Hyperplasia as the main cause of pathology development
Why does this phenomenon occur when gums grow on a tooth? Most often this is due to the proliferation and enlargement of its cells. Scientifically, this process is called hypertrophy or hyperplasia (i.e. proliferation and increase in volume of tissue). The problem in most cases occurs against the background of an inflammatory process occurring in the oral cavity or metabolic disorders and hormonal imbalances in the body.
On a note! Hyperplasia or hypertrophy is a pathology in which soft tissue cells begin to grow uncontrollably, and the gums themselves can become inflamed and increase in size, they can begin to “crawl” onto the crown, partially or even completely (in the most advanced situations) block it.
Prerequisites for the development of hyperplasia
Various reasons can serve as prerequisites for accelerated and enhanced cell division:
- excessive accumulation of hard tartar and bacterial plaque above and below the gums,
- malocclusion: in such a situation, some teeth and, accordingly, the soft tissues and mucous membrane that surrounds them are subject to increased stress and pressure, they are constantly injured. The nutrition and blood circulation of tissues is disrupted, as a result of which their cells can begin to grow rapidly,
- endocrine diseases,
- genetic predisposition and heredity,
- long-term use of steroid hormonal drugs, antidepressants, anticonvulsants,
- hormonal imbalance during pregnancy, after childbirth, during menopause in women, changes in hormonal status in adolescents during puberty1,
- acute vitamin deficiency: hyperplasia often occurs due to a lack of vitamin C,
- traumatic damage to the mucous membrane due to incorrectly installed fillings, artificial crowns or braces,
- teething,
- leukemia
Main diseases characterized by tissue hyperplasia
Fibrous or hypertrophic gingivitis
Between the teeth there are gingival papillae, which during the development of fibrous gingivitis begin to gradually increase in size, they become denser and grow. In this case, the mucous membrane remains painless for a long time, and there is no bleeding.
Read more about all types and symptoms of gingivitis in a separate article on the website.
The disease develops against the background of poor oral hygiene and the accumulation of a large amount of plaque; it can appear due to poor-quality prosthetics and constant trauma to the mucous membrane. People who have hormonal imbalances or gastrointestinal diseases also encounter fibrous gingivitis. The disease often occurs in both adults and children.
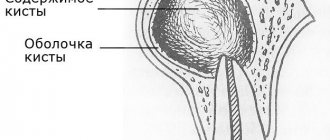
Important! A growth over a tooth is not always associated with hyperplasia; it can be nothing more than a gumboil, abscess, fistula or cyst, indicating advanced dental diseases. Most often, such manifestations are very painful, they are white in color, because... pus accumulates in them.
Fibromatosis
This is a hereditary disease and therefore often manifests itself in childhood. It is characterized by the growth of individual areas of the gums and proceeds very slowly. The color of the affected tissues is usually no different from healthy ones; they are painless.
The disease occurs mainly in the frontal area of the smile, and soft tissues can grow so much that they cover the crowns by more than 2/3. If fibromatosis is not treated, it is fraught with destruction of interdental septa, osteoporosis, and a severe violation of the aesthetics of the smile.
Fibropapilloma
If the gums have grown onto the crown, then a disease such as fibropapilloma may be to blame. This is a benign tumor. The tumor is hard to the touch, but painless. Its appearance in childhood is more dangerous, because can lead to disruption of the formation, growth and eruption of permanent elements.
Epulis
Epulis, like fibropapilloma, is a benign formation. It has a mushroom shape, because the tumor grows on a stalk. Appears as a result of chronic irritation and tissue injury. The most common location is the area of the incisors or canines. If the tumor is not removed, it can lead to pathological mobility and tooth loss.
Diagnosis and treatment of recession
During the dental examination, the doctor looks at how serious the gum recession is and conducts an instrumental examination. Determines the depth and width of the lesion in order to understand how much the tooth root is exposed, using a periodontal probe. Damage to the gums is calculated by the index of exposure of the gingival margin. After the dentist determines the extent of the disease, an effective treatment for recession is selected.
As gum recession gradually increases, it can lead to serious complications. So how to stop gum recession? The pathology should be treated in a timely manner. Treatment at an early stage always gives a guaranteed result in getting rid of the disease.
Therapy is possible using the following methods:
- cleaning from plaque and deposits;
- gum surgery;
- pfr-membranes (plasmolifting);
- physiotherapy;
✔ The initial stage of pathology is to cleanse plaque and deposits
, which may be in periodontal pockets. The dentist uses ultrasound to remove plaque and stone. The technique is called Air Flow.
Deep cleansing is performed using Vector and Varius devices. The specialist performs curettage of the gums. It comes in open and closed types. The open type is characterized by cutting the gums, treating the roots of the teeth, cleaning, and suturing. This is a full-fledged operation.
✔ Gumplasty
is an operation where the missing volume is filled and therapy is performed to achieve aesthetics. Before starting the procedure, caries is treated, deposits and stone are removed. Using a scalpel, the doctor makes an incision, then the gum is tightened or moved to another place. Next, the specialist applies stitches.
✔ Platelet Rich Fibrin
or plasmolifting involves the closure of gum recession due to the targeted injection of a composition from the patient’s blood plasma into the affected areas. It stimulates the regeneration of damaged cells. The substance is administered using PFR membranes or through injection. The membranes are sutured into gum tissue. Treatment is carried out in courses of 3-5 procedures.
✔Physiotherapy also has positive results
. Exposure to magnetic current, laser, or ultraviolet radiation gives a positive effect in treatment.
When the pathology is so advanced that all the above methods will not help, all that remains is to remove the loose teeth and install implants in their place. After tooth extraction and complex therapy, it is recommended to install an implant with a smooth neck and an antibacterial coating. To prevent receding gums, you need to ensure constant oral hygiene and protect yourself from traumatic factors.
Why does the problem appear in children and when should you see a doctor?
The situation when gums grow on a child’s tooth most often occurs during the period of teething, as well as the change from a primary bite to a permanent one. During eruption, the mucous membrane swells and increases slightly in size, because it is irritated, blood circulation increases in it, but in this case we are not talking about hyperplasia. However, it is necessary to monitor the condition of the child’s oral cavity over time.
You should consult a doctor in the following situations:
- if 2-3 months after the crown “hatched”, it did not come out completely, and most of it remains under the gum or soft tissue hangs over it, partially covering it,
- the baby tooth did not fall out during the change of bite, but gums are growing on it: perhaps a permanent element is “hiding” under the formed tubercle, which did not have enough space, and it began to make its way in a different direction or into the second row,
- the growth is filled with white contents, and the child has a bad smell from the mouth: perhaps we are talking about the presence of advanced dental diseases, which are complicated by a fistula, abscess or cyst.
Gum recession: why gums recede
The formation of gum recession occurs when the surface of the tooth root is exposed. Without consulting a dentist, you will never be able to determine the exact reason why your gums are receding. This is due to a whole range of possible reasons, and in addition there are a large number of predisposing factors that make the risk of recessions more likely. Let's look at them.
1) Occlusal trauma, overload of teeth –
Occlusal trauma means that the contacts between your lower and upper teeth are not ideal, and in some areas there may be so-called “super contacts” (areas of premature overbiting). Normally, when the jaws are closed, the contact of the premolars, canines and molars should first occur, and only lastly the incisors. But if your incisors close first, then after all the other teeth have closed, they will experience overload, which will lead to bone resorption and a decrease in gum level (see photo below).
In addition to improper contact between the upper and lower teeth, bruxism (excessive uncontrolled clenching of the jaws, most often at night) can lead to occlusal injury. Patients usually refer to this condition as teeth grinding during sleep. You can learn more about this disease using the link above.
Exposure of tooth roots as a result of occlusal trauma:
Excessive chewing pressure on the teeth for a long time leads to resorption of the bone around them. Accordingly, in parallel with the decrease in bone level, there is also a decrease in the level of the gums, which primarily becomes noticeable in the area of the lower anterior teeth. For example, if you are missing part of your lateral chewing teeth, this leads to a redistribution of the chewing load on the remaining teeth, which will cause them to be overloaded. The front teeth are not physiologically designed for chewing at all - their function is to bite off food. In the absence of lateral chewing teeth, chewing food occurs with the front teeth, which quickly leads to their overload.
The absence of even 1 chewing tooth on each side can quickly lead to a decrease in the bite height in the lateral parts of the jaws, and this in turn will lead to excessive contact of the upper and lower front teeth (which will also cause bone resorption and gum recession with exposure of the roots of the teeth) . Moreover, a decrease in bite in the lateral parts of the jaws can occur not only due to the loss of several teeth. This can also occur due to excessive abrasion of dental tissues (on the chewing surfaces of molars), due to errors in prosthetics or restoration of teeth with filling materials, as well as as a result of the gradual abrasion of old fillings.
What to do - if you do not have missing teeth, then you need either a “gnathologist” or a very good orthopedic dentist to carry out “selective grinding of teeth” (this procedure will normalize the contacts between the upper and lower teeth, removing all “super contacts”) . If you have a reduced bite height in the chewing parts of the jaws due to the absence of some teeth, you need prosthetics. We are talking about replacing missing teeth with artificial crowns, replacing old fillings on the chewing surfaces of molars with ceramic inlays... But you need to start with a consultation with a prosthetist.
2) Chronic generalized periodontitis –
We have already said above that one of the main reasons why gums recede is their inflammation. It all starts with a completely harmless superficial inflammation of the gums (gingivitis), which is manifested by bleeding gums, their swelling and pain when brushing your teeth. But in the absence of treatment or improper treatment of gingivitis, the attachment of the gums to the neck of the teeth is gradually destroyed, inflammatory bone resorption and the formation of periodontal pockets begin to occur.
Reduced gum level due to gum inflammation –
When bone destruction reaches a certain degree, tooth mobility also joins the symptoms. Destruction of the periodontal attachment, bone resorption, periodontal pockets, tooth mobility - these are all symptoms of the next stage of gum inflammation, which is called periodontitis. Accordingly, because When periodontitis occurs, the level of bone tissue around the teeth decreases, and the level of the gums will also decrease.
Important: please note that a decrease in the level of gums in the area of 1-2 teeth is possible even with the most initial form of gum inflammation - even with catarrhal gingivitis. And for this it is enough simply to have microbial plaque in the area of the necks of the teeth (+ the presence of some predisposing factors, for example, a thin gum biotype). But with chronic generalized periodontitis, subsidence of the gum level occurs immediately in the area of a large group of teeth.
What to do - you need to start with a consultation with a periodontist (this is a dentist who specializes in the treatment of gum inflammation). Treatment of periodontitis includes not only anti-inflammatory therapy and removal of dental plaque, but also splinting of movable groups of teeth and prosthetic replacement of missing teeth. Therefore, in addition to consulting a periodontist, you may also need to consult an orthopedic dentist.
3) Incorrect movements of the toothbrush –
If you brush your teeth with a horizontal motion (instead of a sweeping motion) every day year after year, this can lead to gum recession - especially in the area of the lower front teeth. Typically, such patients not only have receding gums, but also hard tissue defects of non-carious origin appear in the area of the necks of the teeth. Incorrect brushing technique plays an important role in the formation of gum recession - especially in the presence of predisposing factors (thin gums, small height of attached gums, concomitant catarrhal gingivitis, etc.).
4) After correcting the bite with braces -
After correcting the bite with braces, you can often notice a decrease in the level of the gums. What I want to say here... There are only a few good orthodontists, so most of them plan orthodontic treatment without taking into account factors such as the height of the attached gum, the biotype of the gum, the thickness of the cortical plate of the jaw in the area of the teeth being moved. And as a result, we have what we have...
5) In the presence of predisposing factors –
Below we present a number of factors that sharply increase the risks of gum loss and root exposure. In some cases, they themselves can be the cause of gum recession (such as a highly attached frenulum of the lower lip), but most often they increase the damaging effects of the causes that we described above. These predisposing factors relate to the individual anatomical features of the gum structure in different patients.
- If you have a thin gum biotype, thin biotype means a small gum thickness. With the same force of the damaging factor, in patients with thin gums, recession will occur faster and be deeper than in patients with thick gums.
- Thickness of the cortical plate of the alveolus - if your cortical plate of the jaw (the front wall of the alveolus) is too thin.
Let's look at this using the example of the lower incisors. The anterior surfaces of the roots of the lower incisors are covered with a thin layer of bone, on top of which soft gum tissue is already located. In some patients, this layer of bone may be too thin (less than 0.5 mm), which, in the presence of a damaging factor, leads to too rapid bone loss, followed by a decrease in gum height. In some patients it can be even worse. For example, on the front surface of the roots of the lower incisors (in the area of their upper thirds) there may be no bone plate at all. In this case, the upper third of the roots will be covered only by the gum. This situation creates a risk of a recession, i.e. the fact that the gums will recede and the tooth root will be exposed - maximum.
- The height of attachment of the frenulum of the lips - for example, the frenulum of the lower lip may be attached too high to the gum edge, and then the movement of the lips (during conversation and facial expressions) will lead to the frenulum “tearing” the edge of the gum from the teeth. The same will apply to the low-attached frenulum of the upper lip.
- Insufficient level of attached gum – the gum is usually divided into “attached” and “unattached” (see photo below). Above the dotted line is the attached gum, and below it is the non-attached mobile gum. The peculiarity of the attached gum is that it is firmly fused with the underlying tissues and therefore immobile. The unattached gum is mobile, and its peculiarity is that it follows the movement of the lips and cheeks.
Very often the gum recedes on a tooth that has a very small height of attached gum. There is a clear relationship - the lower the level of attached gums, the higher the risk of recession (recession of the gums and exposed roots). When the level of attached gum is low, dentists often recommend performing special surgical operations on the gums, which can increase the level of attached gum and prevent exposure of the roots of the teeth.
Gum growth on wisdom teeth
There are situations when gums have grown on a wisdom tooth. And this is not related to the phenomenon of hyperplasia. If the third molar has only recently begun to erupt outward, one of its cutting edges has already appeared, and suddenly you feel pain, bad breath appears, and upon examination, inflammation, swelling of the soft tissues and their overhang over the tooth are discovered, then you probably have pericoronitis began.
Pericoronitis is an inflammation of the gingival hood over the third molar. The disease develops due to the fact that small pieces of food begin to get into the gap between the gum and the “eight” that has not fully penetrated, which rot because they are difficult to remove.
For more information about what pericoronitis is and how it is treated, read the feature article on the website.
If a broken tooth is healed
Situations where a tooth broken at the very root is overgrown with gums are not uncommon. It can break due to injury or collapse due to advanced dental disease. After this, many people are in no hurry to remove the root, and in some cases it gradually grows over from above (this process can last several years), and then does not bother or hurt for a long time. However, sooner or later, unpleasant sensations still appear: it becomes painful to chew, overgrown tissues swell and are constantly injured.
“My gums have grown on my back tooth, which broke off three years ago. I completely forgot about him, because... It didn’t give me any trouble, only sometimes after cleaning it would scavenge, but I didn’t attach any importance to it. All this was revealed during an examination at the dentist, when I went there with a completely different problem. In principle, the doctor decided everything quickly: he opened this growth and removed the root, then put stitches, but then it healed for a very long time and painfully. It was also very disappointing to hear that if I had contacted him immediately after the tooth was chipped, it could have been restored, but I immediately decided for myself that it was lost. That’s it!”
Varvara, review from 32top.ru
Remember that if a tooth is broken, then either its timely removal or restoration and prosthetics is necessary, because a serious inflammatory process can begin under the overgrown tissues or at the root, which can spread to the jaw, cheek, can develop deep into the body, lead to periostitis and osteomyelitis.
How long does the gum “grow” and the stages of development of hyperplasia
Pathology can develop slowly if it is caused by fibromatosis, epulis or fibropapilloma. And it can develop more rapidly if it occurs against the background of gingivitis.
As for the stages of development of hyperplasia, doctors identify the following:
- first stage: the gingival papillae thicken and thicken, while there are no other alarming signs,
- second stage: soft tissues grow and can cover up to half of the crown. Due to the volume, tissues are easily injured during oral hygiene and when chewing food, they can begin to bleed,
- third stage: the most rare stage. The tissues grow so much that they can even cover the cutting area of the crown. Granulations appear on the affected areas.
If you break off a tooth, gum growth may take several years.
Why does the gum move away from the tooth?
A prerequisite for the destruction of the periodontal attachment is the presence around the necks of the teeth - soft microbial plaque or supragingival tartar. The formation of dental plaque occurs due to irregular oral hygiene. In some patients with periodontitis, tartar may not be visually visible, because... when the attachment of the gum to the tooth is destroyed, it can already be localized below the level of the gum (then it is called “subgingival”).
But usually the destruction of the attachment of the gums to the teeth is always preceded by a long period of chronic inflammation of the gums, during which the patient is only bothered by periodic bleeding of the gums, possibly bad breath, redness or cyanosis of the gingival margin, as well as swelling of the gingival papillae. These symptoms are characteristic of gingivitis, an inflammatory disease of the gums in which the attachment of the gum to the tooth is not yet broken.
The lack of professional treatment for gingivitis (usually patients during this period self-medicate using antiseptic rinses and toothpastes for bleeding gums) leads to destruction of the attachment of the gums to the teeth. As a result, so-called periodontal pockets (gingival pockets) are formed between the teeth and gums, and patients in this case may complain that their gums have moved away from their teeth.
Stages of gum inflammation (gingivitis and periodontitis) –
Conclusions: Figure 10 shows the differences between gingivitis and periodontitis, and that with periodontitis, the gums are not attached to the teeth to the full depth of the periodontal pockets (from 3 to 6 mm or more). Therefore, if your gum has moved away from a tooth, there is simply no point in delaying a visit to the dentist, unless, of course, your goal is to remove these teeth in the near future. And in this case, there is no method of self-medication (magic rinses or ointments for gums) that would allow you to save the situation without going to the dentist.
In the absence of professional treatment of gums by a dentist, such teeth will first become mobile, then they will begin to fan-shaped and shift in different directions (under the forces of chewing pressure). In Fig. 11-13 you can see advanced forms of periodontitis in patients who, unfortunately, turned to the dentist too late. The teeth in these photographs have a very high degree of mobility and many of them only need to be removed.
Consequences of lack of treatment -
Signs and symptoms of hyperplasia
Those who have this problem rarely experience pain right away. But almost all patients notice a visual violation of the aesthetics of a smile, because the gums become voluminous and loose, which, as a rule, is the reason for visiting a doctor.
Discomfort and pain appear after the tissues have grown significantly, and they involuntarily have to be constantly injured during hygiene procedures and eating food. Another sign is the appearance of bad breath, which does not go away after careful hygiene or quickly returns again.
Consequences and complications if the pathology is not treated
Many patients see overgrown gums as only one problem – a significant disruption to the aesthetics of their smile. However, this is not so: if the pathology is not eliminated and it is allowed to progress further, then this is fraught with serious complications for the health of the oral cavity and the body as a whole.
If left untreated, the patient may develop degenerative diseases of periodontal tissues, leading to the destruction of the interdental septa and supporting ligaments that hold the teeth in the sockets. You may lose your teeth much earlier than you would like.
Hypertrophied tissues are subject to constant trauma, which is why any benign formation can sooner or later become malignant. Another common complication is osteoporosis.
For children, the lack of treatment is fraught with disruption of the formation, as well as the timing of the loss of milk and the eruption of permanent elements.
If a single growth appears on the gum, this may not always indicate hyperplasia or hypertrophy. Some people mistake the growth for a fistula, cyst, or abscess. If you do not consult a doctor in a timely manner for these pathologies, the purulent contents from these neoplasms can spread throughout the body, causing damage to the cardiovascular and circulatory systems, gastrointestinal diseases, sepsis and even a brain abscess.
Symptoms of gum recession
In dentistry, there are several types of receding gums, each characterized by its own symptoms, but the general symptoms of gum recession
are as follows:
- tissue volume decreases;
- bleeding during dental hygiene;
- there is swelling, redness of the gums;
- the molar root is exposed;
- there is a high sensitivity to temperature changes;
- caries may develop;
- eating food causes pain and discomfort;
Advanced cases include multiple cervical caries, discoloration of enamel, teeth are located at a far distance from each other. When teeth are exposed, food debris and plaque accumulate in the pockets. Purulent contents are released. The initial stage does not entail unpleasant symptoms, which is why most patients are unaware of the presence of the disease. To prevent gum recession, you need to visit the dentist every six months!
Methods of treating pathology in dentistry
The most common method of removing overgrown tissue is surgical excision using a scalpel or laser. Scientifically, this surgical operation is called gingivectomy. The procedure is performed under anesthesia.
About the indications, types and complications after gingivectomy - in the feature article on the website.
If there are few damaged tissues, then doctors may suggest their removal using cryodestruction, when under the influence of low temperatures they die off on their own over time.
If tissue proliferation is accompanied by an inflammatory process, then electrophoresis and darsonvalization may additionally be prescribed.
In addition to excision of excess tissue, treatment should be carried out aimed at eliminating the cause that provoked the development of the pathology. If the cause is a malocclusion, then the patient needs to see an orthodontist, who will prescribe devices to correct the position of the dentition. If there is a fragment of a tooth inside the overgrown gum, then it is necessary to remove it or use prosthetics, if the situation allows. In case of internal diseases of the body, the patient will be referred to specialized specialists - endocrinologist, gastroenterologist, cardiologist, etc.
Dentists are required to sanitize the oral cavity and remove hard and soft bacterial plaque.
Main stages of treatment
Since it is not always possible to determine the exact cause of the disease, treatment methods can affect different levels of the body:
- General strengthening therapy. Aimed at strengthening the body's defenses, replenishing the supply of important vitamins (C and P), normalizing the psycho-emotional state, and restoring metabolic processes.
- Local therapy includes relieving inflammation, cleaning the oral cavity from plaque and tartar. For this purpose, mouth rinses with antiseptics and special anti-inflammatory gels are prescribed.
- Surgical treatment involves incision and emptying of periodontal pockets, excision of granulation tissue, and removal of highly mobile teeth.
- Orthopedic methods are used to stabilize teeth with special splints or dentures.
Based on the clinical picture and advanced stage of the disease, as well as diagnostic data, the doctor prescribes several treatment methods. The treatment regimen necessarily includes professional cleaning of the oral cavity and local anti-inflammatory therapy.
Recovery period after surgery
If the gum has grown on the tooth, then now you know what to do - you need to contact a dentist who will prescribe adequate treatment.
Since treatment for hyperplasia involves surgical manipulation, there will be a recovery period after it, taking from 5-7 to 10-14 days. At this time, you need to follow all the doctor’s recommendations: take prescribed anti-inflammatory and wound-healing agents, rinse with antiseptics, and use painkillers as pain occurs.
During the rehabilitation period, it is important to exclude “irritating foods” from the diet: spicy and salty, cold and hot, solid foods. And, on the contrary, you need to diversify your diet with foods rich in vitamins C, E, B, A, calcium and phosphorus.
To care for the oral cavity, you need to use a brush with soft bristles and a non-abrasive toothpaste; you should avoid using an irrigator for a few days.
Prevention
Preventive measures are carried out in healthy people, as well as in patients after treatment. In order to reduce the likelihood of primary periodontitis or its relapse, it is necessary to follow some rules:
- Brush your teeth daily and thoroughly with a suitable toothbrush and toothpaste.
- Use additional products (dental floss, balms, etc.).
- Periodically have your mouth professionally cleaned at your dental clinic.
- Visit the dentist at least twice a year.
- Treat caries and other dental diseases in a timely manner.
- Try not to injure your gums.
- If gums become inflamed, painful or bleeding, consult a doctor immediately.
- Include vitamins and minerals in your diet.
- Lead a healthy lifestyle, give up bad habits.
These simple recommendations will help maintain the oral cavity in proper condition and prevent the development of many dental diseases, including periodontitis.
Is it possible to get rid of the problem on my own?
Some people use decoctions of medicinal herbs and plants (chamomile, oak bark, sage and others), as well as solutions to relieve gum inflammation (such as Chlorophyllipt or Stomatophyte) to get rid of the problem. However, you need to understand that hyperplasia cannot be cured by rinsing. This measure will not reduce the volume of overgrown tissue, but will help relieve signs of the inflammatory process and alleviate the condition during teething, and is also well suited as a concomitant therapy after surgical excision of excess gum tissue, which is carried out in a dental office.