In orthopedic dentistry, a crown on a tooth made of zirconium dioxide is considered one of the best means of prosthetics. Before its appearance, the integrity and aesthetics of the dentition were restored mainly with the help of porcelain and metal-ceramic structures.
Both had certain disadvantages. Therefore, specialists and patients gradually began to request new dentures that would not be susceptible to chipping, had high strength and looked as natural as possible on the teeth.
Eventually, a material that met these requirements was found, after which it began to be widely used in dental prosthetics.
What is zirconium dioxide?
The name “zirconium dentures” is often used in everyday life by patients and dentists. But, strictly speaking, it is not entirely correct. The correct term is “zirconia crowns.” The material from which such structures are made is a refractory oxide of the chemical element – Zirconium metal. To stabilize this compound, yttrium and aluminum oxides are used. After preliminary sintering of such material, a milky-white blank is obtained, from which a dental prosthesis is formed by mechanical processing on special milling equipment.
Manufacturers rating
The blocks are produced by different companies and can differ significantly in aesthetic parameters and quality. Classic milling discs are not transparent and are completely white. Some manufacturers have launched pre-colored zirconium blocks on the market, characterized by a beautiful natural color and a smooth shade change from the cervical area to the incisal edge of the tooth. The rating is based on reviews from doctors, scientific studies, and articles in leading dental publications. So:
- Katana® UTML (Japan). The material produced by this company makes it possible to make dentures that are not inferior to ceramics.
- Prettau® Anterior (Germany).
- Bruxzir® (USA).
Material advantages
Zirconium dioxide is superior in many respects to other materials used for prosthetics. It makes it possible to obtain crowns that:
- They have a small thickness. Unlike metal-ceramic prostheses, zirconium oxide crowns are thin-walled. Therefore, there is no need to grind down a large amount of dental tissue under them. And, accordingly, depulpation is not required, that is, the tooth remains alive.
- They fit as accurately as possible to the supporting part. In the manufacture of such crowns, computer modeling technologies are used, so the dentures fit tightly and hermetically to the gums, and bacteria do not penetrate under them.
- They look natural. Zirconium dioxide is distinguished by such properties as light conductivity and transparency, which corresponds to the characteristics of natural enamel. Therefore, crowns made from it are very similar to real teeth.
- Biocompatible with body tissues. Zirconium dioxide does not cause irritation in the oral cavity, does not provoke allergic reactions and does not stain the gums in the area adjacent to the crown.
- They do not chip or crack. Such crowns are so strong that they can even be installed on chewing teeth, including as part of bridge structures.
- They do not lose their original characteristics over time. With proper care, even after several years of use, dentures retain their color and shine.
Manufacturing and fixation of a partial zirconium denture
High-strength ceramic materials are becoming increasingly in demand in dental practice. Metal-ceramic crowns are essentially two-layer restorations that are supported by a metal coping or similar substructure and lined with a more aesthetic material, ceramic. The introduction of zirconium dioxide has made it possible to replace metal caps with more aesthetic and equally durable analogues, and although zirconium itself is more opaque, the use of more transparent feldspathic ceramics in the structure of partial dentures for veneering such restorations helps to easily solve this problem.
According to one systematic review of publications from 2006 to 2013, which analyzed 67 clinical studies and 4663 cases of metal-ceramic crowns and 9434 cases of all-ceramic single restorations, it was possible to establish the following: the five-year success rate of metal-ceramic crowns is 95.7%, leucite-reinforced and lithium disilicate – 96.6%, and lined with zircon – 91.2%. Ceramic chips occurred with almost the same frequency in both metal-ceramic crowns and those with a zirconium base, and the rate of such complications over 5 years did not exceed 2.6%. However, fracture of the zirconium base was extremely rare - only 0.4% of cases over 5 years. At the same time, loss of retention of zirconium structures was observed in almost 4.7% of situations. On the other hand, tooth fractures and their iatrogenic devitalization were most often observed when using metal-ceramic structures, and amounted to 1.2 – 1.8%.
From a biological point of view, all-ceramic crowns perform better than their metal-ceramic counterparts, as indicated by the higher rates of fracture of abutment teeth with loss of vitality when using structures supported by a metal cap. The high strength of zirconia has generated considerable interest in its use as a load-bearing structure in the manufacture of fixed partial dentures.
One systematic review, which included 40 clinical studies and analysis of 1796 metal-ceramic and 1110 all-ceramic bridge structures, found that the survival rate of such restorations was 94.4% and 90.4%, respectively. That is, no significant differences were observed between the 5-year success rates of different types of restorations. Fractures of bridge-like restorations made of glass-ceramics (8.0%) and ceramics based on silicon-aluminum compounds (12.9%) occurred significantly more often compared to metal-ceramic (0.6%) and densely sintered zirconium structures (1.9%). Thus, it is clear that the incidence of ceramic chipping and loss of retention was observed more frequently in zircon-supported restorations than in metal-supported restorations.
Clinical trials with zirconia have shown that, despite a relatively low rate of cap fracture, these restorations are generally more susceptible to porcelain chipping than metal-ceramic bridge restorations. Further development of zirconium materials has helped improve their color rendering and transparency, which has taken them to a new aesthetic level. In addition, CAD/CAM technology has advanced significantly, allowing laboratories to fabricate monolithic restorations without the need for subsequent layering of feldspathic ceramics. Monolithic zirconium oxide has become a popular material for the manufacture of crowns for distal teeth and as part of fixed bridge structures. However, the volume of necessary research remains insufficient to draw definitive and reasoned conclusions.
A recent clinical study comparing the performance of CAD/CAM metal-ceramic (12) and all-zirconia (10 lithium disilicate and 10 zirconia) restorations demonstrated that there was no significant difference in the volume of gingival fluid released into the sulcus across all restorations placed. and the patients’ own control teeth. The study was carried out 1 and 6 months after fixation of the structures. During the laboratory production of metal-ceramic and zirconium crowns, an iTero scanner (Align Technology) was used, and for lithium disilicate restorations, an E4D scanner (Planmeca/E4D Technologies) and an E4D milling cutter (Planmeca/E4D Technologies) were used. It has been noted that zirconia crowns have the lowest level of horizontal margin discrepancy.
Another study that recorded the fracture rate of monolithic zirconia restorations based on data from two commercial dental laboratories found the fracture rate to be 0.99% for distal monolithic restorations and 2.06% for anterior restorations. areas. In total, 39,827 aesthetic designs were analyzed in the study. However, this study may have been flawed because it is likely that not all dentists returned broken crowns back to the laboratory. Previously, the production of zirconia restorations took a lot of time due to the cost of processing and sintering the crowns, but the introduction of a new induction furnace for ceramics (CEREC Speedfire, Dentsply Sirona) has made it possible to practically transfer the entire fabrication process to the clinical office, which was previously considered almost impossible. Not only does zirconia have special physical properties, but the use of such restorations also provides a more conservative approach to the preparation of abutment teeth during a single visit.
This article presents a clinical case of the manufacture of a 3-unit zirconium bridge structure during one appointment day by a dentist.
Clinical case
A 57-year-old patient presented to the dentist in October 2015 for an endodontically treated maxillary first molar (tooth 14) with a root fracture (Figure 1).
Photo 1. X-ray before treatment: vertical fracture of the root of the 14th tooth.
The patient was about to start chemotherapy and needed immediate tooth extraction due to existing pain and possible risk of infection. After he completed chemotherapy in May 2016, he again contacted the dentist with a request to restore the existing defect. Previously, the patient had solid gold bridges installed on teeth 18 to 20 and teeth 29 to 31. Despite the fact that the doctor proposed to replace the existing dentition defect with an implant, the patient refused surgical intervention and wished to restore edentia with the help of a bridge, since he was completely satisfied with the existing similar structures.
Since full crowns had already been installed on the teeth adjacent to the defect (teeth 13 and 15) (photo 2), the dentist agreed to perform prosthetics. Full crowns made of zirconia were chosen as superstructures, characterized by their high flexural strength and fracture resistance. In addition, such structures can be fixed using the classical algorithm using composite cement. Despite the fact that zirconium restorations are not as aesthetically pleasing as some glass-ceramic structures, the patient was primarily interested in the functional parameters of the crowns rather than their appearance.
Photo 2. View of the extraction area after healing.
Of course, the doctor could choose zirconium crowns with ceramic veneers as an alternative restoration option, but in this case the risk of chipping in the long term increases significantly. The selected all-ceramic designs provide both predicted reliability of restorations and significantly reduce the risk of chipping under the influence of functional loads. After removing the previous restorations from teeth 13 and 15, the doctor did not find any significant structural changes or caries in the area of the supporting units of the dentition (photo 3), so he only slightly refreshed the stumps using medium and fine abrasive burs (Meisinger USA).
Photo 3. Fairly good condition of the supporting teeth after removal of the previous structures.
Despite the fact that preparation for zirconium oxide structures may not exceed 0.5 mm, in this case the total amount of tissue reduction along the load-bearing walls of the teeth was about 1.0 mm. Retraction was then performed using No. sutures. 1 Ultrapak (Ultradent), and the preparation area was scanned (CEREC OmniCam, Dentsply Sirona) with further analysis of the resulting image in the CHAIRSIDE CEREC 4.4.3 software (Dentsply Sirona) (photo 4).
Photo 4. Visualization of the preparation area and determination of the edges of future structures.
During the analysis, we used the Biojaw biostatic algorithm built into the program, which helped to comprehensively evaluate the entire digital jaw model. Thanks to this step, it is possible to recreate the primary restoration models, which, after only minor corrections, are then suitable for the successful subsequent milling of superstructures (photo 5).
Photo 5. Bridge design.
CEREC Zirconia (Dentsply Sirona) was chosen as the working material due to its high strength and color characteristics. Milling was carried out on an inLab MC X5 machine (Dentsply Sirona) using carbide burs (Shaper 25/Finisher 10). The dry milling technique ensures excellent integration of the edges of the restoration due to the detail of all elements of the restoration, and also helps to reduce work time, since it eliminates the stage of drying the structure (photo 6).
Photo 6. Milled zirconium.
The total milling time for the 3-unit bridge was 29 minutes. Correction of parafunctional habits that provoked pathological abrasion of the frontal group of teeth was not carried out, since the effect remained unchanged over the past few years, and the patient himself did not show any desire to treat this pathology.
During the treatment, the patient used a night guard in order to prevent possible damage to the structure of the supporting teeth, and polished zirconium restorations are characterized by significant resistance to abrasion, which guarantees a long-term result of their functioning. Data from some laboratories indicate the possibility of abrasion of antagonist teeth by zirconium, which was also confirmed in separate clinical studies. This effect is observed if the surface of zirconium dioxide is simply glazed after milling. During milling, the zirconium becomes rough, and after applying the glaze, the areas between the roughness are simply filled in. During operation, the more delicate structure of the glaze quickly wears away, exposing the rough zirconium interface, which provokes abrasion of natural antagonist teeth. To prevent this complication, the zirconium surface can be polished, which significantly reduces its abrasive effect. Laboratory studies have shown that polished zirconia causes the least abrasion of opposing tooth enamel, glazed zirconia the most, and polished and then glazed zirconia to be somewhere in between the two. A systematic review including analysis of 62 studies confirmed that, regardless of production algorithm, the least abrasion of enamel was observed when using polished zirconia, and the glaze, which wears off over time, does expose the hard and rough surface of the structure. Therefore, polishing the ceramic before glazing helps to minimize the effect of abrasion on opposing teeth. After removing the sprue (Universal White Polisher 9613V-220), a fine diamond bur at up to 5000 rpm (863-016) was used to contour the anatomy, as well as a pink polisher (9771F-170) to ensure a smooth occlusal surface. This stage also helps to recreate a smoother surface of the restorations after glazing, which also has a positive effect on minimizing the risk of abrasion of the enamel of antagonist teeth (photo 7).
Photo 7. Contouring before sintering.
Even if the surface is pre-polished before glazing, the effect after sintering helps to increase the flexural strength parameters. Since high-strength zirconium oxide can be quite opaque, it is advisable to infiltrate appropriate liquids to ensure optimal shade parameters of restorations and ensure high parameters of their esthetics. In this case, Incisal Blue and Violet Color Liquids Prettau Aquarell (Zirkonzahn) and Okklusal Amber (Whitepeaks Dental Solution) solutions were used for infiltration (photo 8).
Photo 8. Infiltration before sintering.
The structure was then ready for sintering and placed occlusally down in the CEREC Speedfire oven (Dentsply Sirona) (photo 9).
Photo 9. Preparing the bridge for sintering, positioning with the occlusal surface down.
The use of ceramic balls in this oven is not necessary, as its mechanism of action is based on patented induction technology, which provides energy-efficient heating cycles based on the volume and shade of the ceramic. Single crowns are typically sintered in less than 15 minutes, and bridges in approximately half an hour. After sintering and cooling (photo 10), the restoration is manually polished to a mirror finish (photo 11).
Photo 10. View after glazing and cooling.
Photo 11. Polished bridge structure.
For this, the author prefers to use Meisinger Twist polishers (green, blue, and pink) at speeds less than 11K rpm. This approach helps to reduce the abrasive effect of zirconium restorations below the level of feldspathic ceramics and equate it approximately to the level of abrasion of gold alloys. After polishing, paints and shadows can be applied to the zirconium in order to improve the final aesthetic parameters of the restorations and closely mimic the appearance of natural teeth. Dentsply Sirona manufactures special CEREC Speedfire glaze pins (Figure 12) that hold the restoration in place during the second 7-minute sintering cycle (Figure 13).
Photo 12. Pin for glaze.
Photo 13. Restorations after the second 7-minute glazing cycle.
In this case, GC Initial IQTM Luster Pastes (GC America) and IPS Ivocolor (Ivoclar Vivadent) were used for touch-up. CEREC Speedfire is the first furnace to simultaneously glaze and sinter zirconia and other glass-based ceramics. The final appearance of the structure is shown in photo 14.
Photo 14. Final appearance of the restorations before cementation.
The advantage of monolithic zirconium oxide is its ability to be fixed using the classical algorithm or by adhesive fixation, depending on the characteristics of the preparation. In this case, cementation was performed using composite-modified glass ionomer cement (FujiCEMTM 2). High-strength zirconia is also the material of choice for restorations due to its flexural strength in relation to the dimensional parameters of the bridge structure (Figure 15).
Photo 15. The final appearance of the restorations in the oral cavity.
This approach may result in slight discrepancies in shadow or color relative to the patient's adjacent teeth. To address this aspect, more translucent zirconia options continue to be developed, which will help solve the problem of optical mismatch of crowns. Samples of such materials, however, require a longer sintering cycle, which can last about 8 hours.
All-zirconia restorations do not have the same light transmission as natural tooth structures and also significantly increase the shade, but these clinical aspects were not critical in the described clinical case.
conclusions
With the introduction of CEREC Speedfire and dry milling capabilities, the production of monolithic crowns, abutments and 3-unit bridges has become possible right in the dentist's office. These procedures can be performed in one visit, thus expanding the indications for the use of CAD/CAM technology in everyday dental practice.
Authors: Mike Skramstad, DDS Dennis J. Fasbinder, DDS, ABGD
Who is suitable for zirconium crowns?
In each case, different materials may be suitable for prosthetics. So, if we consider zirconium crowns, then these reliable and aesthetic prostheses are suitable for restoring teeth in any part of the row, including chewing units. They are also suitable for installation in the smile area. To achieve the effect of a natural tooth, crowns that replace incisors are covered with a porcelain layer and painted in the color of natural enamel.
Indications for the use of zirconium dioxide prostheses may also include a patient’s tendency to be allergic to metal, loose gums, and increased tooth wear. Another argument for this particular choice is the desire to keep the abutment tooth alive and minimally ground. This is not possible when using metal-ceramic structures.
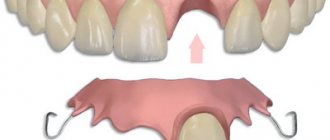
Zirconium crown for complete tooth loss
If the patient has completely lost a tooth, we recommend restoring it with a crown on an implant. This option is much more aesthetically pleasing and functional than a bridge on adjacent supporting teeth. Dentures on an implant are more expensive than a bridge. However, the adjacent teeth will remain healthy, the implant will fully perform the functions of a tooth root, and the volume of bone tissue around it will be preserved.
First we perform implantation. If we are talking about the smile area, then a temporary prosthesis will be made before the tooth is removed. The installation of the implant takes place in two stages, which can take 5-6 months. A long period can be attributed to the disadvantages of prosthetics on implants. However, you will get the highest quality result - you will be able to chew any food.
When the implant has completely taken root, we will fix the crown on it using an abutment mount and a miniature screw, which is then covered with filling material.
How are zirconium crowns made?
To produce dentures from zirconium dioxide, CAD/CAM technology is used, which is the modeling and manufacturing of products using computer programs.
The entire process from preparation to installation of zirconium crowns consists of several successive stages:
- Taking dental impressions at the dentist's office.
- Creation of a three-dimensional model of the future prosthesis on a computer.
- Designing a 3D model of the crown, and “trying it on” here, in a computer program.
- Sending digital information to a special milling machine, on which the frame of the future prosthesis is machined.
- Applying veneering ceramic mass to the base of the crown if it is used to restore the front tooth.
- Baking the prosthesis to achieve a strong connection between the ceramic layers and the frame.
- Grinding and polishing of finished crowns.
If a zirconium dioxide structure is machined “in full anatomy,” that is, subsequent veneering is not expected, then the milky-white prosthesis is treated with special dyes before final sintering. After this, it takes on a more natural look.
How much and how does addiction take place?
Prosthetics with zirconium crowns does not imply any special rehabilitation. After the procedure, the patient is able to carry out daily activities without restrictions. Eating food is possible after 2 hours, liquids - after 10-20 minutes. During the period of adaptation to crowns, the following sensations may occur:
- tongue/cheek biting;
- problems with diction;
- discomfort in the jaw muscles;
- insomnia;
- increased salivation;
- dry mouth.
To quickly get used to crowns, it is recommended to use dental gels, engage in muscle exercises, talk more, and follow a diet that excludes viscous and hard foods.
Possible problems:
- discomfort. A foreign body in the mouth sometimes bothers the patient, after 10-14 days the discomfort goes away, but if the discomfort does not disappear, it is better to consult a doctor - the orthopedist will replace the product or adjust its height;
- reaction of the front teeth to cold/hot. Excessive sensitivity after treatment indicates a loose fit of the crown to the cervical segment of dentin;
- pain. If pain persists for more than 5-6 days, you should consult a doctor - hygienic cleaning or root canal treatment may be required.
Life time
Crowns and bridges made of zirconium dioxide last the longest of all similar structures. This material is 30 times stronger than ceramics, so dentures made from it can last 15–20 years, and this period is not the limit either. But to extend the period of use of such crowns, you need to properly care for them and not test their strength by cracking nuts or candy with your teeth. In addition, it is important to regularly visit the dentist for preventive examinations and check the condition of the supporting units, which also determines the service life of the dentures installed on them.
Causes of complications
Complications after crown prosthetics are associated with general diseases, errors in the clinical process, and insufficient sanitation of the oral cavity.
Consequences of installation:
- crown deformation;
- development of inflammation;
- formation of carious cavities;
- poor quality fixation;
- change in bite;
- infectious tissue damage.
If there is intense pain or an unpleasant odor, the crown will have to be removed and further treatment tactics discussed with the attending physician.
Care of zirconium crowns
Zirconium dioxide dentures should be cleaned in the same way as your own teeth:
- do this twice a day - after sleep (breakfast) and evening meals;
- you can use regular toothpaste and a medium-hard brush;
- Use dental floss to clean contact surfaces.
To maintain the pleasant color and shine of the crowns, after each meal it is useful to rinse your mouth with at least plain water. In addition, at least once a year you need to visit the dentist to check the condition of your teeth and prosthetic structures, even if nothing is bothering you.
If the teacher is not perfect...
Of course, it is not always possible to perfectly prepare a tooth for a zirconium crown. Sometimes the specified 4 mm and 20º cannot be obtained. What to do in such cases? Dr. Christensen says that many dentists use composite cement in these cases, either self-adhesive (bonding included) or conventional (bonding applied separately). Materials offered by Gordon as an example are RelyX Unicem 2 (3M ESPE), Maxcem Elite (Kerr Dental), Multilink Automix (Ivoclar Vivadent), Panavia (Kuraray Dental).
At the same time, the loss of zirconium crowns fixed with such cements is a more frequent phenomenon than the loss of crowns with RMGI cements. To achieve a more reliable result when using composite cements, Dr. Christensen suggests applying the bonding agent to the prepared tooth and to the inner surface of the crown.
. The advice is based on CR's practical experience, but not on the recommendations of cement manufacturers: Gordon regrets the fact that there is simply no consensus among them on this issue.
Zirconium or cermet?
The restorative properties of zirconium dioxide and the uniqueness of the prosthesis manufacturing technique allow us to successfully solve the most complex aesthetic problems:
- structural stability
. It is stronger and stronger than metal, can withstand high loads, does not deform under pressure, and has low thermal conductivity, which makes it possible to manufacture large structures that do not change the configuration in a ceramic furnace, guaranteeing an exact fit throughout the entire life of the product; - biological compatibility
. The material is not prone to oxidation, it is safe for the opposite healthy units - metal ceramics can provoke allergies; - aesthetic profile
. Zirconium crowns provide excellent results while maintaining strength characteristics. The only controversial issue is the lack of strong fluorescence and insufficient transparency. This is a subjective opinion, since the required degree of transparency is selected depending on the volume of material, restoration area, type of restoration, and fluorescence can be recreated using special masses. The cement for fixation is selected according to the criteria of color, degree of brightness, and transparency - with its help, an experienced dentist can correct color inconsistencies in the finished all-ceramic restoration; - installation
. Preparation does not require grinding of significant amounts of tissue, removal of nerves, or long-term preparatory therapy. Each tooth is modeled individually and fits exactly into place.
Indications for installation
Zirconium crowns are indicated for many dental problems. Most often, such prosthetics are performed in the following cases:
- unsuccessful restoration when the structure should be replaced;
- damage to gum tissue due to caries;
- allergic reaction to components of other materials;
- aesthetic defects;
- blood flow problems;
- absence of lateral teeth and incisors;
Experts advise placing a crown made of dioxide for people with endocrine diseases and diabetes. They are also suitable for those patients who do not want to have their front teeth removed. After all, other crowns require the removal of nerves due to the likelihood of developing caries and other dental problems.
This solution will be ideal for those who need to replace more than four front or chewing teeth. Possible contraindications:
- too deep bite;
- involuntary grinding of teeth during sleep;
- teeth of low clinical height;
- inflammatory processes in the mouth;
- psychical deviations;
- low body resistance due to past illnesses;
- pregnancy.
Zirconium dioxide is a fairly strong material, and constant friction can lead to deformation of the corresponding tissues. For this reason, it is advisable not to install such crowns on people with increased tooth wear. It is important to see a doctor regularly to notice this process in a timely manner. If other solutions are not available for one reason or another, it is better to immediately install zirconium crowns on the antagonist teeth.