analysis of lateral TRGs, to identify correlations between x-ray cephalometric parameters characterizing the morphology of the facial skull in the sagittal and vertical directions and the aesthetics of the face in the sagittal direction.
- Determine the parameters that are most suitable for assessing the signs of AF.
- Determine the degree of severity of signs of PVPA in the sagittal, vertical and transversal directions.
- Develop a system for quantitative assessment of APLA.
- On the basis of the method of quantitative assessment of AFLP, develop a computer program for automated assessment of signs of AFLP.
Clinical population and research methods
We examined 265 patients with various forms of dentoalveolar anomalies: 115 men and 150 women (Fig. 4) aged from 9 to 59 years, the average age of the examined was 21±8.60.
Rice. 4. Distribution of those examined by gender
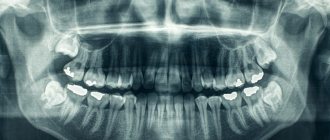
135 lateral TRGs of the skull, 44 TRGs in frontal projection, 135 frontal and profile photographs of the face and 86 pairs of jaw models were analyzed. Persons who had previously received orthodontic treatment were excluded from the examination.
Among the examined, 155 people were identified with a mesial relationship of the dentition and 114 with a distal one. An open bite was combined with a mesial relationship of the dentition in 123 subjects, with a distal one in 54. Deep incisal overlap in combination with a distal relationship of dentition was noted in 38 cases, with a mesial relationship in 17. Among the examined, 22 people had normal incisal overlap in combination with distal relationship of the dentition, 15 - with the mesial one (Fig. 5).
Rice. 5. Distribution of those examined according to the depth of the incisal overlap
Among those examined with a mesial relationship of the dentition, 36 had lower prognathia, 24 had upper micrognathia, 20 had upper micro- and retrognathia, 16 had lower macro- and prognathia, 16 had lower macrognathia, 14 had upper retrognathia, 4 - upper retro- and lower macro- and prognathia, 3 - upper retro- and lower prognathia, 2 - upper and micro- and lower prognathia, in 20 the anomaly was localized at the level of the dentition.
Among patients with distal dentition, 38 people had lower micrognathia, 37 had lower retrognathia, 22 had lower micro- and retrognathia, 2 had upper macrognathia, 2 had upper macro- and lower micro- and retrognathia, 13 the anomaly was localized at the level of the dentition (Fig. 6).
Rice. 6. Distribution of those examined depending on the identified pathology: a) with a mesial relationship of the dentition; b) with a distal relationship of the dentition
The following methods were used during the study:
- Analysis of teleroentgenograms using the proposed modified method (Fadeev R. A., Kuzakova A. V., 2009) [11]. The method includes 16 groups of parameters that allow assessing violations of the morphology of the facial skull in the sagittal and vertical directions, as well as facial aesthetics in the sagittal direction. An automated version of the Cephalo simplex technique was used.
- Analysis of photographs and TRG in direct projection was carried out according to the method of Trezubov V.N., Fadeev R.A., Dmitrieva O.V., 2002 [1], an automated version of the “Harmony” technique was used.
- Expert assessment method.
- A method for retrospective evaluation of treatment results in patients with PCPA.
- Analysis of literature data.
- Correlation analysis was carried out in the STATISTICA 6 program.
- Statistical data processing in Matlab 2009.
Bone, dental and skin points were identified on copies of the lateral TRGs in the Cephalo simplex computer program. Next, calculations were made and diagnoses of the subjects were obtained (Fig. 7).
Rice. 7. Screen form of the automated version of the modified technique for analyzing lateral TRG Cephalo simplex: identification of bone, skin and dental points
Research results
The correlation analysis revealed a strong negative correlation between the Wits parameters and the interapical angle ss-n-spm (ANB) (r = -0.82) (Fig. 8), a strong positive relationship between the angle of inclination of the base of the mandible to the plane of the base of the skull Pm/Pb and the growth angle of the facial skull ns-gn (r = 0.84) (Fig. 9).
Rice. 8a
Rice. 8b
Rice. 9a
Rice. 9b
A strong positive relationship was obtained between the angle of facial convexity Kn-prn-Kspm and the angle of convexity of the facial profile Kn-sn-Kspm (r = 0.77), strong negative relationships between the angle of convexity of the facial profile Kn-sn-Kspm and the aesthetic angle Pe/Pn (r = -0.83), facial convexity angle Kn-prn-Kspm and aesthetic angle Pe/Pn (r = -0.73) (Fig. 10) [4].
Rice. 10. Convexity angle of the front profile Kn-sn-Kspm. Facial convexity angle Kn-prn-Kspm. Aesthetic angle Pe/Pn. Pe/Pn and Kn-sn-Kspm (r = -0.83), Pe/Pn and Kn-prn-Kspm (r = -0.73), Kn-sn-Kspm and Kn-prn-Kspm (r = 0.77)
Thus, to assess morphological disorders in the sagittal direction, we can recommend the Wits parameter and the interapical angle ss-n-spm; in the vertical direction, the angle of inclination of the base of the lower jaw to the plane of the skull base Pm/Pb and the growth angle of the facial skull ns-gn can be recommended. To assess aesthetic disorders in the sagittal direction, you can use the facial convexity angle Kn-prn-Kspm, the aesthetic angle Pe/Pn, and the facial profile convexity angle Kn-sn-Kspm [4].
Based on the analysis of TRG in the lateral and direct projections and the above research methods, we were able to identify 3 degrees of severity of morphological disorders in the sagittal direction for patients with a distal and mesial relationship of the dentition (Fig. 11); in the vertical direction for patients with vertical and horizontal types of growth of the facial part of the skull (Fig. 12); in the transversal direction (Fig. 13) [6–10].
Rice. 11a. Degrees of severity of morphological signs of PCA in the sagittal direction for patients with distal dentition: 1st degree, 2nd degree, 3rd degree
Rice. 11b. Degrees of severity of morphological signs of PCA in the sagittal direction for patients with distal dentition: 1st degree, 2nd degree, 3rd degree
Rice. 11th century Degrees of severity of morphological signs of PCA in the sagittal direction for patients with distal dentition: 1st degree, 2nd degree, 3rd degree
Rice. 11 Degrees of severity of morphological signs of PCA in the sagittal direction for patients with mesial relationship of the dentition: 1st degree, 2nd degree, 3rd degree
Rice. 11d. Degrees of severity of morphological signs of PCA in the sagittal direction for patients with mesial relationship of the dentition: 1st degree, 2nd degree, 3rd degree
Rice. 11th. Degrees of severity of morphological signs of PCA in the sagittal direction for patients with and mesial relationship of the dentition: 1st degree, 2nd degree, 3rd degree
Rice. 12a. Degrees of severity of morphological signs of PCA in the vertical direction for patients with a vertical type of growth of the facial part of the skull: 1st degree, 2nd degree, 3rd degree
Rice. 12b. Degrees of severity of morphological signs of PCA in the vertical direction for patients with a vertical type of growth of the facial part of the skull: 1st degree, 2nd degree, 3rd degree
Rice. 12th century Degrees of severity of morphological signs of PCA in the vertical direction for patients with a vertical type of growth of the facial part of the skull: 1st degree, 2nd degree, 3rd degree
Rice. 12 Degrees of severity of morphological signs of PCA in the vertical direction for patients with a horizontal type of growth of the facial part of the skull: 1st degree, 2nd degree, 3rd degree
Rice. 12d. Degrees of severity of morphological signs of PCA in the vertical direction for patients with a horizontal type of growth of the facial part of the skull: 1st degree, 2nd degree, 3rd degree
Rice. 12th. Degrees of severity of morphological signs of PCA in the vertical direction for patients with a horizontal type of growth of the facial part of the skull: 1st degree, 2nd degree, 3rd degree
We have also identified 3 degrees of severity of facial aesthetic disorders in the sagittal direction for patients with a convex, as well as a straight or concave type of facial profile (Fig. 14); in the vertical direction for patients with an increase in the lower / decrease in the upper or a decrease in the lower / increase in the upper height of the face (Fig. 15); in the transversal direction (Fig. 16) [5-10].
Rice. 13a. Degrees of severity of morphological signs of PCA in the transversal direction: 1st degree
Rice. 13b. Degrees of severity of morphological signs of PCA in the transversal direction: 2nd degree
Rice. 13th century Degrees of severity of morphological signs of PCA in the transversal direction: 3rd degree
Rice. 14a. Degrees of severity of violations of facial aesthetics in the sagittal direction for patients with a convex type of facial profile: 1st degree, 2nd degree, 3rd degree
Rice. 14b. Degrees of severity of violations of facial aesthetics in the sagittal direction for patients with a convex type of facial profile: 1st degree, 2nd degree, 3rd degree
Rice. 14th century Degrees of severity of violations of facial aesthetics in the sagittal direction for patients with a convex type of facial profile: 1st degree, 2nd degree, 3rd degree
Rice. 14 Degrees of severity of violations of facial aesthetics in the sagittal direction for patients with a straight or concave type of facial profile: 1st degree, 2nd degree, 3rd degree
Rice. 14d. Degrees of severity of violations of facial aesthetics in the sagittal direction for patients with a straight or concave type of facial profile: 1st degree, 2nd degree, 3rd degree
Rice. 14th. Degrees of severity of violations of facial aesthetics in the sagittal direction for patients with a straight or concave type of facial profile: 1st degree, 2nd degree, 3rd degree
Rice. 15a. Degrees of severity of violations of facial aesthetics in the vertical direction in patients with an increase in the lower / decrease in the upper height of the face: 1st degree, 2nd degree, 3rd degree
Rice. 15b. Degrees of severity of violations of facial aesthetics in the vertical direction in patients with an increase in the lower / decrease in the upper height of the face: 1st degree, 2nd degree, 3rd degree
Rice. 15th century Degrees of severity of violations of facial aesthetics in the vertical direction in patients with an increase in the lower / decrease in the upper height of the face: 1st degree, 2nd degree, 3rd degree
Rice. 15 Degrees of severity of violations of facial aesthetics in the vertical direction in patients with a decrease in the lower / increase in the upper height of the face: 1st degree, 2nd degree, 3rd degree
Rice. 15d. Degrees of severity of violations of facial aesthetics in the vertical direction in patients with a decrease in the lower / increase in the upper height of the face: 1st degree, 2nd degree, 3rd degree
Rice. 15th. Degrees of severity of violations of facial aesthetics in the vertical direction in patients with a decrease in the lower / increase in the upper height of the face: 1st degree, 2nd degree, 3rd degree
Rice. 16a. Degrees of severity of violations of facial aesthetics in the transversal direction: 1st degree
Rice. 16b. Degree of severity of violations of facial aesthetics in the transversal direction: 2nd degree
Rice. 16th century Degree of severity of violations of facial aesthetics in the transversal direction: 3rd degree
The system for quantitative assessment of the dentition is supplemented by three degrees of severity of violations of the relationship of the dentition in the sagittal direction for the distal and mesial relationship of the dentition, in the vertical direction for open and deep bite, in the transversal direction in the anterior and lateral parts of the dentition. The system also includes 3 degrees of close position and 3 degrees of tooth retention, 2 degrees of edentulism and 3 degrees of functional impairment [6-10].
On the basis of the system for quantitative assessment of signs of AFLP, the computer program “Ortho-Expert” was created (Rospatent certificate of state registration of a computer program No. 2011615185 dated 07/01/2011), which allows you to automate work with the system (Fig. 17).
Rice. 17. Screen form of the “Ortho-expert” program
conclusions
- Correlations between radiocephalometric parameters characterizing the morphology of the facial skull in the sagittal and vertical directions and the aesthetics of the face in the sagittal direction were revealed.
- Parameters for assessing the signs of AFPA have been determined.
- Based on the analysis of lateral TRGs, TRGs in a direct projection, photographs of the face and diagnostic models, as well as using methods of expert assessment of treatment results and analysis of literature data, a systematization of the PCA has been proposed, allowing a quantitative assessment of the symptoms of the anomaly in the sagittal, vertical and transversal directions.
- On the basis of the system for quantitative assessment of signs of CPLA, a computer program for automated assessment of signs of CPPA “Ortho-Expert” has been developed.
- An objective assessment of the signs of CPPA will help determine the degree of complexity of the proposed treatment, choose tactics for correcting CPPA, and judge the effectiveness of the treatment based on changes in the severity of the signs.
Discussion and practical recommendations
All data obtained during the examination of the patient can be entered into the following tables (Table No. 1, 2).
Table No. 1. Results of quantitative assessment of the PCA: morphology, occlusion, aesthetics, function
| Direction | Morphology | Occlusion | Aesthetics | Function |
| Sagittal | ||||
| Vertical | ||||
| Transversal |
Table No. 2. Results of quantitative assessment of PCL: close position of teeth, retention, adentia
| 1st degree | 2nd degree | 3rd degree |
| Close position of teeth | ||
| Retention | ||
| Edentia |
Thus, having received a description of the dental anomaly according to all its characteristics, it is possible to draw up a treatment plan for the patient, taking into account the degree of severity of all components of a particular PCA.
To illustrate how to work with the system for quantitative assessment of PCA, we present an extract from the medical history. Patient N., 47 years old, arrived at the surgical hospital to perform the surgical stage of orthodontic treatment. Photographs of the patient's face, his dentition, as well as lateral TRG and OPTG are presented in Fig. 18-20.
Rice. 18a. Photographs of the face of patient N., 47 years old, in the preoperative period: front photograph of the face
Rice. 18b. Photographs of the face of patient N., 47 years old, in the preoperative period: front photograph of a face with a smile
Rice. 18th century Photographs of the face of patient N., 47 years old, in the preoperative period: profile photograph of the face
Rice. 19a. Photographs of the dentition of patient N., 47 years old, in the preoperative period: dentition in the right projection
Rice. 19b. Photographs of the dentition of patient N., 47 years old, in the preoperative period: dentition in a direct projection
Rice. 19th century Photographs of the dentition of patient N., 47 years old, in the preoperative period: dentition in the left projection
Rice. 20a. Lateral TRG of patient N., 47 years old, in the preoperative period
Rice. 20b. OPTG of patient N., 47 years old, in the preoperative period
There was a distal relationship of the dentition, lower retro- and micrognathia, protrusion of the upper and lower incisors, a decrease in the angle of the lower jaw, an increase in the interincisal overlap (more than 8 mm), and an increase in the interincisal distance along the sagittal (6 mm). Tables No. 3 and 4 contain information about the severity of the patient’s signs of PCA.
Table No. 3. Results of quantitative assessment of the PCA of patient N., 47 years old, in the preoperative period: morphology, occlusion, aesthetics, function
| Direction | Morphology | Occlusion | Aesthetics | Function |
| Sagittal | 3 | 2 | 2 | 2 |
| Vertical | N | 3 | N | |
| Transversal | 1 | N |
Table No. 4. Results of quantitative assessment of the PFA of patient P., 47 years old, in the preoperative period: close position of the teeth, retention, edentia
| 1st degree | 2nd degree | 3rd degree |
| Close position of teeth | + | |
| Retention | ||
| Edentia |
The treatment plan included correction of the shape of the dental arches and position of the teeth, osteotomy of the lower jaw and the creation of tight occlusal contacts. In Fig. 21-23 show photographs of the patient’s face, dentition, as well as lateral TRG and OPTG in the postoperative period.
Rice. 21. Photographs of the face of patient N., 47 years old, in the postoperative period: front photograph of the face
Rice. 22a. Photographs of the dentition of patient N., 47 years old, in the postoperative period: dentition in the right projection
Rice. 22b. Photographs of the dentition of patient N., 47 years old, in the postoperative period: dentition in a direct projection
Rice. 22c. Photographs of the dentition of patient N., 47 years old, in the postoperative period: dentition in the left projection
Rice. 23a. Lateral TRG of patient N., 47 years old, in the postoperative period
Rice. 23. OPTG of patient N., 47 years old, in the postoperative period
From tables No. 5 and 6 it can be seen that many signs of PCA have become less pronounced, and some parameters have taken on normal values, which indicates the effectiveness of the treatment.
Table No. 5. Results of quantitative assessment of the PCA of patient N., 47 years old, in the postoperative period: morphology, occlusion, aesthetics, function
| Direction | Morphology | Occlusion | Aesthetics | Function |
| Sagittal | 3/N | 2/N | 2/1 | 2/N |
| Vertical | N/1 | 3/N | N | |
| Transversal | 1/N | N |
Table No. 6. Results of quantitative assessment of the PFA of patient P., 47 years old, in the postoperative period: close position of teeth, retention, adentia
| 1st degree | 2nd degree | 3rd degree |
| Close position of teeth | + | |
| Retention | ||
| Edentia |
- Dmitrieva O.V. Photogrammetric analysis of facial signs of dental anomalies: Dis. Ph.D. - St. Petersburg, 2002. - 187 p.
- Trezubov V.N., Fadeev R.A. Planning and forecasting the treatment of patients with dental anomalies. - M.: MEDpress-inform, 2005. - 224 p.
- Trezubov V.N., Shcherbakov A.S., Mishnev L.M., Fadeev R.A. Orthopedic dentistry: textbook. - St. Petersburg: Foliant, 2010. - 656 p.
- Fadeev R. A., Ispravnikova A. N. Identification of correlations between various x-ray cephalometric parameters // Institute of Dentistry. - 2009, No. 2. - P. 22-24.
- Fadeev R. A., Ispravnikova A. N. Results of an expert assessment of violations of facial aesthetics in various forms of dentofacial anomalies. // Institute of Dentistry. - 2009, No. 2. - P. 22-24.
- Fadeev R. A., Ispravnikova A. N. System for quantitative assessment of dentoalveolar anomalies (part 1) // Institute of Dentistry. - 2010, No. 2. - P. 22-23.
- Fadeev R. A., Ispravnikova A. N. System for quantitative assessment of dentoalveolar anomalies (part 2) // Institute of Dentistry. - 2010, No. 3. P. 24-27.
- Fadeev R. A., Ispravnikova A. N. System for quantitative assessment of dentoalveolar anomalies (part 3) // Institute of Dentistry. - 2010, No. 4. - P. 28-31.
- Fadeev R. A., Ispravnikova A. N. System for quantitative assessment of dentoalveolar anomalies (part 4) // Institute of Dentistry. - 2011, No. 1. - P. 30-32.
- Fadeev R. A., Ispravnikova A. N. System for quantitative assessment of dentoalveolar anomalies (part 5) // Institute of Dentistry. - 2011, No. 2. - P. 28-31.
- Fadeev R. A., Kuzakova A. V. Clinical cephalometry. A textbook on diagnostics in orthodontics. - St. Petersburg: MEDI publishing house, 2009. - 64 p.
- Netzel Frank, Schultz Christian. Practical guide to orthodontic diagnostics. - Lvov: GalDent, 2006. - 174 p.
- Legan HL, Burstone Ch. J. Soft tissue cephalometric analysis for orthognatic surgery // Austr. Dent. J. - 1988. - Vol. 38, No. 10. - P. 744-751.
- Proffit, William R. Fields, Henry W., Jr. Contemporary Orthodontics // Mosby, 2006. - 768 p.
Indications for use
Teleradiography in orthodontics, without exaggeration, is considered the most effective and informative diagnostic procedure and is prescribed for a number of indications.
When correcting the bite
Today, malocclusion can be completely eliminated if high-quality and effective orthodontic treatment is carried out. It, in turn, cannot be carried out without an x-ray, which will show how complex the pathology is, associated problems, and so on.
Making the correct diagnosis or clarifying it
It is sometimes difficult to understand the causes of toothache, incorrect tooth growth, soreness and bleeding gums during an initial examination of the oral cavity. TRH may be prescribed to clarify the diagnosis.
Planning and prognosis of treatment for various dental anomalies
Before installing dentures, braces, implants, sinus lifting, tooth extraction and other dental operations, it is necessary to do a TRG to accurately determine the treatment plan.
Monitoring the ongoing processes of changes in periodontal tissues
Treatment of periodontal disease, pulpitis, periodontitis and other complex diseases of the oral cavity requires monitoring over time. In this case, an x-ray will show how effective the treatment is.
What is a TRG image in orthodontics?
During the diagnostic process, a TRG image is taken. It allows the doctor to get an idea of the relationship between the bone structures and soft tissues of the area being examined. Unlike a conventional X-ray, a TRG image shows a more complete picture.
Orthodontics, as is known, deals with the correction of dental anomalies. Therefore, TRG in orthodontics is prescribed to those who need the installation or replacement of appropriate structures. These can be braces, plates or aligners.
TRG in orthodontics is prescribed, as a rule, at the stage of treatment planning in Moscow clinics. However, it can be carried out both during treatment and after it. This is necessary to observe the dynamics and evaluate the result.
Types of teleroentgenogram
There are several types of teleradiography. The doctor’s task is to choose exactly the option (or several) that will help create the most complete picture of the pathology.
Frontal
Frontal TRG is considered the main diagnostic procedure and is prescribed before the start of orthopedic treatment. An overview image of the head is taken from the back and front and allows you to clearly see the existing inflammatory processes, facial asymmetry and fractures.
TRG in lateral projection
A lateral view of the TRG is performed to diagnose abnormal jaw development and prevent its consequences. In addition, a lateral teleroentgenogram provides the doctor with the opportunity to examine the jaw from the side and calculate the inclination of the lower teeth and those located in the upper row. This x-ray is often taken before a patient is assigned to wear braces.
Axial
Axial TRG (also called “mental”) is an additional diagnostic procedure along with lateral or frontal. Axial TRG is necessary to determine changes in the structure of the cheekbones, maxillary sinus and nasal cavity. Mainly used when implantation of the upper front teeth is necessary.
Teleradiography (TRG), price for service
Moscow clinics everywhere offer this type of diagnostics, such as teleradiography (TRG). The price of the service depends on the type of equipment, distance from the center and some other factors. Nevertheless, the average price of its implementation is about 1700-1800 rubles.
However, it is worth noting that the main task of a diagnostician is the calculation and analysis of TRG. The price of this service in Moscow clinics varies between 4500-8000 rubles. Interpretation of the image allows you to determine the timing of correction, predict the result, avoid complications, etc. Therefore, it is so important, in addition to the image, to decipher the TRG. The price of this service is justified, since it determines how correct the treatment will be.
The Novodent clinic also offers a type of diagnostics such as teleradiography (TRG). The price for the image and its analysis is indicated in the “Cost” section.
How is diagnosis carried out?
Typically, a TRG image is taken in a standing position (in special cases, when it is difficult for the patient to stand, a lying position is allowed).
The patient stands close to the device, the doctor helps him take the desired head position. To fix the head, special plastic supports are inserted into the ear canals. Before the image, the patient’s face along the midline of the soft tissue (including the soft palate) is lubricated with a barium suspension, this is necessary to create contrast in the image. The photo is taken in a few seconds. The procedure is painless and relatively safe.
Advantages of the technique
A teleroentgenogram (almost every dentist can tell you in more detail what it is) has some advantages over other diagnostic procedures:
- high information content of images (with the help of TRG, especially if it is done in several projections at once, it is possible to identify almost all pathologies of the dental system
); - instant results;
- safety and painlessness (can be done on children and pregnant women in the second trimester).
Indications
Teleroentgenograms are performed for diagnostic purposes in both adult patients and children.
Here are the main indications for the study:
- injuries of the dentofacial apparatus;
- abnormalities in the structure of the jaw or teeth;
- clarification or diagnosis;
- assessment of the effectiveness of the treatment;
- the presence of pain in the area of the temporomandibular joint.
TRH is always prescribed at the stage of preparation for orthodontic treatment and surgical interventions in the maxillofacial area.
Contraindications
There are a number of contraindications for performing TRG of the skull in one of the possible projections (lateral or other).
Bleeding and/or pneumothorax
Conditions such as open bleeding and pneumothorax (accumulation of air or gases in the pleural cavity) require urgent medical attention, possibly surgery. Radiography
(in particular, the TRG method), if required, will only be done after solving the problems described above.
General serious condition of the patient
It is not recommended to disturb a patient who is in serious condition once again to perform an x-ray (in particular, for an x-ray of the skull). The condition can worsen even from moving along the hospital corridor, so it is better to either refuse an x-ray or have it done later, when the patient’s well-being improves.
Pregnancy (especially 1st and 3rd trimesters)
The first and third trimesters of pregnancy are contraindications for taking most medications, as well as performing many diagnostic procedures, especially x-rays. There is a possibility (albeit very small) that in the first trimester, when all the organs and systems of the fetus are developing, ionizing radiation can disrupt this process. The third trimester is dangerous because any disturbance in the ongoing development of the fetus (which theoretically could occur due to exposure to X-rays), excessive anxiety of the expectant mother or other negative factors can provoke premature birth.
How often do they do it?
Teleradiography is considered a safe study and can be done several times a year. The radiation dose during the procedure is minimal (about 20 microsieverts). For comparison, during classical fluorography the radiation is 110 microsieverts.
The frequency of TRG is determined by the doctor individually in each specific case. For example, an image is always taken at the stage of preparation for orthodontic treatment, during the correction process and after its completion.