Glossitis is an inflammatory disease of the tongue, which can act as an independent pathology or be a symptom of other diseases of the internal organs. Sometimes a change in the shape or color of the tongue may be the only sign indicating a problem in the body. Therefore, it is important not to ignore painful changes in the oral cavity.
Self-medication can lead to chronic glossitis, which is characterized by severe growths and the appearance of ulcers. Seeing a doctor will help you make a correct diagnosis and cope with the disease in a short time.
Symptoms
Depending on the type of disease (and there are quite a few of them), typical signs will vary. Nevertheless, there are general symptoms that are similar for all forms.
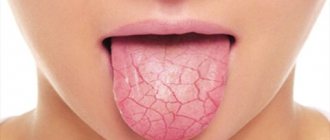
First of all, glossitis changes the appearance of the tongue: growths that are dense to the touch are formed on it or areas are formed whose color differs from the healthy mucous membrane (the shade can vary from red to burgundy). In addition to visual changes, there are other symptoms:
- burning of the tongue, often accompanied by swelling;
- increased salivation;
- feeling of a foreign body in the mouth;
- changes in taste sensations (foods may acquire an unusual taste, sometimes a person becomes completely unable to perceive the taste of food);
- difficulty swallowing;
- change in diction (speech becomes slurred; in order to express a simple thought, a person has to make serious efforts, because due to pain it is difficult for the patient to pronounce words clearly).
If treatment is neglected, there is a high probability that the disease will enter the chronic stage: its onset is indicated by a change in the structure of the tongue and a noticeable increase in its size.
What is desquamative glossitis?
The surface of the tongue is covered by a mucous membrane lined with stratified epithelium. Normally, it is pink and uniform in color. With desquamative glossitis, the epithelium begins to exfoliate and slough off, forming red spots of varying sizes with a light border. Inflamed areas can cause pain and a burning sensation, but often the disease is not accompanied by discomfort, so the patient may not notice it at all.
Foci of inflammation periodically change their location: the epithelial layer is restored in one area, then destroyed in another. Thus, the spots constantly “migrate”, and the language becomes like a geographical map. This is where desquamative glossitis gets its informal name.
Causes of the onset of the disease
The following factors can cause the development of glossitis in adults:
- herpes virus that affects the mucous membrane;
- the presence of tartar, untreated caries;
- inflammation of the gums;
- poor oral hygiene;
- low immunity;
- burns;
- alcohol and smoking abuse;
- tongue injuries from sharp edges of fillings and teeth;
- allergies to certain foods or toothpaste components;
- overly spicy foods consumed on a regular basis.
The most common cause of glossitis in children is tongue biting. In addition, incorrectly selected braces, as well as a number of diseases (dermatitis, diabetes, the presence of worms) can provoke the disease. Often, children develop candidal glossitis, which looks like a white coating on the surface of the tongue.
Answers on questions
What diagnostics are carried out before treatment?
The dentist examines the patient, collects medical history data: complaints, data on the patient’s general health (presence of chronic diseases). If necessary, laboratory diagnostics are prescribed: a smear (culture) from the oral cavity for microflora.
How to treat hairy tongue in adults?
The doctor prescribes complete sanitation of the oral cavity: removal of stone, plaque, and carious teeth. Selects individual home hygiene products. Prescribes a diet that includes plenty of fluids and solid vegetables. Smoking is prohibited. If necessary, the dentist prescribes rinsing solutions and antibacterial agents.
Types of glossitis of the tongue
There are many forms of this disease, differing in their symptoms. Glossitis can be:
- diamond-shaped, when thickened, diamond-shaped areas of epithelium form on the back of the tongue (their color varies from red to bluish). As a rule, this indicates chronic diseases of the gastrointestinal tract;
- folded (folds in the tongue, which are a congenital anomaly), which does not require treatment (however, it is still carried out for aesthetic purposes at the request of the patient);
- interstitial (a section of muscle tissue is replaced by connective tissue, the tongue becomes dense and inactive. If measures are not taken in time, connective tissue will completely replace muscle tissue), which occurs in patients with syphilis;
- deep, in which the inflammatory process often leads to the formation of phlegmons and abscesses, affecting the chin and neck area;
- catarrhal (determined by redness of the tongue and a thick coating on it);
- desquamative, when furrows, cracks and areas of scaly peeling appear on the sides and back of the tongue. It is often observed in cases of disturbances in the gastrointestinal tract and circulatory system, as well as during pregnancy. This type of glossitis is also called geographic tongue due to the large number of grooves and lines on the surface of the tongue, similar to the outlines of the continents;
- Gunter's (atrophy of the papillae occurs, the surface of the tongue gradually becomes smooth - all these signs indicate the onset of anemia).
Drug treatment
The diagnosis is usually made by visual examination. To clarify the causative agent of inflammation, a scraping from the surface of the tongue is prescribed for further laboratory testing. The patient is also referred for consultation to specialized specialists - a gastroenterologist, immunologist, endocrinologist or hematologist. If glossitis acts as a symptom of a pathology of internal organs, then therapy will be aimed at the underlying disease.
Treatment is complex. Local methods include:
- Treatment of affected areas with antiseptic solutions.
- The use of anti-inflammatory ointments with a wound healing effect.
- Rinse with herbal decoctions in consultation with your doctor.
To increase the body's immune strength, vitamin therapy is carried out. For severe pain, analgesics are prescribed. In case of purulent form, it is recommended to take antibacterial drugs. But such treatment is prescribed only after identifying the exact cause of the disease. After the acute period is over, the oral cavity is sanitized if necessary.
The prognosis is favorable, but only if you consult a doctor. Self-medication leads to worsening of the disease. Frequent complications of glossitis are abscesses, phlegmon and oncological formations. These conditions require surgery.
As a preventative measure, it is recommended to visit the dentist regularly, treat chronic diseases of the internal organs, and carefully monitor oral hygiene.
How to treat
The treatment methods used will directly depend on the reasons that provoked the development of glossitis, so high-quality diagnosis comes to the fore.
It is impossible to say for sure which doctor treats glossitis, since it will depend, again, on the reasons that caused the disease: you should start by visiting a dentist, who, in turn, may need to consult a therapist and even a surgeon.
If glossitis is a consequence of diseases (syphilis, gastrointestinal problems, anemia), then it is necessary to eliminate these diseases.
To reduce pain, the doctor may recommend applying local lotions with Lidocaine, Pyromecaine and other anesthetics. This procedure can actually be carried out at home. In order to speed up recovery, the tongue is regularly cleaned of plaque with a cotton swab soaked in Chymotrypsin. If there are ulcers, lotions with Iruksol are prescribed. Traditional medicine methods are also allowed, for example, rinsing with a decoction of chamomile or soda, lubricating the affected areas with propolis and much more.
There are quite a few treatment options: the doctor will be able to choose the most effective one, so at the first signs of illness you should not delay visiting him.
Preventive techniques for glossitis
Most often, the disease is much easier to prevent than to treat.
For this reason, dentists advise following the following preventive techniques:
- following the rules of dental and oral hygiene;
- systematic preventive examination in the dental office;
- reducing the use of hot spices that irritate the mucous membrane of the tongue;
- giving up cigarettes and alcoholic beverages.
Timely and high-quality treatment can easily eliminate glossitis, while the complete absence of therapy leads to irreversible and sad consequences.
Most common reasons
Sometimes, the causes of glossitis are congenital, for example with a folded tongue. But most often the disease develops against the background of:
- Chemical and thermal burns.
Putting garlic paste on a sore tooth may not be such a good idea. And hot food is harmful to the mucous membrane of the tongue and stomach. - Infections.
Do you have a red spot on your tongue and it hurts? This may be a symptom of a fungal (candidiasis), viral (herpes), bacterial (Helicobacter, spirochete, staphylococcus, streptococcus) infection. - Mechanical damage.
Gnawing on nuts is dangerous not only for teeth, but also for the mucous membrane of the mouth and tongue. Sometimes constant mechanical impact is caused by incorrect prosthetics. - Lack of vitamins
, especially group B. This affects tissue metabolism, resulting in inflammation of the mucous surface. - Psychoneurological factors.
With stress or neurological disorders, the tongue becomes inflamed quite often.
Glossitis is an inflammation of the tongue, which can occur either primarily or as part of other pathological conditions. Complications of glossitis include abscess formation (purulent melting of tissue with the formation of a cavity), spread of inflammation to surrounding tissues, septic processes, difficulty breathing when the abscess is located at the root of the tongue, pain during meals, which can lead to severe protein deficiency, as well as malignant degeneration of a focus of chronic inflammation.
The development of glossitis is caused by traumatic injuries to the mucous membrane of the tongue, primary infection with pathogenic flora, or other pathological conditions with impaired differentiation of the epithelium. Traumatic ulcerations usually occur as a result of mechanical impact from teeth, foreign materials (braces, piercings), self-harm and other factors. In addition to injuries, risk factors for glossitis include poor oral hygiene and other inflammatory diseases of the oropharynx (tonsillitis, pharyngitis), as well as caries. When pathological flora (especially staphylococcus) is deposited on the ulcerative defect, abscesses and phlegmon can form. The classification of purulent inflammation of the tongue includes division by etiology (dental, odontogenic, tonsillogenic), by localization and course - acute or chronic inflammation on the back, root, body.
The main symptom in the clinical picture of glossitis is the development of a pronounced, rapidly increasing pain syndrome. With an abscess of the tongue, speech and swallowing become sharply painful, a general increase in body temperature is possible, pain can radiate to other areas (ear, throat), touching the tongue is sharply painful. If the abscess is localized in the area of the root of the tongue, then there is a change in speech (it becomes dysarthric), pain when opening the mouth, talking and eating. Cellulitis is characterized by increased pain, hoarseness, difficulty breathing, and sometimes closing the mouth becomes impossible due to its significant enlargement.
Diagnostic criteria also include enlargement of the submental and submandibular lymph nodes, wasting of the tongue muscles during a prolonged process, increased salivation, bad breath, swelling of the tongue, facial asymmetry and other rarer symptoms.
Diagnosis and treatment of glossitis is carried out by a gastroenterologist, as well as a dentist.
To diagnose glossitis, in addition to identifying the listed symptoms, visualization of the source of inflammation (visible erosion, ulcer, palpable solid formation) is required. Additional examination methods are usually not required, however, if the treatment is ineffective, bacteriological examination and determination of sensitivity to antibacterial drugs can be used. If an oncological process is suspected, a CT or MRI or biopsy may be required. When an abscess ruptures or a therapeutic puncture occurs, the contents must be sent for bacteriological and cytological examination. In a general blood test with an abscess, acute-phase indicators of inflammation may be noted - leukocytosis with a shift of the formula to the left, an increase in ESR, an increase in alpha globulins.
Differential diagnosis of traumatic injury should be carried out with such specific ulcers as tuberculous and syphilitic. These conditions can be distinguished by cytological examination of scrapings and bacterioscopy. Biopsy is required in cases suspicious for squamous cell carcinoma and lymphoid tumors. Abscess formation must be differentiated from actinomycosis (fungal disease), tumors, Ludwig's tonsillitis, lymphadenitis and other diseases.
Treatment of traumatic damage to the tongue is aimed primarily at correcting or eliminating the damaging factor - tooth deformation, replacement of metal structures, correction of the bite. To improve healing, it is necessary to adhere to dietary prescriptions, possibly the use of local anesthetics, rinses, the use of non-steroidal anti-inflammatory drugs, in some cases - steroidal anti-inflammatory drugs, as well as antibacterial drugs if there is an established bacterial etiology or the risk of developing an abscess in people with immunodeficiency. An abscess is treated only surgically by opening and draining the abscess and using antiseptic and antibacterial agents. Patients with a prolonged inflammatory process due to the risk of transformation into a tumor process should be monitored.
Causes of desquamative glossitis
In medicine, there is no clear list of reasons why desquamative glossitis occurs. This disease can be diagnosed separately, or can be caused by certain systemic disorders.
The causes of primary desquamative glossitis include mechanical damage - injury from sharp edges of teeth or poorly fitted orthopedic structures, burns from hot food and chemicals. It is also common in young children as a reaction to the appearance of their first teeth.