Causes of viral stomatitis in children
There are several causes of viral stomatitis in children. This:
- recent infectious diseases: herpes (80% of cases), influenza, adenoviral infections, measles, chicken pox;
- contact with a sick person: a viral type of stomatitis is transmitted by airborne droplets, as well as through some objects (toys, dishes, personal hygiene items, etc.);
- weak immunity.
Viral herpes in children is one of the most common forms of damage to the oral mucosa. This can be explained by the fact that babies are very sensitive to the herpes virus, and if one of the family members gets herpes, there is a high probability that the child will develop stomatitis.
Types and routes of infection
The ways of transmission of the disease, depending on its type, are clearly demonstrated in the table:
| View | Contagiousness | Path of infection |
| Viral | Yes | Infection can occur in the following ways:
|
| Bacterial | Yes | Children:
Adults:
|
| Fungal (candida) | Yes | There is no airborne transmission; infection can occur by sharing dishes and cutlery with an infected person. Factors that increase the risk of infection:
|
| Aphthous | No | Aphthous stomatitis is contagious only when accompanied by a viral infection: in this case, the routes of infection are the same as for the viral form. |
| Traumatic | No | There is no person-to-person transmission. |
Symptoms
- The child becomes nervous, capricious, lethargic, whiny, refuses to eat and sleeps poorly.
- With viral stomatitis, children sometimes develop a fever.
- The child complains of severe pain in the mouth, the submandibular lymph nodes are painful when pressed.
- There is an unpleasant odor from the mouth.
- When examining the oral cavity, you can see that the gums are swollen and bleeding, and ulcers (aphthae) have appeared on the tongue and mucous membranes - at first they resemble pimples, then they become covered with a whitish film.
Viral stomatitis in children is dangerous because at the initial stage its symptoms resemble a sore throat: the child has difficulty swallowing, complains of pain in the mouth, and upon examination the throat looks swollen. And if you self-medicate, you can ensure that dental aphthae will spread further. Only a specialist can make an accurate diagnosis.
Classification and forms of the disease
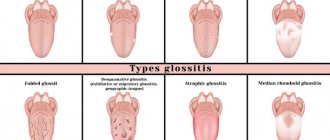
According to the nature of the disease, stomatitis can be:
- Spicy . The appearance of painful ulcers in the mouth is accompanied by fever. The disease lasts 2–3 weeks;
- Chronic . The disease progresses in waves, with periods of long lulls and rare exacerbations. Lasts up to 2–3 years.
According to the type of pathogen, stomatitis is:
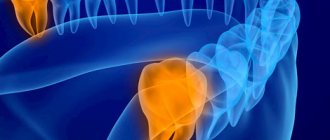
- Viral . Its causative agent is the herpes virus. It causes bubbles of clear liquid to appear. After the bubbles burst, aphthae remain in their place.
- Radial . If the mucous membrane is irradiated by ionizing radiation, compactions and erosions may occur.
- Fungal . Occurs when immunity decreases or a shock dose of antibiotics. A powdery coating forms on the seals of the mucous membrane, and when you try to remove it, the aphthae is exposed.
- Bacterial . Caused by streptococci and staphylococci. The whole process goes quickly - ulcers are actively formed, aphthae quickly stop hurting and heal.
- Chemical . This is the result of burns to the mouth from acids or alkalis. In this case, deep ulcers are formed and the tissue is deformed.
Depending on the type of pathogen, several forms of acute stomatitis are distinguished:
- Fibrinous. In the initial stage, rashes appear no more than 1–3 times a year during exacerbations of systemic diseases or microtraumas of the mouth. Small blisters covered with fibrous plaque are located on the inner surface of the lips, tongue, and cheeks. They scar after 1–2 weeks. If the cause of the disease is not treated, aphthae form more and more often and cover large areas.
- Necrotic. Typical for patients suffering from severe chronic pathologies. In this case, aphthae become a consequence of the death of the epithelium. In the initial stage, aphthae are painless, but then develop into ulcers that do not close within a period of several weeks to a month.
- Gradular . It develops when the salivary glands are damaged, and aphthae develop next to them. The ulcers are painful and take 1 to 3 weeks to heal, after which the ulcers reopen.
- Scarring. Aphthae cover the mucous membrane of the mouth near the salivary glands, pharynx and palate. At first they are small in size, but quickly unite into deep painful ulcers with a diameter of up to 1 centimeter. They heal slowly (up to 3 months) and form scars.
- Deforming. The most severe form of aphthous dermatitis. Aphthae grow deeply into the mucous membrane and, when healing, form rough scars that deform the oral cavity. Deforming stomatitis is the most difficult to treat; recovery will take at least 2 months.
- Herpetic . Consequence of infection by the herpes virus. Up to 30 small ulcers simultaneously form on the mucous membrane, the tissues become inflamed and turn bright red. It is more common in infants who become infected with the virus in utero or during childbirth.
- Recurrent . Aphthae do not heal for a long time, merge with each other and form a large painful ulcer. The lesions become covered with a white coating, make it difficult to eat, and the person suffers from pain and burning. This form of stomatitis occurs only in adults.
In children, 2 forms are most often observed:
- Spicy . Children under 3 years old are ill, usually against the background of other infectious diseases - whooping cough, diphtheria, measles. In acute stomatitis, a lot of saliva is released, the smell from the mouth is unpleasant, putrefactive.
- Mixed. They appear in children over 4 years of age and cause frequent relapses. In this case, the disease affects an increasingly larger area each time.
Treatment of viral stomatitis in children
The course of treatment for viral stomatitis in children depends on the timeliness of visiting a doctor, as well as the age and state of the child’s immunity. It may include:
- Rinse
As a rule, the dentist recommends treating the mucous membranes of the oral cavity with anti-inflammatory drugs. Also, for viral stomatitis in children, you can use decoctions of certain plants (calendula, chamomile, sage) or an infusion of oak bark. For small children who do not know how to rinse their mouths, irrigation can be done using a regular rubber bulb.
- Treatment with ointments and oils
After rinsing, for the treatment of viral stomatitis in children, sea buckthorn oil or vitamin A (in oily form) is usually used, which is used to lubricate the aphthae. If viral stomatitis in children is caused by herpes, the doctor will prescribe a special ointment. To treat the oral cavity with oils and ointments, you must use cotton swabs.
- Antipyretic and painkillers
Since the disease occurs with an increase in temperature and causes very painful sensations in the baby, the doctor prescribes appropriate medications. For example, for viral stomatitis in children, drugs such as Nurofen and paracetamol can be used.
What can cause stomatitis?
Many factors can lead to inflammation of the mucous membrane: from banal mechanical damage to disruptions in the body that are not related to the dentist’s field of work.
The following causes lead to stomatitis :
- neglect of oral hygiene recommendations;
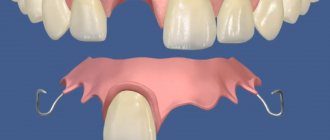
- injury to the mucous membrane from sharp edges of teeth or fillings, dentures or other objects;
- dental diseases - caries, tartar, etc.;
- allergies - not only to food, but also to hygiene products and even dental materials;
- various diseases - from viral to endocrine, such as diabetes;
- poorly made prostheses;
- expired prostheses;
- metabolic or immune disorders;
- problems with microflora in the body;
- direct contact with the mucous membrane of pathogenic microorganisms;
- bad habits - smoking, drinking strong alcohol;
- reaction to certain medications.
The mucous membrane is much easier to damage than the skin. Especially in the mouth, where it is always exposed to temperature changes, touched by teeth, dentures, braces and solid food particles.
The cause of dental disease is mainly pathogenic bacteria (for example, caries is caused by streptococcus), which also harm the gums. And tartar is a hardened plaque that contains not only microbes, but also other unfavorable components. In addition, if the stone is subgingival, then the mucous membrane suffers first.
In many cases, allergies are discovered suddenly. The patient may not be aware of its presence, since he calmly eats any food. However, chemicals in toothpaste or mouthwash can cause a reaction. Studies have shown a negative effect on the mucous membranes of sodium lauryl sulfate, contained in some toothpastes. If the problem began soon after the restoration or treatment of the tooth, then you should consider the possibility of the body's response to the filling or crown material.
Decreased immunity can also cause deterioration of gums. And metabolic disorders affect not only the supply of microelements to the body’s tissues (including the mucous membrane), but also the composition of saliva, a decrease in the protective properties of which makes the oral cavity vulnerable to bacteria. Approximately the same can be said about the beneficial microflora: if it is in order, it helps to suppress the work of harmful microorganisms; if it is disrupted, the microbes attack vulnerable areas.
The cause of stomatitis in adults and children can be obvious - direct entry into the mouth of a large number of pathogenic bacteria. They can get from contaminated surfaces. Simply put, if a child constantly puts various objects into his mouth, stomatitis may occur. If an adult has carried through the years the bad habit of biting nails or pens, this can also contribute to the appearance of inflammation.
Medicines can have different effects on the body, in particular, they can affect the immune system, microflora and saliva production. Dry mouth is promoted by antihistamines and antihypertensive drugs, anticoagulants, antipsychotics, antispasmodics, etc. And a low level of saliva production provokes the growth of bacteria. Antibiotics and anti-asthma medications can lead to Candida infections in the mouth. There can be many options, including the influence of the sugar contained in the medicine. stomatitis often appears in adults as a result of treatment for a completely different pathology.
How to avoid getting stomatitis again
To avoid getting stomatitis again, you need to follow 3 rules:
- Maintain hygiene.
- Treat teeth, check and change orthopedic structures in a timely manner.
- Monitor your general health.
The first rule for preventing recurrent stomatitis is hygiene. It is best to have your teeth professionally cleaned by a dental hygienist after the symptoms of the disease have disappeared. A specialist will use ultrasonic equipment to remove tartar and old plaque and advise on further dental care tactics in each specific case. The professional cleaning procedure should be carried out 2 times a year to remove accumulated dirt that regular cleaning cannot remove. This is especially true for patients with braces or dentures - the presence of foreign structures in the mouth requires regular professional cleaning.
It is necessary to treat teeth so that there are no putrefactive processes in the mouth, and there are as few pathogenic bacteria in the microflora as possible. And if the cause of stomatitis or contributing factors were disturbances in the functioning of the body, then you need to closely monitor your health and maintain your immunity.
Pathogens and causes of fungal stomatitis (thrush in the mouth)
The causative agent of the disease is a yeast-like fungal microflora of the genus Candida (hence the name - candidal stomatitis ), and in the overwhelming majority of cases the species Candida albicans. But in more rare cases, fungal stomatitis can also be caused by other types of fungal microflora, for example, Candida tropicalis, krusei, parapsilosis, glabrata.
Fungi of this genus (there are 150 varieties, of which about twenty can cause candidiasis), almost always present on the tissues of the oral cavity, are normally harmless, but do not benefit the body. Their reproduction is controlled by many factors: the chemical balance in the mouth, local and general immunity, and competing bacterial microflora. When these factors are suppressed, the balance is disrupted and the fungus begins to multiply intensively. Actually, candidal stomatitis is not caused by the fungus itself, but by the enzymes it secretes that destroy the components and structure of the epithelium of the mucous membrane.
Diagnosis of the disease
Before starting treatment for stomatitis, you should consult a dentist. The doctor will listen to complaints, conduct a visual examination of the oral cavity and skin, and also take scrapings from the affected areas. In some cases, consultation with a therapist, dermatologist, allergist and endocrinologist may be required.
Remember that timely diagnosis is the key to successful treatment and easy progression of the disease. Also, regardless of the causes and form of the disease, treatment in newborns should be carried out under the supervision of doctors.
Prevention
To prevent the manifestation of candidal stomatitis, you must adhere to the following rules:
- learn to brush your teeth so as not to injure the mucous membrane;
- use mouth rinses to cleanse the mouth;
- change your toothbrush every 2 months and rinse thoroughly after use;
- if you wear a denture, you must wash it thoroughly using special products, and also follow the storage rules;
- get rid of bad habits;
- if you are taking antibiotics, you must use antifungal drugs and probiotics as prescribed by your doctor;
- wash and treat with boiling water accessories that small children come into contact with;
- Nursing mothers are advised to maintain breast hygiene;
- hardening, physical education in the fresh air;
- visit the dentist regularly.
What happens if stomatitis is not treated?
To avoid the question “To treat or not to treat?”, you should remember two facts about inflammatory processes:
- Neglected inflammation eventually progresses to the chronic stage. This means that problems with the mucous membrane will continue in the future. Chronic inflammation not only causes constant discomfort, but can also develop into a more serious problem.
- Inflammation of one area of the mucous membrane can spread to others. Thus, inflammation of the gums and inner surface of the lips can spread to the respiratory tract and further.
Here are some of the possible complications:
- chronic stomatitis,
- respiratory diseases (for example, laryngitis),
- periodontitis,
- loosening of teeth (after periodontitis),
- scars on the mucous membrane after healing of numerous ulcers,
- gastrointestinal diseases
- vision problems (with a herpetic infection, inflammation can rise there too).