If caries is not cured in time, and there is a deep carious lesion, the only way out is to remove the dental nerve. As caries develops, microorganisms violate the integrity of the enamel, as a result of which the nerve is exposed and reacts to any influence with unbearable pain.
Depulpation (nerve removal) is a modern way to preserve a unit of dentition without implantation.
When nerve removal is indispensable
In modern dental practice, both complete and partial resection are used. Indications for the procedure:
- deep carious tissue damage;
- chronic pulpitis (including asymptomatic);
- bactericidal infection spread by the apex of the tooth root;
- the presence of an extensive pulp area, the threat of developing periodontitis or transition to periodontitis;
- trauma leading to nerve exposure and tooth destruction;
- the need to correct a medical error;
- the need for prosthetics with low crowns.
Unbearable pain can also be an indication for depulpation.
The dentist will never prescribe such a serious intervention as long as it is possible to save the tooth.
Important : problematic “eights” when affected by caries, as a rule, are removed. This is due to the location of the “wisdom” teeth at the end of the dentition, which makes cleaning them from plaque and stone and filling the canals very problematic. Indications for removal are also the wrong direction of eruption, displacement of the dentition, malocclusion, and the development of pulpitis.
Indications for depulpation
When should a dental nerve be removed?
- Advanced caries;
- Pulpitis – including asymptomatic;
- Severe tooth trauma – partial destruction of the tooth and exposure of the nerve;
- Preparation for prosthetic crowns (at the discretion of the orthopedic dentist);
- Periodontitis;
- Consequences of unsuccessful treatment;
- Unbearable pain.
What is the dental nerve called?
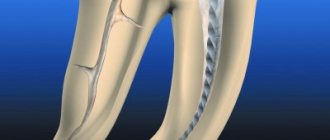
In dentistry, the dental nerve, or pulp, is a complex structure - an interweaving of nerves and vessels located inside the root and crown of the tooth and responding to external stimuli.
Depulpation allows you to save the damaged tooth, but has negative consequences:
- Since the pulp acts as a barrier to infections, removing the nerve deprives the tooth of the necessary level of blood supply and mineralization, which shortens its “life.”
- A tooth deprived of a nerve loses sensitivity, the enamel becomes more fragile and faded, and the strength of the tooth decreases.
Causes of dental pulp damage
The dentist is often visited because of caries - damage and destruction of enamel, which at the initial stage causes aesthetic discomfort.
Important: if the disease is started, the process affects the deeper layers of the tooth and pulpitis develops, that is, the neurovascular bundle becomes inflamed.
Pathologies arise due to the rapid proliferation of microbes, but in addition, the pulp can be damaged for the following reasons:
- gum disease, in which the neck of the tooth is exposed, the bone tissue is destroyed and harmful bacteria penetrate inside;
- trauma, as a result of which part of the tooth can break off, and then microbes enter the resulting cavity;
- mistake by the dentist who installed the filling or crown. If some actions were incorrect, then the nerve will make itself felt after a while.
These are the main causes of pulp damage. The symptoms of this condition will be acute. The pulp will begin to react to cold, hot, too spicy, sweet foods. Removing the nerve in such situations is a necessity, despite the fact that minerals and nutrients will stop flowing to the tooth.
Stages of the depulpation process
- X-ray – necessary to assess the condition of the pulp, the number, length and branching of the canals to be filled.
- Anesthesia - local or complete anesthesia completely covers the issue of pain when removing a nerve (it doesn’t hurt!). At the same time, general anesthesia is used relatively rarely - when treating children, with true dental phobia, etc.
- Installation of a rubber dam - a latex film for insulating a tooth. A modern solution to improve the dentist’s working conditions and protect against the possible spread of microorganisms through saliva.
- The actual removal of the nerve is the excision of tissues affected by caries, opening the pulp chamber and extracting the nerve with a special instrument (pulpoextractor). In modern practice, this is a careful cutting of the pulp without affecting sensitive areas.
- Installation of a temporary filling (for a period of 1-2 weeks).
- Control x-ray.
If the x-ray and the condition of the tooth are satisfactory, after the control period a permanent filling is installed.
Modern method of depulpation
Today, depulpation is carried out using a pulp extractor - a thin metal rod with teeth that can penetrate even remote areas of the root canals. The apex locator device helps determine the depth of the canal to reduce the risk of injury. After the procedure, a temporary filling is usually installed, but a permanent one can also be installed if the doctor does not see the risks of complications and has high-precision instruments on hand, for example, a dental microscope.
Depulpation before prosthetic crowns
Depulpation is unconditional if there is serious tooth decay. It is preferable to remove the dental nerve during prosthetics in the following cases:
- The size of the teeth determines the low position of the crown (too small or short teeth);
- The inclination of the prosthetic tooth is from 15°;
- Increased sensitivity of teeth;
- According to aesthetic requirements.
The need to remove the dental nerve during prosthetics is dictated by deep removal of the top layer of dental tissue: if the doctor is not sufficiently qualified, heating or touching the nerve can cause an attack of unbearable pain. However, cases of nerve-sparing crown installation also occur in modern dental practice.
If over time the nerve under the crown becomes bothersome, it is possible to remove the pulp through the top of the crown and fill the hole after removal.
The danger of such a procedure is associated with the risk of complications in the future due to surgery on the exposed dental nerve.
Should I remove the nerve in the tooth or not? That is the question!
Agree, it is quite a common situation when, after treating caries with a therapist or treating a tooth with a crown by an orthopedist, the latter may begin to bother you. One of the controversial questions that patients have to face at this moment is when to remove the nerve in a tooth , and under what circumstances is there a chance to keep the tooth alive? In reality, this question is not always clear-cut for dentists either. In this article we will try to figure out what the difficulty is here.
Firstly, you need to immediately decide that a “living” tooth is always and definitely better than a “dead” one. Because under the “nerve” there actually lies an entire organ, consisting not only of the nerve, but also of blood vessels and other tissues and cells needed by the tooth. And all this is called pulp. It provides the tooth with both nutrition and protection from any external influences. And therefore, without it, it is difficult for our teeth to count on a long and happy life.
But often as a result of caries, injury or dentist intervention (for example, when grinding living teeth for crowns), an inflammatory process can occur - pulpitis . And here it is very important how reversible this process is. This is what is important for the doctor to determine when rendering a verdict on the pulp - to execute it (i.e., depulpate the tooth) or to pardon it (leave the tooth “alive”).
And here we can say that 100% reliable methods for diagnosing the reversibility of the inflammatory process in the pulp do not yet exist. If we had the opportunity to look inside the tooth with a microscope, then determining the vitality of the pulp would not be difficult. But it is impossible to do this on a living patient; such an opportunity is currently available only to pathologists. As a rather cynical saying goes, this is why these doctors are least likely to make a mistake in diagnosis. So what remains for practicing dentists? How can they avoid making mistakes? Which path should you take? You can only rely on much less informative indirect signs and use your experience and intuition.
Let us briefly examine what is still available to us when making a decision.
Patient complaints.
Of course, one of the most subjective signs, however, sometimes very informative. Therefore, it is often enough to listen to your feelings to understand how bad things are with your tooth. Depulpation certainly cannot be avoided if:
- You feel a fairly strong aching pain that occurs without any apparent reason and does not go away for a long time. At the same time, it can intensify when changing the position of the body (mainly when trying to bend over or lie down), and also noticeably intensifies at night. Usually in such a situation, many people run to the pharmacy for a pack of painkillers, although the most correct thing in this situation is to call your dentist with a request for an urgent appointment...
- You do not feel aching pain all the time, but only from some irritant (most often from cold ). The important point is that this pain does not go away immediately after removing the irritant for some time (from several seconds or more).
If, upon contact with cold, you feel only a short, instantly passing pain, then, most likely, everything for the pulp, maybe not right away, will end well. Any other sensations of discomfort, for example, painful biting or sensitivity when touched by a brush when brushing your teeth, are usually associated with completely different things and do not talk about the condition of the pulp.
Cold test.
This point smoothly follows from the first and is based on the inadequate reaction of the inflamed pulp to irritation (primarily to cold). This can be used for diagnostic purposes and, so to speak, to conduct reconnaissance in force. The technique is simple, but with a touch of slight sadism. The doctor cools the cotton ball with a special spray and touches the “suspected” teeth with it one by one.
The resulting response is compared with that of obviously healthy teeth that are 100% above suspicion (i.e., they are on the other side, on the other jaw and do not have carious holes or any traces of previous treatment). If suddenly someone wants to “play dentist” and can’t wait to find a bad tooth themselves, then at home you can do this test yourself by applying, for example, an ice cube from the freezer to different teeth one by one.
In general, self-diagnosis is pointless, but in this case it can still be useful to understand your own feelings, and then more confidently poke the doctor at the problem tooth.
It should be noted that this method is good primarily only in order to understand which tooth is actually bothering you. After all, pulp pain is quite poorly localized, and the patient often cannot say which tooth is bothering him. It even happens that the pain from the causative tooth radiates to the opposite jaw. This happens especially often with pulpitis of 8 teeth (wisdom teeth). Therefore, if in such a situation you trust only the feelings of the patient himself, you can break a lot of wood and depulpate innocent teeth for no reason. It is almost impossible to judge the severity of the inflammatory process and its reversibility using a cold test. For each patient, “oh-yoyoy” and “ah-yayayy” can mean completely different things. Although, as in the first point, by the duration and severity of the pain reaction, the doctor can indirectly judge the hopelessness of attempts to keep the pulp alive.
X-ray.
Another highly informative technique for most cases, which is completely useless for determining the neglect and reversibility of the pulpitic process. X-rays can also only indirectly help identify a problematic tooth if there is any doubt about the “culprit” of the pain. The pulp itself, like soft tissue, does not show any changes on x-ray if it is inflamed. What signs can help a doctor suspect something is wrong?
— location of the previously installed filling close to the pulp chamber
In this image: the red line marks the border of the filling, the blue line marks the border of the pulp. As you can see, they are located quite close to each other.
- hidden, invisible during visual inspection, deep carious cavity in the interdental space
In this picture: the black arrow shows a hidden carious cavity that formed on the back side of the lower 7th tooth under the gum level and led to inflammation of the pulp. The reason in this case was the 8 (wisdom tooth) that was not removed in time.
-presence of denticles in the pulp chamber or root canals
In this image: the yellow line marks the border of the filling, which is close to the pulp (its borders are marked in red). A denticle has formed in the thickness of the pulp due to chronic irritation (marked in blue).
-small reactive expansion of the periodontal fissure around the apex of the tooth root
Electroodontometry (EDO).
This is an old, if not ancient, way to check the condition of the pulp using essentially the same method as with the cold test. Those. irritate her. Only in this case it is no longer a low temperature, but an electric current. This time, nothing sadistic, as everyone usually thinks when explaining the essence of the technique. To carry it out, it is not at all necessary to pass current through the entire patient in some kind of electric chair. It is enough to connect a special small device to the tooth, which generates rather weak microcurrents.
By the value to which the tooth “responds” with slight tingling and pinching, one can judge (again, very approximately, unfortunately) the degree of pulp viability. The advantage of this method compared to the cold test is that instead of “ouch” and “ouch”, the doctor deals with impartial readings from the device. Another thing is that 100% of these indications can only be used to judge whether the pulp is alive at all, or whether it died a hero’s death. Everything else, again, is very conditional.
In the end, what do we have? There are 2 main problems with teeth suffering from pulpitis (or very similar pain : difficulties in some clinical cases in determining the source of pain, and difficulties in making a decision about preserving/removing the pulp. As we have seen, it is not easy for even an experienced and knowledgeable doctor to objectively understand these issues in all cases. If with the first question mistakes can almost certainly be avoided, then with the second... while there are no methods for objectively assessing the condition of the pulp, each doctor will make decisions at his own discretion. Someone, playing it safe, depulps all the teeth in a row indiscriminately. Someone is trying to keep them alive. The more data a doctor can collect and interpret correctly, the risk of making an erroneous decision will be minimized. In general, this is an iron law of medicine: the better and more thorough the diagnosis, the more correct and effective the treatment.
What happens if a mistake is made? I'll tell you one example from my practice. A young girl went to the doctor complaining of aching pain in her teeth “somewhere on the right side.” Without any special diagnostics, treatment began... First, one tooth with a deep filling was depulped, which seemed the most suspicious to the doctor. The pain remains. Then - the next one, the pain did not go away. Then both right normally erupted wisdom teeth were removed. The pain even intensified for a while... Instead of stopping and thinking at that moment, the doctor depulped another 3 (!!!) completely intact (i.e. untouched) teeth on this side, but on the other jaw. When the pain did not go away even after that, the girl, suspecting something was wrong, went to look for reasons in other places. Ultimately, she was diagnosed with trigeminal neuralgia, which, although it is not always well and quickly treated, in her case it was released quite quickly due to the treatment prescribed with the help of a neurologist. The result of the diagnosis using the “finger in the sky” method was 5 completely needlessly killed teeth.
Therefore, it is so important to collect as completely as possible all possible subjective and objective information if the situation is confusing. In this case, the probability of making a wrong decision will tend to zero. In addition, you should strive to preserve the pulp in the tooth, and do not rush into radical decisions if in doubt. At the same time, in borderline cases, you should always monitor the result of treatment, even if the pain has subsided. A cold test, x-rays, and odontometry will be able to promptly identify asymptomatic (“silent”) pulp death and the need for its removal. Otherwise, a cyst may grow completely unnoticed near the root of the tooth. And then there is a risk of losing the entire tooth.
About dental anesthesia
Standard dental practice is an injection of anesthetic; Taking tablet analgesics before going to the dentist is not recommended, as it leads to a decrease in the effectiveness of anesthesia (usually the effect of an anesthetic injection is 45 minutes). For patients suffering from a fear of injections, it is possible to use paste anesthesia, which has a similar effect.
The choice of anesthesia is up to the dentist; Taking into account the individual pain sensitivity threshold of each patient, the standard dose is sometimes doubled or even tripled. With proper selection of an anesthetic, discomfort during the procedure for the patient is excluded.
Why can a tooth hurt after pulp removal?
This often happens: the nerve has already been removed, but the pain remains. Such manifestations are acceptable in the first 3-4 days as a natural reaction of the body (for example, to clenching the jaws or to temperature stimuli).
Other causes of toothache after pulp removal:
- Careless cleaning of the canals, preservation and intensification of the inflammatory process due to incomplete removal of tissue damaged by caries.
- Using during the procedure a pulp extractor that is not suitable for the size of the canal or improper handling of the instrument.
- Broken dental instrument, retention of its remains in the upper part of the root (such a medical error leads to the need to remove the tooth).
- The occurrence of a secondary inflammatory process in the treated canals (residual pulpitis) occurs against the background of an incompletely removed nerve.
- Allergic reaction of the patient to the filling material.
Modern pulp removal
Today, it is enough to go to the dentist once to remove the pulp. The doctor gives an anesthetic injection and calmly works with the tooth, removing the destroyed layer of dentin, extracting the pulp, treating and filling the canal. Sometimes inspection using a microscope is possible. To be on the safe side, your doctor may place a filling temporarily to make sure he has completely removed the pulp. And only if everything turns out to be in order, the final filling is installed.
Incomplete removal of the pulp is also possible, which makes sense if only the outer part of the pulp is affected by inflammation. Dead tissue is removed from the opened tooth, the outermost part of the pulp is removed, and the root remains intact. This is especially important on children's teeth, since the pulp is responsible for the formation of roots. When the pulp is not completely removed, the tooth is kept alive, and further destruction occurs more slowly.
Change in enamel color after nerve removal
If the dental clinic follows international depulpation protocols, such phenomena are excluded. However, in budgetary institutions there are frequent cases of using outdated practices.
The color of the enamel after nerve removal can be affected by:
- Improper preparation of the tooth for installation of a filling;
- Poor quality instrumental processing of channels;
- Low quality filling materials.
Thus, when using resorcinol-formalin paste (the use of the material is practiced in the treatment of baby teeth), the enamel acquires a pinkish tint; When using endomethasone, the tooth may turn yellow after a few years.
Sequence of treatment
- Diagnostics . After the doctor has examined you and collected your medical history, an X-ray is taken. This diagnosis allows you to evaluate the structure of the tooth and plan treatment. To see the full anatomy of the root canals, a computed tomography (CT) scan is performed - a 3D diagnostic that allows you to see all the structures of the tooth.
- Pain relief . Local infiltration or conduction anesthesia is performed. Before the injection, the gums are lubricated with an anesthetic gel so that the injection is not felt.
- Setting up insulation . Root canal work should be done in clean, dry conditions. For this purpose, rubber dam (insulation) is used. It is a latex plate that is placed on the tooth. Advantages of isolation: saliva and plaque do not enter the root canals. Medicines and solutions also do not flow into the patient’s mouth.
- Preparation of hard dental tissues . The doctor uses a drill to remove the destroyed tissue. To prevent overheating of the tooth, water flows from the tip. The doctor creates direct access to the root canals.
- Nerve removal . It is performed with thin sterile instruments similar to long needles. The doctor places an instrument into the root canal and removes the nerve. Machine rotary tools may also be used. This stage is completely painless, since anesthesia was previously performed.
- Mechanical and medicinal treatment of canals . The canals are washed with special antiseptic solutions and passed through with instruments. This allows you to completely remove the diseased nerve and relieve inflammation.
- Temporary filling . Root canal work is complex, so it is not always possible to treat a tooth in one visit. An anti-inflammatory paste is placed into the canals, a temporary filling is placed, and a further stage of treatment is planned.
For permanent restoration of the crown part of the tooth, ]esthetic dentistry[/anchor] will be required.
Possible complications
A medical error associated with poor-quality disinfection of the canal when removing a nerve can trigger the process of suppuration with subsequent transition to a periodontal abscess (in the absence of adequate treatment). This complication leads to the need for tooth extraction.
Other possible complications:
- Pain for several days after nerve removal. The duration of discomfort is individual for each patient; if pain persists for a long time, it is necessary to consult a doctor to re-open the canals and carry out disinfection.
- Increased bleeding of the canal occurs when the pulp extractor is removed after the pulp has been torn off. To avoid this phenomenon, many specialists carry out the procedure in stages with copious rinsing of the tissues with an antiseptic. Bleeding control is carried out directly at the appointment.
- The appearance of granuloma, fistula, cyst, gumboil.
Specific problems can arise if the material is applied incorrectly: if the filling extends beyond the boundaries of the root apex, the jaw nerve may be pinched.
If you experience pain in the lips and chin, you should urgently consult a dentist: a possible complication is facial paralysis.
Removal with arsenic
Once upon a time there was only one way to remove it, it was terribly painful, especially since you had to visit the doctor several times. At first, the doctor drilled the tooth down to the pulp with a drill, which was extremely painful. Next, arsenic was placed in the hole and it was temporarily sealed with a filling. In a couple of days, the arsenic dealt with the nerve, and the tooth hurt so much that no medicine could help. Then I had to go to the doctor again, he opened the temporary filling, removed the nerve, and cleaned the root canals. Pulp is a tenacious substance, so this process was also extremely painful.
This technology poses a certain danger, because arsenic is a poison, and the doctor, when using it, must be especially careful, and the patient must be careful: if you are late with the second visit to the doctor and leave arsenic in the tooth, it will completely destroy it, which will end deletion. Dentists stopped using arsenic and developed new techniques for removing pulp.