In modern medicine, various methods of examining the gastrointestinal tract are used. The most common is the endoscopic direction. Gastroscopy allows the doctor to visually examine the esophagus, intestines and stomach in real time, as well as take tissue samples for laboratory tests. However, this method is not painless. Patients often complain that their throat hurts both after FGDS and during the procedure.
Carrying out FGDS
The FGDS procedure lasts no more than ten minutes. If a biopsy is needed, it will take a little longer.
The patient is placed on his left side, after which the oral cavity and larynx are treated with a local anesthetic to reduce sensitivity.
A mouthpiece is placed in the mouth, through which the endoscopist inserts a tube with a probe. The doctor moves it deeper with gentle movements, examining the inner walls of the duodenum and stomach. If an ulcer or tumor is found, he will take a tissue sample for a biopsy. He will also remove detected polyps if necessary.
FGDS is a safe procedure, but in some cases it causes pain. Most often this occurs with ulcers or cancerous tumors. In these cases, the patient is recommended to undergo diagnostics under anesthesia.
How is rehabilitation after septoplasty?
With the development of technology, septoplasty has ceased to be uncomfortable. The operation begins with the patient being given anesthesia, then the doctor uses an endoscope, through a small incision, to enter between the layers of the mucous membrane and straighten the septum.
During the rehabilitation period, technologies were also created that allow the patient to avoid unpleasant sensations and breathe through the nose. Intranasal septal splints according to Reiter or splints were created. They are made of soft silicone, as it does not cause any harm to the nasal cavity and is painlessly removed from it. The splints have a seven-sided shape, which completely follows the shape of the nasal septum at the site of the operation. The essence of splints is that they keep the septum in the midline. After the operation, while the patient is under anesthesia, a silicone splint is sewn on.
Splints come in different modifications. Depending on the shape of the nose, they can be either large or small. A tube can also be inserted between the silicone of the splint, through which the patient can breathe immediately after the operation. The septal splint stays in the nose for about 5-7 days, during which time the nasal septum takes its position.
What to do if your throat or stomach hurts after FGDS
Painful sensations in the stomach after gastroscopy in the absence of ulcers and tumors disappear on the second day. For severe pain, it is enough to take painkillers.
Sore throat occurs due to mechanical damage to the walls of the larynx by the endoscope. In this case, it is recommended to talk less and gargle with solutions of furatsilin and miramistin. Rinsing with saline solutions is also allowed.
Painful sensations will be alleviated by taking sea buckthorn oil (2-3 times a day, a teaspoon). Combined with the healing effects of honey, this will help speed up your recovery.
Sprays are also successfully used, effective for sore throats and easy to use. They have a complex effect - healing, anti-inflammatory and antimicrobial.
Our clinic employs experienced endoscopists who can conduct an FGDS examination painlessly and without complications.
Septal splints
Recently, septal splints or intranasal splints have become an integral part of operations on the nasal septum. For septoplasty, rhinoseptoplasty and closure of perforations of the nasal septum, the final stage of the operation is the installation of septal splints on both sides of the nasal septum.
The reason splints are so popular among surgeons is a number of advantages that improve the outcome of the operation, reduce the risks of postoperative complications and speed up the patient’s recovery.
The advantages of septal splints are reflected in the table
| Traditional septoplasty method | Septoplasty using septal splints | |
| Nasal discharge | After the operation, the mucous discharge in the nose and the remaining blood dry up. Crusts form in the nasal cavity, which adhere to the nasal mucosa and are difficult to remove. They also impair breathing and cause severe discomfort in the patient in the postoperative period. | Septal splints cover the entire mucous membrane of the nasal septum and prevent the formation of crusts on the mucous membrane of the nasal septum. And due to the fact that they are made of silicone, all the pathological contents in the nose do not find adhesion and are easily washed off with a nasal shower. |
| Swelling of the mucous membrane | After surgery, the nasal mucosa begins to swell and close the nasal passages due to surgical exposure. Because of this, the patient cannot breathe through his nose, he has to breathe through his mouth, and thus develops dry mouth, etc. | Silicone splints prevent the nasal mucosa from swelling and closing, as they are very flexible and quite elastic. And thanks to special channels, the patient does not have breathing problems after the operation. |
| Adhesions in the nose | Often, upon a second visit to the doctor, the patient is informed about the formation of adhesions in the nose (synechia). The reason for adhesions in the nose is that the mucous membrane of the nasal septum, due to swelling, begins to come into contact with the mucous membrane of the lateral (opposite) wall of the nose, as a result of which they stick together, and the patient faces additional surgery. | Being a barrier between mucous membranes, splints help to avoid this complication. |
| Re-displacement of the septum after surgery | High risk of displacement. | Splints, like a plaster cast, applied to a broken limb, keep the nasal septum strictly in the midline and give it additional support. Thus, splints help to avoid such complications as a secondary displaced nasal septum. |
| Nose bleed | Frequent nosebleeds. | By holding the nasal septum tightly in the midline, the splints compress the vessels and blood does not accumulate between the layers of the nasal septum mucosa. Thus, frequent complications such as nosebleeds or hematoma of the nasal septum do not occur with installed splints. |
| Tamponation | Mandatory packing. Tampons in the nose create additional discomfort. | It is possible to avoid packing of the nasal cavity. Due to this, the rehabilitation period for the patient is easier. But it should still be remembered that only the surgeon decides whether to pack the nasal cavity or not, depending on the circumstances after installing the splints. |
Managing swallowing problems
Having trouble swallowing is called dysphagia. Your healthcare team can help you manage your dysphagia. Your team includes doctors, nurses, a swallowing specialist, and a clinical dietitian.
You will meet with a swallowing specialist before, during, and after treatment. This specialist:
- explain how treatment may affect swallowing;
- will teach you how to perform exercises to stretch and strengthen the muscles involved in swallowing;
- will monitor any changes in your ability to swallow as you progress through radiotherapy;
- will help you maintain your ability to swallow after treatment ends to prevent long-term or delayed changes.
Pain when swallowing
If you have pain when swallowing, your healthcare team will give you pain medicine to help you manage the pain. Follow your doctor's directions for taking your medication. If it doesn't help, tell your doctor or nurse. There are a wide variety of medications that can be used to relieve this type of pain.
Aspiration
If you have trouble swallowing, food or liquid may accumulate in the back of your throat. This increases the risk of aspiration. Signs of aspiration include:
- cough when swallowing;
- cough after swallowing;
- change in voice while eating or drinking.
If any of these signs occur, contact your swallowing specialist immediately. This specialist will assess whether your ability to swallow has changed and may recommend foods and drinks that are safe to swallow. You will also be given help with swallowing exercises to help prevent your ability to swallow from getting worse.
Call your doctor or nurse right away if you have any of the following symptoms:
- dyspnea;
- whistling when breathing;
- pain when breathing;
- cough with phlegm or mucus;
- temperature 100.4°F (38°C) or higher.
These may be signs of developing pneumonia or a respiratory infection.
Lockjaw
Trismus is a condition where you cannot open your mouth as wide as usual. Trismus can occur at any time, immediately after or even years after treatment.
If you cannot open your mouth wide enough, it will be difficult for your doctor to examine your mouth. This may also be due to other problems, for example:
- Irrigating the mouth and brushing teeth (oral hygiene), which can lead to bad breath, tooth decay and oral infections;
- chewing and swallowing, which may make it difficult for you to eat and drink;
- speech;
- kisses;
- insertion of a breathing tube, for example if you ever need general anesthesia (a drug given to keep you asleep during an operation or procedure);
- carrying out routine dental treatment.
When trismus occurs, its treatment is very difficult. This is why it is important to prevent trismus and treat the condition as early as possible. Your swallowing specialist will teach you exercises to help prevent trismus. It is also important to maintain good oral hygiene and good posture.
to come back to the beginning
About normal swallowing
Figure 1. Organs involved in swallowing
Many muscles and nerves work together to help you swallow (see Figure 1).
When you eat and drink, food and liquid mix with your saliva. Saliva softens and moistens food. Chewing allows you to break down food. When chewed, food and saliva form a bolus.
When swallowing, the tongue pushes food to the back of the mouth. After this, a reflex is triggered, and the root of the tongue pushes food into the esophagus. At this point, the larynx closes to prevent food or liquid from entering the airway (trachea). The food then passes through the esophagus and enters the stomach.
If the muscles in the mouth or throat are weakened, food and liquid can become stuck in the esophagus or enter the airways and lungs. Both of these situations can be dangerous.
The entry of food or liquid into the airways or lungs is called aspiration. Aspiration can lead to complications such as pneumonia (infection of one or both lungs) and respiratory infections (infections that affect the nose, throat, and airways).
to come back to the beginning
Endotracheal anesthesia - indications
In plastic surgery, endotracheal anesthesia is used for many operations.
Examples include rhinoplasty, augmentation mammoplasty, abdominoplasty, mastopexy, circumferential facelift and SMAS platysmaplasty. Liposuction can also be performed using an intubation technique, although local anesthesia may be chosen for smaller cases. Endotracheal anesthesia is indicated for all long-term operations accompanied by a violation of the integrity of deep tissues, not only the skin. This is how a general rule can be formulated. Minor surgical interventions are often performed under local anesthesia. Examples are otoplasty for protruding ears, bullhorn (a type of lip surgery) or lipoma removal.
How is endotracheal anesthesia performed?
Preparation for surgery consists of several stages. The preparatory stage is premedication. Before surgery, the patient is given sedatives - tranquilizers, drugs with anxiolytic effect. Taking sleeping pills the evening before surgery is also part of the preparatory phase. Thanks to premedication, a person approaches surgery in a calm and balanced state.
Immediately before the operation, induction anesthesia is performed - intravenous administration of sedatives, which ensures smooth falling asleep before intubation begins. The next stage is muscle relaxation. When the patient falls asleep, he is given a small dose of muscle relaxants - drugs that help relax the muscles. Thanks to muscle relaxants, the tone of the laryngeal muscles is reduced and optimal conditions are created for the insertion of an endotracheal tube.
The fourth stage is the direct insertion of the endotracheal tube and its connection to the ventilator. At this stage, the patient is already sleeping and dreaming, and nothing bothers him.
How to relieve toothache during a cold
There are a hundred ways to relieve toothache, but only a dozen methods will be effective. Common control options include:
- non-steroidal anti-inflammatory drugs (NSAIDs) . When people have a cold, they resort to Fervex, Theraflu, Antigrippin and other drugs containing paracetamol. So why not replace the old and harmful paracetamol with a modern, soft and effective nimesulide or meloxicam? Both of the latter substances easily reduce temperature, block pain and fight inflammation;
- local anesthesia . Novocaine or lidocaine is applied to a cotton swab and applied to the diseased area. A sophisticated method suggests crushing 1 tablet of No-shpa (drotaverine) and pouring the resulting powder onto the affected area in the mouth. In both cases, the treated area becomes numb for 2-3 hours;
- traditional methods . The pulse is found on the arm on the opposite side and a clove of garlic is tied. The mechanism is not clear, but the pain subsides;
- warming up The method is effective, but dangerous: purulent inflammations cannot be heated, because this provokes the melting of surrounding tissues by pus enzymes. And only a doctor can tell about the nature of the inflammation.
The listed methods only relieve symptoms, which shortens the time of an attack of acute pain, but do not treat teeth.
And one last thing. Toothache only seems like a trifle at first - people endure it for days because of fear of dentists - but it is fraught with many dangers, just like a cold that is not cured in time. Take care of yourself and take care of your health. You are alone!
Moscow metro station Zvezdnaya, Danube Avenue, 23
What can and cannot be done after tooth extraction
- What to do after tooth extraction
- What to do after wisdom tooth removal
- What not to do
- What do we have to do
- What to do after tooth root removal
- Baths after tooth extraction
- What to do after a child’s tooth extraction
- What to do after removing a tooth with a cyst
- Temperature rises after tooth extraction
Tooth extraction is a major dental operation.
The recovery period after such a procedure can take some time and last from three days to seven days. There are indications and contraindications for what measures the patient needs to take to ensure that the rehabilitation process goes as quickly and successfully as possible. If you strictly follow the dentist’s recommendations and the general rules of the postoperative period, you can significantly bring the moment of recovery closer and avoid unpleasant or even dangerous complications. Rules of conduct during recovery after a doctor has pulled out a tooth may differ depending on the severity of the operation performed, its type, the general health of the patient, his habits and age. However, there are general recommendations that are relevant for any postoperative situation.
Science and clinical practice
I will try to tell you about the effect of anesthesia on the human body, and in particular on the brain.
Anesthesia is a state of loss of consciousness that is induced artificially and is characterized by its reversibility. Anesthesia produces pain relief, which allows it to be used in surgery to relieve the patient of the suffering associated with the sensation of physical pain. The state of anesthesia is achieved with the help of anesthetics; there is a certain medical specialization - an anesthesiologist who selects the optimal dose and combination of drugs based on the individual characteristics of the patient’s body, in addition, the type of medical effect matters. It often happens that anesthesia causes fear in people to a large extent more than the surgical operation itself. Among other things, there are many rumors and rumors about anesthesia; some fear that anesthesia can cause death. Is it really? How does anesthesia affect the human body? Is it dangerous, will anesthesia affect further memory problems and cognitive functions of a person?
I don’t want to offend anyone, but very often I hear amazingly illiterate and ignorant statements about anesthesia on this subject, not only from ordinary people, but also from doctors, but almost any non-anesthesiologist will be happy to tell you thoughtfully something like “anesthesia is always anesthesia” or “Anesthesia is not candy.” It’s good that at least the majority do not repeat the generally accepted nonsense that “anesthesia takes 5 years of a person’s life” or “affects the heart.” Patients who undergo operations under general anesthesia write with pleasure in various forums how afraid they are of “general anesthesia,” and a chorus of well-wishers echoes them: “yes, yes, anesthesia is like dying a little,” “anesthesia has a lot of contraindications,” “maybe allergic shock!” It seems that you can do without anesthesia and there is no need to monitor the patient’s somatic condition during the most complex and traumatic interventions. True, no one writes that pain has a very, very strong effect on health, that not everything can be tolerated.
Most of us know about anesthesia that it is used during operations as an anesthetic; this is where our knowledge ends and fears, worries, and speculation begin. General anesthesia, or anesthesia, is a time-limited state of unconsciousness during the administration of special painkillers, during which time the patient undergoes a surgical operation, after which the patient’s consciousness is restored. The actions of the anesthesiologist are aimed at relieving the patient of pain during the operation, as well as to ensure a normal and painless transition to a state of consciousness, with no discomfort.
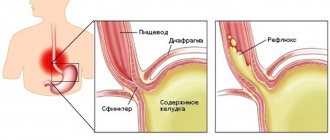
How general anesthesia affects the human body should be discussed based on what type of anesthesia is used. General anesthesia is divided according to several criteria, but again we will not go deeper, but will only name and characterize the main types used in practice. For major operations on internal organs located above the diaphragm, which separates the chest cavity from the abdominal cavity, anesthesia with artificial ventilation of the lungs is usually used, and, in heart operations, with artificial circulation. Anesthesia drugs can be administered either intravenously or through inhaled air, or both. Sometimes such anesthesia is also supported by spinal (subdural) or epidural anesthesia, which, in turn, can be used independently. During spinal anesthesia, the drug is injected under the dura mater into the fluid that washes the spinal cord at the level of its segments responsible for sensitivity in the surgical area. For the duration of the anesthetic, these segments and all those located below them become insensitive to pain, and the anesthetized parts of the body become immobile. With epidural anesthesia, the drug that causes it is injected above the dura mater, at the level of the nerve trunks extending from the spinal cord and, washing them, causes an interruption of sensory and motor nerve impulses at the site of action of the drug. Organs located below the operation site may not be anesthetized. Both types of such anesthesia are considered gentle: they are the least aggressive and have the advantages of general and local anesthesia, while practically not having their disadvantages. Epidural anesthesia can also be prolonged. In this case, a thin catheter (tube) is placed over the dura mater and brought out. It is glued to the patient’s back and painkillers are added there: this postoperative pain relief is the most effective. These types of anesthesia require a very small amount of a drug from the group of local anesthetics; until recently, pain relief was done with lidocaine, but now drugs have been proposed that act longer and are more effective in smaller doses.
The anesthesiologist chooses the type of anesthesia based on the individual characteristics of the person being operated on; the choice depends on his physical condition, on what kind of operation is being performed, and even the level of qualification of the surgeon and the anesthesiologist himself matters. In order to perform the same operation on different people, different types of anesthesia can be applied to them; the ideal combination of drugs is selected for the patient, which is achieved by mixing different drugs and types of pain relief. Thus, the importance of a specialist anesthesiologist is extremely difficult to overestimate; this doctor is always present during all major operations.
People who have undergone surgery, and therefore general anesthesia, report the following symptoms and unpleasant moments after the use of painkillers:
Firstly, memory impairments are possible, which can manifest themselves in different ways, from subtle isolated cases to regular and pronounced ones that arise suddenly.
Secondly, after using anesthesia, some note sleep disturbances, which can persist even several months after the operation.
Thirdly, immediately after surgery, the use of anesthesia can cause headaches, hallucinations, hearing and speech disorders. All these symptoms, as a rule, disappear within the next few hours after the application of anesthesia.
And this is not a complete list of troubles that can be caused by the use of anesthesia, as people who have suffered it say.
Now let's talk about the effect of general anesthesia on the brain:
Some of the consequences of anesthesia are memory impairment, decreased attention, and deterioration in learning ability. The disorders described above in medicine are called postoperative cognitive dysfunction. Memory impairments observed after anesthesia always cause a lot of trouble for patients. Patients are concerned about what happened to their memory after anesthesia, how long it will last, and what can be done to alleviate the condition. As a rule, anesthesiologists cannot give clear answers to the questions posed above. Memory impairment after anesthesia is not such a rare complication. Most studies regarding post-anesthesia memory impairment have focused on cardiac surgery. It has been shown that during the first week after anesthesia, memory impairment occurs in 30-80% of cardiac surgery patients. Patients who have undergone non-cardiac surgery are at slightly lower risk of developing memory impairment after anesthesia. Thus, in the first week after anesthesia, a decrease in memory and attention is observed in 25% of patients, and after 3 months – in 10% of patients. There are studies that show that after undergoing anesthesia, cognitive disorders can persist for a year or more.
Scientists have not reached a consensus on which type of anesthesia has the least effect on the brain. According to some, disorders of cognitive functions such as memory, attention and learning occur with the same frequency, both with general anesthesia and with regional methods of anesthesia (spinal anesthesia; epidural anesthesia). Others have concluded that regional anesthesia is associated with fewer incidents of memory and attention impairment.
There is no clear answer regarding the harmfulness or harmlessness of individual anesthesia drugs. It is believed that sharp changes in the delivery of oxygen to the brain are important in the development of memory impairment during anesthesia. During anesthesia, it is possible to develop certain conditions that are associated with the development of temporary oxygen starvation of the cerebral cortex. These conditions are associated with a significant drop in blood pressure and a marked decrease in oxygen levels in the blood.
Despite the fact that the causes of post-anesthesia intellectual impairments continue to remain unclear, scientists have found a number of factors that increase the risk of developing attention and memory impairments after anesthesia: older age, repeated anesthesia, long-term surgery, low level of education of the patient, and those that developed after surgery. infectious and respiratory complications.
In order not to scare potential patients, as a neurosurgeon I can say that often all problems with memory and cognitive functions are reversible! There is a sufficient arsenal of tools to solve this issue, which in most cases will help not lead to the development of complications or will help restore lost functions as quickly as possible.
The most important thing I want to say in conclusion is that, of course, the risk of anesthesia and the volume of surgical intervention are always assessed. You always need to make a CHOICE!
The choice is of course yours, but after an explanation from the TEAM (anesthesiologist and surgeon) about the development of possible pros and cons - and the occurrence of possible complications.
By the word TEAM I mean a well-coordinated team (anesthesiologist, surgeon, nurses) who work in one direction - for the benefit of the patient with a good quality of life!
Impact on biological tissues
When ionizing radiation enters a cell, it causes the chemical bonds in substances to break, causing the cellular structures to stop doing their job properly. There are no structures in the cell that are resistant to radiation, although their susceptibility to it differs, and the severity of the changes depends on the radiation dose.
One of the leading causes of cell death is damage to the genetic apparatus. In some cases, the cell dies immediately, in others it tries to recover, but DNA damage leads to the fact that its offspring also die after several division cycles. However, if the radiation dose turned out to be insufficient for pronounced changes, the cell is completely restored after 2-6 hours.
The most sensitive to the effects of radiation are those cells that are in the process of dividing. This allows the use of radiotherapy in the treatment of cancer: growing tumor cells are more susceptible to the harmful effects of radiation than healthy tissue.
Most malignant neoplasms are highly sensitive to the effects of radiation, so in countries with developed medicine, more than half of cancer patients undergo radiation therapy at one stage or another. The percentage of such patients is gradually increasing, since modern medicine makes it possible to implement the main principle of radiotherapy - delivering a large dose of radiation to the tumor, protecting healthy tissue from damage. New methods of external radiotherapy significantly reduce the radiation dose to the patient, ensuring better tolerability of treatment. It is impossible to protect healthy tissues from ionizing radiation 100%. Therefore, some patients may experience certain complications after radiation therapy.