Gastritis is an inflammatory or inflammatory-dystrophic disease that affects the inner surface of the stomach. Normally, the mucous membrane lines the entire surface of the organ and plays an important role in the digestion process. Its glands are capable of producing hydrochloric acid, bicarbonate, gastric juice, lipase, the enzyme pepsin and other substances responsible for protecting the body from pathogenic microorganisms, activating metabolic processes in the body, and breaking down fats and proteins.
Classification of the disease
There are many types of pathology, but according to the severity of the signs of the disease, the degree of damage to the mucous membrane, and the frequency of symptoms, acute and chronic gastritis are distinguished. In the first case we are talking about a newly diagnosed disease, in the second - about repeated attacks of the disease.
Acute gastritis can be:
- Catarrhal.
- Fibrinous.
- Corrosive.
- Phlegmonous.
Chronic gastritis is divided into the following types:
- Bacterial. The cause of the development of pathology is the bacterium Helicobacter Pylori. The pathogen is resistant to the acidic environment of the organ and lives on its inner surface.
- Chemical. This type of gastritis occurs due to the aggressive effects of substances of endogenous and exogenous origin - bile, alcoholic beverages, some medications, various toxic substances.
- Autoimmune. It develops as a result of the erroneous influence of immune system cells on a person’s own tissues.
In rare cases, types of gastritis such as granulomatous, resection, lymphocytic, and radiation are diagnosed. Considering the degree of damage to the gastric mucosa, superficial, widespread, deep and erosive varieties of chronic gastritis are distinguished. Depending on the amount of hydrochloric acid in gastric juice, pathology may be accompanied by low or high acidity.
Features of the choice of drugs for the treatment of nocturnal hypersecretion of gastric juice
The content of the article
In the treatment of diseases associated with increased gastric acidity, antisecretory drugs—proton pump inhibitors (PPIs)—are widely used. They are effective for stomach and duodenal ulcers, GERD, and erosive esophagitis.
Mechanism of action of proton pump inhibitors
These diseases cause discomfort, can cause bleeding, lead to perforation of the walls, and predispose to cancer. But the effect of PPIs specifically on nocturnal hypersecretion of gastric juice is questionable. In addition, they have significant side effects, especially in older patients with chronic diseases and taking other medications.
A second option for antisecretory drugs that have also shown effectiveness in treating esophageal diseases are histamine 2 receptor antagonists (H2RAs). Moreover, their list of side effects and contraindications is shorter compared to PPIs, regardless of the severity of clinical symptoms, age of patients, concomitant diseases, or medications taken.
Complications of gastritis
If you do not take into account the doctor’s recommendations, inadequate treatment can cause serious consequences:
- Peptic ulcer disease. Most often it appears in the erosive form of the disease.
- Atrophic gastritis. Due to the low concentration of hydrochloric acid, the glands of the mucous membrane almost completely lose their ability to produce secretions and begin to be replaced by connective tissue. Refers to precancerous conditions.
- Gastric bleeding due to ulcers or erosions. It is characterized by shortness of breath, pale skin, weakness, the presence of blood in the vomit and black liquid stool. Refers to conditions requiring emergency medical care.
- Lack of vitamin B12 and folic acid. It occurs in the autoimmune form of the disease or in the advanced stage of atrophic gastritis, when the stomach glands stop producing the protein responsible for the absorption of vitamin B12.
- Anemia. It develops as a result of acute or chronic blood loss, as well as due to poor absorption of vitamin B12 from food by the body.
Nocturnal hypersecretion of gastric juice - why is it dangerous?
GERD is the most common disease of the esophagus, accompanied by heartburn, including attacks at night. For example, according to surveys, in the United States, 7% of the total population suffers from heartburn every day, and 14% suffer from heartburn less than once a week.
Shaker's study found that nocturnal symptoms of heartburn occur in most adults with heartburn:
- 79% of respondents say they feel heartburn at night;
- 75% of them say their symptoms affect their sleep quality;
- 63% believe that heartburn negatively affects the quality of sleep;
- 40% of respondents indicate a negative impact of the symptom on activity.
Of the 791 respondents who suffered from heartburn, only 41% used antisecretory drugs, and in only 49% of patients the drugs were effective in relieving symptoms.
Proximal migration of acid is thought to predispose to symptoms of GREB at night. Therefore, pathology can lead to damage to the upper respiratory tract and the appearance of respiratory diseases - pharyngitis, laryngitis, chronic bronchitis, bronchial asthma, sinusitis, chronic cough, hoarseness.
Chronical bronchitis
Causes of the disease
There are many factors that contribute to the development of the disease; they can be divided into two groups: endogenous (internal) and exogenous (external) causes.
Endogenous factors
Among internal causes, duodenal reflux and autoimmune processes in the body are of particular importance. With one pathology or another, a change in pH level is observed, which leads to irritation of the gastric mucosa and the development of an inflammatory process. Also play an important role:
- genetic predisposition of a person;
- the presence of parasites in the body;
- dental problems such as missing teeth, caries, malocclusion;
- endocrine diseases, sarcoidosis
- intolerance to dairy and soy products;
- HIV AIDS.
Exogenous causes
Gastritis can be caused by dietary disturbances, as well as by:
- the predominance of fried, smoked, spicy or fatty foods in the menu with a large number of preservatives and dyes;
- bad habits;
- age-related changes;
- constant use of corticosteroid drugs, NSAIDs, aspirin;
- chronic stress and depression.
Acute gastritis - symptoms and treatment
Diagnosis begins with interviewing and examining the patient. During the conversation, the gastroenterologist clarifies what the patient ate before the signs of acute gastritis appeared, what medications he is taking, and whether he has any concomitant diseases (neuralgia, gallbladder, liver or heart disease). Objectively, attention is drawn to pale and dry skin, coating on the tongue, rashes in the area of the nasolabial triangle, bitterness and bad breath. On palpation (palpation), pain occurs in the epigastrium with irradiation to the left or right hypochondrium.
To confirm the diagnosis, various laboratory and instrumental research methods are used.
Important laboratory tests include:
- clinical blood test;
- 13C-urease breath test for antigen to Helicobacter pylori;
- biochemical blood test - allows you to identify disturbances in the functioning of the pancreas, liver, gallbladder and its ducts.
most commonly used instrumental diagnostic methods are
- radiography with a contrast agent - allows you to examine the relief of the gastric mucosa and the degree of tension of its walls;
- Ultrasound of the stomach - makes it possible to study the affected areas during a detailed examination, but does not allow collecting material for a detailed laboratory study.
FGDS deserves special attention - insertion of a thin endoscope into the stomach through the esophagus. This procedure is the optimal diagnostic method for gastric diseases [12]. It is prescribed regardless of the patient’s age. It allows you to determine the areas and extent of damage to the mucosa, assess the risk of internal bleeding and timely detect a malignant neoplasm.
The advantage of FGDS is the ability to perform a biopsy - to pinch off a small piece of tissue from different parts of the stomach. This procedure is painless and cannot cause bleeding.
The rules for preparing for FGDS are quite simple:
- a few days before the procedure, you need to give up some medications or coordinate their use with your doctor;
- 12 hours before the examination, refuse to eat (if the procedure is scheduled for the morning, then the last meal can be at 18:00, but not later).
Often patients are emotionally frightened due to the upcoming FGDS. The procedure is unpleasant, but tolerable and practically painless. As a rule, 15 minutes are allotted for it, but in the absence of pathologies, the process takes no more than 2-5 minutes.
FGDS can take place under:
- general anesthesia;
- light sedation (pain relief);
- local anesthesia.
Most often, doctors use local anesthesia - irrigation of the mucous membrane of the pharynx and the root of the tongue with a special anesthetic drug. This is a reliable method, proven over the years, which does not cause any complications and is easily tolerated by patients of any age. It allows you to reduce the gag reflex and calm the patient, without causing complications. Within 10-15 minutes the patient feels the same as before.
Anesthesia (medicated sleep) is carried out in the absence of contraindications, is easily tolerated, makes it possible to avoid negative emotions from the procedure, and also allows the endoscopist to work calmly and efficiently. Medication-induced sleep is performed in many countries around the world on a regular basis during a standard endoscopic procedure (sleep endoscopy). Local anesthesia is often an exception to the rule and is performed in the presence of contraindications to intravenous sedation, of which there are very few.
Complications after FGDS are rare. These include: dry or sore mouth, headache due to the patient’s severe nervousness. When the walls of the stomach are straightened during the procedure, belching of air may occur.
to become infected during FGDS if the equipment is processed and sterilized not manually, but in automatic installations for washing endoscopes.
Stages of disease development
The disease occurs in four stages:
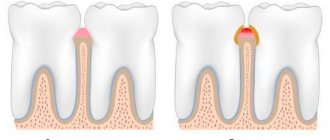
- Hyperemic. The gastric mucosa becomes reddish and swollen.
- Hypertrophic. There is a thickening of the mucosa with a simultaneous decrease in the production of hydrochloric acid. Changes in tissues and cells (dysplasia) and accumulation of leukocytes in the wall of the organ (metaplasia) are possible.
- Atrophic. With prolonged inflammation, the gastric mucosa becomes thinner, regeneration worsens, epithelial cells die, and are replaced by scar tissue.
- Erosive and/or ulcerative. On the inner surface of the organ, due to the thinning of the mucous membrane, lesions of varying depths form.
Features of the treatment of GREB with nocturnal hypersecretion of gastric juice
GERD is treated with antisecretory drugs. In the presence of endoscopic signs of GERD, treatment is more effective than when diagnosing non-erosive GERD. In case of ineffective treatment of non-erosive GERD, it is necessary to consider whether the patient is taking medications properly, whether the dose and duration of treatment are sufficient.
If non-erosive GERD is not treated effectively, other conditions should be considered. Often found:
- Functional dyspepsia. With this pathology, antisecretory therapy can relieve symptoms, but not enough.
- Regurgitation in patients with atrial syndrome, which may be associated with impaired peristalsis or lower function of the esophagus.
- Aerophagia.
- Achalasia.
- Eosinophilic esophagitis.
After endoscopic confirmation of GERD, and if there is no therapeutic response, it is necessary to determine whether the patient is taking the drug or dose correctly and check the duration of use, since resistance to PPIs is rare. Resistance is possible mainly due to a genetic mutation in the cytochrome system.
Treatment of the disease
In order to get rid of gastritis, the specialist prescribes:
- antibiotics whose action is aimed at Helicobacter pylori;
- antacids to neutralize hydrochloric acid and for pain relief;
- drugs to block the production of hydrochloric acid and heal the gastric mucosa.
In the case of an autoimmune process, immunosuppressants and corticosteroids can be used. In any case, the patient is recommended to give up bad habits, eat a healthy diet, and avoid stressful situations.
At the first signs of gastritis, do not wait for self-healing, make an appointment with a gastroenterologist. Ignoring the symptoms can lead to gastritis becoming chronic and causing serious consequences. Multidisciplinary medical specialists are always ready to help you.
Our clinic is equipped with the necessary medical equipment for diagnosing diseases, and our center employs experienced specialists. Timely prescribed treatment and a completed course of drug therapy will allow you to forget about the disease forever or significantly increase periods of remission.
Increased salivation - causes and features
Increased salivation (hypersalivation) is not always associated with food consumption. In this case, this indicates some disorders in the body. Heavy salivation can be a symptom of various internal diseases. Hypersalivation also occurs in dental pathologies. Therefore, if such a problem occurs, you should consult a dentist.
If the doctor discovers local causes, he will carry out the necessary treatment measures. If there is no dental cause, the dentist will refer you to another specialist for examination.
Features of the violation
Hypersalivation causes discomfort. You can understand that such a problem has arisen by the fact that you have to swallow saliva more often. There is also a constant feeling that there is a lot of it in the mouth.
Increased salivation is often accompanied by other unpleasant symptoms. For example, nausea, heartburn, unpleasant odor. Also, saliva sometimes changes color and becomes thick.
Hypersalivation in some cases is the norm. Excessive salivation is observed during teething, getting used to dentures, and during pregnancy. And, of course, this is the norm during meals.
Such a symptom will indicate a problem if it is present together with other signs.
Main symptoms:
- General malaise.
- Dyspeptic symptoms.
- Discomfort when swallowing.
- Change in taste sensations.
What are the reasons
Causes of hypersalivation include:
- intoxication of the body;
- period after tooth extraction;
- pathologies of the digestive system;
- hormonal disorders;
- problems with blood vessels and the thyroid gland;
- angina;
- menopause;
- stress;
- disorders of the central nervous system.
Treatment and prevention
Treatment varies greatly depending on the cause. Sometimes it is enough to sanitize the oral cavity and cure existing dental diseases. In some cases, it will be necessary to remove the salivary glands.
There are special medications that reduce saliva production. Medicines are prescribed only by a doctor after examination.
To avoid this problem, you need to visit the dentist regularly and treat dental diseases in a timely manner.
It is also important to undergo a general medical examination. It is important to monitor oral hygiene and have tartar removed by the dentist every six months. Giving up bad habits and eating healthy are important preventive measures. Good luck! Tags: increased salivation, hypersalivation, treatment and prevention of increased salivation, treatment and prevention of increased salivation Mosrentgen, treatment of hypersalivation Mosrentgen
Treatment of gastritis
Treatment for gastritis depends on the cause. Acute gastritis caused by taking NSAIDs or alcohol abuse does not require drug therapy; it is enough to exclude these triggers.
In other cases, your doctor may recommend:
- Antibiotic therapy against H. pylori.
- Drugs that block the production of hydrochloric acid (a component of gastric juice) and promote healing of the mucous membrane (proton pump inhibitors* - omeprazole, lansoprazole, rabeprazole, esomeprazole, dexlanzoprazole, pantoprazole.
- Antacids** (neutralize stomach acid, relieve pain).
* - Long-term use of proton pump inhibitors, especially at high doses, may increase the risk of hip, wrist and spine fractures, and an osteoporosis prevention program may be required. ** - Side effects - constipation, diarrhea.
Features and advantages of the gastritis treatment method at the Rassvet clinic
Diagnosis and treatment of gastritis at the Rassvet clinic is carried out in the gastroenterology department. We use evidence-based methods based on international clinical guidelines. Your primary treatment will begin only after a physical examination and all necessary tests and diagnostic tests have been completed.
Important. The influence of certain foods or dietary systems on the risk of gastritis has not been proven by research.
At the Rassvet Clinic, we first of all distinguish gastritis from functional dyspepsia. Gastritis is often asymptomatic, but it is necessary to treat it, since it is a slow but sure road to stomach cancer. Functional dyspepsia, on the contrary, is accompanied by many complaints, but endoscopic examination and biopsy do not reveal pathology.
How gastritis is treated at the Rassvet clinic
To clarify the diagnosis, we use the most modern and accurate equipment and logistics methods. For example, we have built a system for diagnosing gastritis and determining cancer risk according to the OLGA classification. Our endoscopes allow you to perform gastroscopy with multiple magnification and examine the mucous membrane through light filters, taking a biopsy from the most suspicious areas. The biopsy samples themselves are also assessed by the histologist using the OLGA scale, and as a result we obtain a figure that reflects the risk of oncological transformation in the coming years. Further treatment tactics depend on the value of this figure.
We value the comfort of patients, so in Rassvet you can undergo an examination under anesthesia in the shortest possible time.
Recommendations from a gastroenterologist at the Rassvet clinic for patients with gastritis
Timely consultation with a doctor and proper treatment will help keep the disease under control. A strict diet is not needed. However, the rules of a healthy diet should be followed - do not overeat, avoid foods that irritate the mucous membranes (smoked, fried, fatty), and give up alcohol. If you are forced to take painkillers that increase the risk of gastritis, check whether they can be replaced with a drug that is less aggressive on the gastric mucosa (acetaminophen, paracetamol).
Author:
Amelicheva Alena Aleksandrovna medical editor
Causes and risk factors of gastritis
- Bacterial infection Helicobacter pylori. It is one of the most common types of infections and is transmitted through the fecal-oral route, for example through contaminated food and water. For the development of gastritis, the presence of Helicobacter pylori infection alone is not enough. It is believed that vulnerability to the bacterium is inherited or occurs due to an unhealthy lifestyle (smoking, poor diet), medications.
- Painkillers (non-steroidal anti-inflammatory drugs, NSAIDs). Regular and excessive use of aspirin, ibuprofen or naproxen can cause both acute and chronic gastritis, their toxic effects reduce the production of the main protectors of the gastric mucosa. To distinguish this situation from other types of gastritis, it is called NSAID gastropathy.
- Alcohol. Irritates and gradually destroys the gastric mucosa, exposing it to the aggressive effects of gastric juice. Alcohol most often provokes acute gastritis.
- Age. Older people are at increased risk of developing gastritis because the lining of the stomach thins with age. Older people are also most vulnerable to infections (H. pylori) or autoimmune disorders.
- Stress. Severe stress associated with injuries, burns, severe operations and infections can trigger acute gastritis.
- Exposure to radiation or radiation therapy (due to another medical condition).
- Bile reflux after gastric resection.
- Allergies to foods such as cow's milk and soy (especially in children).
- Autoimmune diseases. As a result of autoimmune processes, the body produces antibodies that attack the cells that form the gastric mucosa. Autoimmune inflammation occurs, and the functions of the protective barrier of the mucous membrane decrease. Gastritis associated with autoimmune disorders is called autoimmune gastritis. It is more common in people with other autoimmune disorders, including Hashimoto's disease and type 1 diabetes. Autoimmune gastritis may also be associated with vitamin B12 deficiency.
- Other diseases. The risk of gastritis may be increased by other medical conditions, including Crohn's disease, sarcoidosis, parasitic infections, and HIV/AIDS.