Why does subcutaneous emphysema occur?
Chest injuries
Traumatic injuries to the chest organs are the most common cause of subcutaneous emphysema.
In closed injuries, air penetrates into the subcutaneous tissue due to a rupture of the lung. Most often, the integrity of the organ is violated during displaced rib fractures, when sharp bone fragments violate the integrity of the underlying tissues. Less commonly, a lung rupture occurs without accompanying skeletal trauma and is caused by partial separation of the organ from the root due to a fall from a height or intense horizontal impact, such as a car collision. Against the background of the rupture, a closed pneumothorax develops. With limited pneumothorax, there is little or no subcutaneous gas collection. In victims with a total form of pathology, air may spread throughout the chest. Sometimes gas moves from the chest to the neck and face.
Open pneumothorax is observed with stab, stab, and, less commonly, gunshot wounds of the lung. The severity of emphysema varies greatly. A particularly dangerous form of pathology is valvular pneumothorax - a condition when air enters the pleural cavity when inhaling, but does not leave it when exhaling. Continued injection of gas leads to progressive compression of the lung, displacement of the mediastinum, and the development of widespread subcutaneous emphysema.
Another possible cause of the symptom is thoracoabdominal injury. The same mechanism of air escape under the skin is observed as with isolated chest injuries. Distinctive features are the complex nature of the lesion, the high likelihood of traumatic shock and life-threatening complications.
Barotrauma
Lung barotrauma develops when using scuba gear or quickly ascending to the surface. Due to a sharp increase in pressure in the lungs, the alveoli rupture, air escapes into the tissue with the formation of subcutaneous emphysema in the chest and neck area. Chest pain, shortness of breath, frothy sputum with blood, cyanosis of the skin and mucous membranes are observed. Pneumothorax may occur. There is a risk of cerebral and cardiac embolism.
Subcutaneous emphysema
Facial skull injuries
An orbital fracture is accompanied by retraction of the eyeball, soft tissue swelling, and periorbital hematomas. Most often, the lower wall of the orbit in the area of the infraorbital foramen is affected. Palpation reveals sharp pain, a local soft crunch, indicating the presence of subcutaneous emphysema.
Injuries to the paranasal sinuses are manifested by severe local swelling, disturbances in nasal breathing, subcutaneous hemorrhages, and aching pain in the area of injury, which sharply increases with palpation. There is bloody discharge from the nose. Emphysema is detected in the affected area. After the edema subsides, an external defect becomes noticeable, caused by displacement of the bone wall of the paranasal sinus.
Subcutaneous emphysema is also accompanied by fractures of the nasal bones with rupture of the mucous membrane. The pathology is characterized by sharp pain, sometimes a crunching sound at the time of injury. Nosebleeds and rapidly growing swelling are observed, which is later complemented by cyanosis of the nose and lower eyelids. When the fragments are displaced, a violation of the shape of the nose is revealed.
Perforation of the trachea and esophagus
The cause of emphysema can be perforation of the trachea by a foreign body that accidentally enters the respiratory system (during pranks in children, holding small objects in the mouth in adults). The pathology is manifested by suffocation at the time of aspiration, a persistent paroxysmal cough, combined with lacrimation, vomiting, copious secretion of saliva and nasal mucus, and bluishness of the face.
Perforation of the esophagus also occurs due to small sharp objects entering the organ cavity. When swallowed, the patient feels pain, compression in the throat and along the esophagus. If the integrity of the esophageal wall is violated, acute pain that intensifies when swallowing, subcutaneous accumulation of air, and swelling of the soft tissues of the neck are noted. Sometimes pneumothorax forms.
Iatrogenic complications
Minor subcutaneous emphysema can be determined after laparoscopy and is localized in the adipose tissue around the punctures. The reason is the injection of carbon dioxide into the abdominal cavity to improve visualization and facilitate the movement of instruments. When injected, a small amount of gas may enter the surface tissue. The condition does not pose a threat and disappears on its own after a few days.
Incompetence of the bronchial stump develops within 1-3 weeks after pneumonectomy, lobectomy or bilobectomy; it occurs due to incompetence of the sutures and, as a consequence, air entering the pleural cavity, and fluid entering the trachea and bronchi. Accompanied by fever, shortness of breath, pain, cough with a large amount of bloody discharge. Subcutaneous emphysema may be detected in the chest, abdomen, face and neck.
During mechanical ventilation with high inspiratory pressure, patients develop barotrauma. The chest becomes barrel-shaped. The skin turns pale or becomes cyanotic and becomes covered in sweat. By palpation, a “creaking” is detected, caused by the accumulation of air bubbles in the subcutaneous tissue. Pneumothorax and pneumomediastinum are possible.
Other reasons
Other pathological conditions accompanied by subcutaneous emphysema include:
- Spontaneous pneumothorax.
It develops for no apparent reason or against the background of existing lung diseases. It occurs suddenly and is accompanied by sharp squeezing or stabbing pain. In severe cases, severe shortness of breath, fainting, tachycardia, pallor, acrocyanosis, and progressive emphysema of the upper half of the body are observed. - Mediastinitis.
The acute form is manifested by chest pain, hyperthermia, fever, chills, cyanosis of the skin, dilation of the veins of the neck, swelling and emphysema of the upper half of the body, neck, and face. Tachycardia, arrhythmia, hypotension, suffocation, dysphagia, dysphonia are noted. - Bronchial fistula.
The symptom is detected with bronchopulmonary fistulas against the background of purulent pleurisy. Complemented by severe shortness of breath, weakness, sweating, intoxication, cough with the release of a large amount of foul-smelling purulent sputum.
General information
Mention of such a concept as emphysema dates back to 1724. Dutch physician Herman Boerhaave noted a case of swelling in one patient. He noted that swollen areas have a characteristic crunching sound upon palpation. A little later, Rene Laennec described emphysema as a separate phenomenon.
Currently, this disease is not widespread. However, in medical practice, cases periodically arise when, after dental operations, complications arise in the form of emphysema in the oral cavity. The risks increase when using tools that operate under high air pressure.
Diagnostics
Diagnostic measures are carried out by a pulmonologist. In case of traumatic genesis of the symptom, the participation of a traumatologist is required; in case of facial lesions, consultation with a maxillofacial surgeon is necessary. During the collection of anamnesis, the specialist finds out what happened in the period preceding the formation of emphysema, identifies other complaints, and assesses the dynamics of the development of the disease. The following procedures are carried out:
- Visual inspection
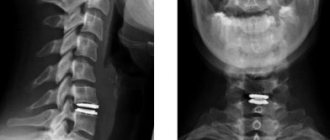
. The presence of subcutaneous accumulation of air is indicated by an uneven increase in the volume of soft tissues, sometimes creating the impression of “bloat”. Palpation is painless, a gentle crunch is detected by palpation. Possible lag of half of the chest in the act of breathing, expansion of the saphenous veins, and forced positioning of the patient. - Radiography
. In case of pathologies of the OGK, an overview photograph must be taken, and optionally a targeted one. It is possible to detect rib fractures, hemo- and pneumothorax, pneumomediastinum. For facial injuries, radiographs of the orbit, nasal bones, and zygomatic bone are taken. Sometimes an X-ray of the skull is required to rule out fractures of the brain. - CT scan
. CT of the OGK is performed to clarify the nature of the damage, identify atelectasis, pneumo- and hemothorax, and other pathologies, and is performed natively or with contrast. Patients may also have a CT scan of the lungs or a CT scan of the mediastinum. To detail the changes detected on X-rays of the facial bones, CT scans of the orbit and other studies may be prescribed. - Magnetic resonance imaging
. MRI of the lungs is informative in distinguishing between inflammatory and non-inflammatory lesions, studying lung tissue, vascular structures, the lymphatic system and fluid accumulations. Performed at the final stage of the examination as part of differential diagnosis and planning of thoracic interventions. - Endoscopic methods
. Suspicion of esophageal perforation is an indication for esophagoscopy. Tracheobronchoscopy is performed for tracheal perforation, bronchial fistulas, and other pathologies. In some cases, thoracoscopy is necessary to clarify the diagnosis and carry out treatment measures. - Other techniques
. Scintigraphy is recommended for assessing capillary blood flow and pulmonary ventilation; it is used for atelectasis, pneumonia, and obstructive pathologies. Pleural puncture allows you to determine the nature and amount of exudate in pleurisy, hemothorax and hydrothorax.
Subcutaneous emphysema on x-ray
Bullae in the lungs on CT
Bullae in the lungs on CT are visualized as distinct, relatively darker, bubble-like areas of lung tissue, resembling holes or large pores of a sponge. The denser the tissue, the lighter it appears on CT scans—so, for example, bones are white, but airy lung tissue is a relatively uniform graphite gray color.
Using a CT scan of the lungs, a radiologist can accurately determine the diameter of the bullae, their number, and find out whether there are signs of emphysema, bronchiectasis or other diffuse pulmonary diseases.
Treatment
Pre-hospital assistance
Victims with open chest injuries should apply a tight bandage to the wound area to transform an open pneumothorax into a closed one. Rib fractures should be fixed with a wide bandage of a towel or sheet placed on the chest during exhalation. To facilitate breathing, patients are transported in a semi-sitting position.
In patients with facial injuries, bleeding is stopped. Cold is applied to the affected area. If the person is conscious, he is transported with his head slightly tilted forward to avoid blood entering the respiratory tract. In case of impaired consciousness, transportation is recommended to be carried out in a lateral decubitus position. It is strictly prohibited to set fragments.
Conservative therapy
Air from fatty tissue is absorbed on its own, so subcutaneous emphysema itself does not require treatment. Therapeutic measures are aimed at eliminating the cause of the pathology and alleviating the patient’s condition. Patients with OGJ injuries are treated with fracture anesthesia or vagosympathetic blockade upon admission. According to indications, a pleural puncture is performed to remove air or fluid. The following medications are prescribed:
- Painkillers
. Analgin, ketorol and analogs are used orally or parenterally for severe pain. For intense pain, intramuscular administration of narcotic analgesics is possible. - Glucocorticosteroids
. Dexamethasone or prednisolone tablets are used to prevent the development or reduce the severity of the inflammatory process. For patients with barotrauma, medications are recommended to eliminate laryngospasm. - Antibiotics
. Drugs are necessary for all open injuries, as well as for the development of inflammatory and purulent complications. In patients with injuries, medications can be prescribed for preventive purposes in the first days. - Antitussives, expectorants
. Indicated to reduce pain caused by coughing, facilitate mucus discharge, and ensure complete drainage of the bronchial tree.
An obligatory part of the treatment of injuries and diseases of the acute respiratory tract is physical therapy, which allows you to quickly restore the normal functioning of the bronchi and alveoli. Exercises are performed from the first days after admission. The program is drawn up taking into account the patient’s condition and the severity of the pain syndrome. Breathing exercises are complemented by chest massage.
Forms of the disease
Based on the location and extent of the problem, three main forms of emphysema are distinguished.
- Limited. Affects a small area and is easily identified by palpation.
- Common. Air accumulation is noted just above and below the lesion.
- Total. Reaches incredibly large sizes and poses a threat to the patient's life.
Emphysema can be post-traumatic and iatrogenic. The first occurs with closed or open injuries. Iatrogenic is a consequence of dental procedures. The subcutaneous or submucosal form of the disease often occurs due to tissue injury during tooth extraction.