Available painkillers: esters and amides
Bibliography
1 GRLS, r/u LP-004175 dated 03/03/2017
2 Certificate GMP-0036-000221/18
3 Greveling K, Prens EP, Ten Bosch N, van Doorn MB. Comparison of lidocaine/tetracaine cream and lidocaine/prilocaine cream for local anesthesia during laser treatment of acne keloidalis nuchae and tattoo removal: results of two randomized controlled trials. Br J Dermatol. 2016 Jul 5. doi:10.1111/bjd.14848 Hernandez E.;
4 J. Cassuto, R. Sinclair, M. Bonderovic, Anti-inflammatory properties of local anesthetics and their present and potential clinical implications. Acta Anaesthesiol Scand 2006; 50; 265-282]
5 Based on IQVIA report March 2022 - September 2022
6 Russian medical journal. Zhigultsova T.I., Parkaeva L.V., Ilyina E.E., Vissarionov V.A.: “Experience of using 5% Emla cream in the practice of dermatocosmetologists”
7 Instructions for use of the medicinal product for medical use Acriol Pro
8 T.N. Calvey, N.E. Williams. Pharmacology for anesthesiologists. Publishing house Binom, Moscow, 2007, 119-128
9 Based on the report “Anesthetics in injection cosmetology for 2016” Vademecum Analytical Center for sales volume.
10 T.I. Zhigultsova, Ph.D. L.V. Parkaeva, E.E. Ilyina, professor V.A. Vissarionov: “Experience of using 5% Emla cream in the practice of dermatocosmetologists” Cosmetology and plastic surgery. Vol. 16, No. 9, 2008
11 On the Russian market there are so-called cosmetic products containing lidocaine and not registered as medicines
12 Cling film can be used as an occlusive dressing
13 Drug Release Studies on an Oil-Water Emulsion Based on a Eutectic Mixture of Lidocaine and Prilocaine as the Dispersed Phase
14 Federal Law-61 “On the Circulation of Medicines” dated April 12, 2010, Federal Law-323 “On the Fundamentals of Protecting the Health of Citizens in the Russian Federation” dated November 21, 2011 and Federal Law-532 “On Amendments to Certain Legislative Acts of the Russian Federation Regarding Counteraction to Trafficking falsified, counterfeit, substandard and unregistered medicines, medical devices and counterfeit dietary supplements" dated December 31, 2014.
15 Federal Law-532, Technical Regulations of the Customs Union on the safety of perfumery and cosmetic products, Federal Law 61, Federal Law 532, Criminal Code of the Russian Federation, Art. 235, 238, 227
16 V.V. Osipova.MMA named after. I.M. Sechenov. Psychological aspects of pain. Lecture. №1/2010
17 According to GMP News. Analysis of the market for local anesthetics used in cosmetic injections in 2022.
18 One type of occlusive dressing, namely: bandage, cling film, adhesive tape or rubberized fabric
19 The combination of lidocaine and prilocaine in concentrations above 0.5-2% has bactericidal and antiviral properties. In Akriol Pro the concentration is 5%.
20 A.A. Stepanov, G.V. Yatsyk, L.S. Namazova Method of preventing pain in young children during vaccination // Into the practice of pediatricians - 09.14.2006 -
21 N.V. Klipinina, RMJ, Some features of the perception and experience of pain by children: a psychologist’s view, reprint. 2007.1-7
22 E.A. Ranneva. The use of EMLA® cream in the complex correction of cosmetic imperfections. Experimental and clinical dermatocosmetology 2010, No. 2: 48-53.
23 Gonzalez S. Evaluation of Topical Anesthetics by Laser-Induced Sensation. Lasers in Surgery and Medicine 23:167–171(1998));
24 V.G. Lebedyuk et al. Anesthesia in dermatocosmetology. Experimental and clinical dermatocosmetology, 2010 No. 5
25 Meltem F. Söyleva Nilüfer Koçaka Bahar Kuvakia Seyhan B. Özkanb Erkin Ki˙rb; Anesthesia with Cream for Botulinum A Toxin Injection into Eyelids. Ophthalmologica 2002;216:355–358
26 E.V. Matuszewska and authors. Topical local anesthetics in cosmetology. Clinical Dermatology and Venereology. 03.2017 pp. 89-96
27 Therapeutics and Clinical Risk Management 2006:2(1) 99 – 113
28 F. Michael Ferrante, Timothy R. Wade Bopcore Postoperative Pain. Management. Per. from English/Ed. M.: Medicine, 1998.- 640 pp., p. 243
29 Lakhin R.E. Local anesthetics. Department of Anesthesiology and Reanimatology of the Military Medical Academy named after. S.M.Kirova, St. Petersburg, 2013, Committee on Ultrasound Technologies of the All-Russian public organization “Federation of Anesthesiologists and Resuscitators.” Clinical guidelines “Intensive therapy for systemic toxicity with local anesthetics. Moscow - St. Petersburg 2015 Page. 10 https://www.far.org.ru/recomendation
30 Wetter DA et al. J American Acad. Dermatol. 2010;63(5):789-98
31 https://www.1nep.ru/articles/issledovanie-sostava-populyarnykh-mestnykh-anestetikov/
32 ORDER OF THE MINISTRY OF HEALTH OF THE RUSSIA dated 08.10.2015 No. 707n
33 Davydov O.S. Peripheral and central mechanisms of the transition of acute pain to chronic pain and the possible role of cyclooxygenase 2 inhibition in the prevention of chronic pain syndrome. Neurology, neuropsychiatry, psychosomatics. 2016;8(2):10-16.
34 J. ALASTAIR CARRUTHERS, MD, JEAN DA CARRUTHERS, MD. Safety of Lidocaine 15% and Prilocaine 5% Topical Ointment Used as Local Anesthesia for Intense Pulsed Light Treatment. Dermatologic Surgery 2010;36:1130–1137
35 Ya-Xian et al. The number of cells in the stratum corneum of normal skin depending on the anatomical location on the body, age, gender and physical parameters Archives Dermatol Res 1999; 291:555–559.
36 J. Morgan, Magid S. Michael. Clinical anesthesiology, Book 1. Binomial. Moscow St. Petersburg, 2001
37 Arendt-Nielsen L, Bjerring P, Nielsen J. Acta Derm Venereol 1990;70:314-318
38 Belarusian State Medical University. 2nd Department of Therapeutic Dentistry. Therapeutic dentistry. Part 1. Ed. A.G. Tretyakovich, L.G. Borisenko.
39 Dermatol Surg 1999;25:950-954
40 K. Greveling et al. Br J Dermatol 176(1), 81-86. 2016 Dec 10
41 Juhlin and Evers Adv Dermatol 1990;5:75-92
42 Arendt-Nielsen L, Bjerring P, Nielsen J. Acta Derm Venereol 1990;70:314-318
43 Study Desensor 001. Wahlgren CF, Quiding H. J Am Acad Dermatol 2000;42:584-8.
44 https://www.1nep.ru/estetic/articles/13952/
45 Guide to dermatocosmetology, edited by E.R. Arabia and E.V. Sokolovsky. St. Petersburg: Foliant Publishing House LLC, 2008 - 632 pp.
46 https://www.1nep.ru/estetic/articles/132197/
47 https://medside.ru/dikain
48 https://medi.ru/instrukciya/novokain_9473/
49 https://medside.ru/anestezin
50 https://grls.rosminzdrav.ru/Default.aspx
51 Radman et al.2002, Yamashita., 2003
52 https://www.krasotaimedicina.ru/diseases/hematologic/methemoglobinemia
53 Evers H, Scott B, Dahlquist AC. Dermal analgesia after epicutaneous application of 5% cream, 5% prilocaine cream, 5% lidocaine cream and placebo cream, to volunteers. Study 89EM03 (n= 21, cross-over). CSR 802-10AC088-2,1989.
54 MASMI. A study of users of skin anesthetics. June 2018
55 O.M. Burylina, A.V. Karpova. Cosmetology. Clinical guidelines. GEOTAR-Media. Moscow, 2018
56 Postoperative pain: the role of peripheral and central sensitization mechanisms. https://rsra.rusanesth.com/publ/posleoperatcionnaya_bol.html
57 Paul M. Friedman, MD, Jushua P. Fogelman, MD and others. Comparative Study of the Efficacy of Four Topical Anesthetics. Dermatolog Surg 1999; 25:950-954
58 https://www.1nep.ru/articles/rynok-kosmeticheskikh-anestetikov-dlya-kozhi/
59 https://www.rlsnet.ru/mnn_index_id_879.htm
60 https://yandex.ru/health/pills/product/ultrakain-ds-2195
61 https://grls.rosminzdrav.ru/Default.aspx on 02/15/2021
62 Ziganshin O.R. Comparison of the effectiveness and safety of topical local anesthetics for superficial surgical interventions in dermatology. Clinical dermatology and venereology. 2018;17(6):53-60. https://doi.org/10.17116/klinderma 20181706153
63 Comparison of Topical Anesthetics for Radiofrequency Ablation of Achrocordons: Eutectic Mixture of Lignocaine/Prilocaine versus Lidocaine/Tetracaine Pratik Gahalaut,1 Nitin Mishra,1 Sandhya Chauhan,2 and Madhur Kant Rastogi11Department of Dermatology, Venereology and Leprosy, Shri Ram Murti Smarak Institute of Medical Sciences, Nainital Road, Bareilly 243001, India2Department of Pediatrics, Shri Ram Murti Smarak Institute of Medical Sciences, Nainital Road, Bareilly 243001, India
64 https://www.gazeta.ru/science/2012/11/01_kz_4837701.shtml
65 https://www.kp.md/daily/23716.3/53610/
66 https://doktorbel.livejournal.com/29873.html
67 https://politeka.net/zdorovye/870023-uchenye-vyjasnili-kak-muzhchiny-i-zhenshhiny-zapominajut-bol-kto-vynoslivee/
68 https://spacefacts.ru/news/people-and-medicine/psychology/792-udovolstvie-ili-bol.html
69 https://tattooinfo.ru/raznoe/foto-prokolotoj-guby-vidy-kak-delat-uxod-za-mestom-prokola.html
70 https://tatuazhpro.ru/pirsing/indastrial.html
71 https://sprs-therapy.ru/faq/V-kakih-sluchayah-nuzhno-primenyat-SPRS-terapiyu_i-v-kakih-nelzya
72 https://sprs-therapy.ru/faq/Kakim-obrazom-provoditsya-SPRS-terapiya
73 https://cosmetology-info.ru/6425/Metody-udaleniya-vtorogo-podborodka/
74 https://beauty.net.ru/public/inektsionnaya_konturnaya_plastika_nososleznoy_borozdy/
75 https://www.1nep.ru/articles/131016/
76 Morrison A.V., Bocharova Yu.M., Morrison V.V. Botulism toxin - a therapeutic effect in cosmetology (review). Saratov Scientific and Medical Journal 2016; 12(3):521–524.
77 A.V. Gara, V.G. Zolotareva, Features of botulinum therapy for aesthetic indications for patients over 45 years old, Injection methods in cosmetology No. 4-2011 – 54-60 s
78 Methodological manual on mesotherapy for students of postgraduate and additional professional education. / Shamov B.A., Dyadkin V.Yu., Zhelonkina T.I./ – Kazan: KSMU, 2011. – 60 p.
79 https://www.1nep.ru/estetic/articles/119953/
80 Evers H, Scott B, Dahlquist AC. Dermal analgesia after epicutaneous application of EMLA 5% cream, 5% prilocaine cream, 5% lidocaine cream and placebo cream, to volunteers. Study 89EM03 (n= 21, cross-over). CSR 802-10AC088-2,1989.
81 https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=019941
82 Superficial, medium or deep peeling: what to choose - https://medbooking.com/blog/post/
83 Features of medium peels – https://www.1nep.ru/estetic/articles/190169/
84 Facial peeling – https://cosmetology-info.ru/668/Piling-litsa/
85 Plastic surgery of cheekbones with fillers – https://cheap-fillers.ru/articles/plastika-skul-fillerami
86 Ozone therapy (O3) for the face - a revolutionary beauty technology - https://plastichno.com/cosmetology/ozonoterapiya-dlya-litsa#i-7
87 Effective face lift with liquid mesothreads: what is it and what are the popular brands? – https://beautyexpert.pro/kosmetologiya/inektsionnaya/tredlifting/vidy-nitej/zhidkie-mezoniti.html
88 Mesotherapy of the periorbital area using peptide cocktails – https://www.manuolog.ru/info/about/articles/stati-po-kosmetologii/mezoterapiya-periorbitalnoy-oblasti-s-primeneniem-peptidnykh-kokteyley/
89 Enzyme hair removal: getting rid of excess vegetation – https://plastikaplus.ru/kosmetologiya/epilyaciya/enzimnaya.html
90 Liquid mesothreads and traditional threadlifting: advantages and disadvantages – https://aesthetic-futures.com.ua/zhidkie-mezoniti-i-tradicionnyj-tredlifting-preimushhestva-i-nedostatki
91 Cannula in cosmetology and medicine – https://ladysdream.ru/kanyulya.html
92 7 myths about anesthesia: what are we afraid of? – https://www.psychologies.ru/articles/7-mifov-o-narkoze-chego-myi-boimsya/
93 Medium peeling - an uncompromising method of rejuvenation - https://plastichno.com/cosmetology/sredinnyj-piling#i-3
94 Khunger N. Standard guidelines of care for chemical peels. Indian J Dermatol Venereol Leprol 2008;74(Suppl):S5-S12 – https://pro.bhub.com.ua/cosmetology/himiceskie-pilingi-standartnye-rekomendacii-po-primeneniu#
95 Kim Lawless - 10 secrets of successful hair removal - https://www.cosmo.ru/beauty/body/10-sekretov-udachnoy-epilyacii/
96 All about Sugaring - https://www.gabbi-shugaring.ru/vse-o-shugaringe#rec61612476
97 Hirsutism – https://www.krasotaimedicina.ru/diseases/zabolevanija_endocrinology/hirsutism
98. Intralesional interferon therapy for recurrent warts, G. E. Bagramova, T.G. Sedova, A.N. Khlebnikova // Russian Journal of Skin and Venereal Diseases No. 1, 2013 – 23-26 p.
99. Korolkova T.N., Goma S.E. Study of the effect of mesotherapy with pineal gland peptides on skin moisture and elasticity, Russian Journal of Skin and Venereal Diseases. 2017; 20(5) – 305-310 p.
100. S.V. Klyuchareva, S.M. Nikonova, I.V. Ponomarev, Laser treatment of benign pigmented skin tumors, experimental and clinical dermatocosmetology No. 3, 2006 – 22-31 p.
101. Photorejuvenation in the complex correction of age-related skin changes, N.I. Tsisanova, Journal of Applied Aesthetics No. 1, 2007
102. https://plastichno.com/cosmetology/fotoomolozhenie
103. Current state of the problem of human papillomavirus infection / L. A. Yusupova, E. I. Yunusova, Z. Sh. Garayeva, G. I. Mavlyutova, K. A. Salakhutdinova // Attending physician No. 7/2019; Page numbers in the issue: 64-67 – https://www.lvrach.ru/2019/07/15437345
104. Human papillomavirus infection of the genitals in women, S.I. Rogovskaya, V.N. Prilepskaya, E.A. Mezhevitinova, M.N. Kostava // Bulletin of Dermatology and Venereology, N 6-1998, pp. 48-51. – https://nature.web.ru/db/msg.html?mid=1178539&uri=index.html
105. https://www.1nep.ru/estetic/articles/183501/
106. https://www.1nep.ru/articles/208888/
107. https://cosmetology-info.ru/6925/salon-procedures-Lipolitiki-dlya-litsa/
108. https://www.1nep.ru/articles/204894/
109. https://www.verywellhealth.com/stratum-corneum-anatomy-1069189
110. Turkin P.Yu., Rodionov S.V., Somov N.O., Mirgatia I.O. Venous trophic ulcers: current state of the issue // General Medicine. 2022. No. 1. URL: https://cyberleninka.ru/article/n/venoznye-troficheskie-yazvy-sovremennoe-sostoyanie-voprosa
111. Kruglova Larisa Sergeevna, Panina Anastasia Nikolaevna, Strelkovich Tatyana Igorevna Trophic ulcers of venous origin // Russian Journal of Skin and Venereal Diseases. 2014. No. 1. URL: https://cyberleninka.ru/article/n/troficheskie-yazvy-venoznogo-geneza
112. Yu.M. Stoiko, A.I. Kirienko, I.I. Zatevakhin, A.V. Pokrovsky, A.A. Karpenko et al., Russian clinical guidelines for the diagnosis and treatment of chronic venous diseases // Phlebology No. 3, 2022 – 143-240 pp. — https://webmed.irkutsk.ru/doc/pdf/ven2009.pdf
113. Dovnar R.I., Smotrin S.M. Trophic ulcers of the lower extremities: modern aspects of etiology and pathogenesis // Journal of GrSMU. 2009. No. 4 (28). URL: https://cyberleninka.ru/article/n/troficheskie-yazvy-nizhnih-konechnostey-sovremennye-aspekty-etiologii-i-pathogeneza
114. Burleva E.P., Babushkina Yu.V. Experience in outpatient treatment of trophic foot ulcers that complicated the course of diabetes mellitus // Hospital-replacing technologies: Outpatient surgery. 2022. No. 3-4. URL: https://cyberleninka.ru/article/n/opyt-ambulatornogo-lecheniya-troficheskih-yazv-stop-oslozhnivshih-techenie-saharnogo-diabeta
115. Kutsenko I.V., Andrashko Yu.V. Conservative treatment of trophic ulcers of the lower extremities in chronic venous insufficiency // Methodological recommendations. 2007. https://medinfo.center/wp-content/uploads/2019/12/metodichka-tya.pdf
116. Trophic ulcers of the lower extremities in outpatient clinic practice//Methodological recommendations for fourth-year students of the Faculty of Medicine. 2020 https://rsmu.ru/fileadmin/templates/DOC/Faculties/LF/fsurg2/algoritm_dignost/UP/3._UP_Troficheskie_rasstroi__stva_kozhi_nizhnikh_konechnostei__.pdf
117. Russian clinical guidelines for the diagnosis and treatment of chronic venous diseases. Phlebology, issue No. 2. 2013 https://www.mrckb.ru/files/flebologii.pdf
118. I. L. Mikitin, G. Z. Karapetyan, L. V. Kochetova, S. V. Yakimov, R. A. Pakhomova Modern view on the treatment of trophic ulcers // Creative surgery and oncology. 2013. No. 4. URL: https://cyberleninka.ru/article/n/sovremennyy-vzglyad-na-lechenie-troficheskih-yazv
119. Aralova M.V. Personalized technology for regional treatment of patients with trophic ulcers of the lower extremities. dis. for the academic degree of Doctor of Medical Sciences Voronezh, 2019
120. Lok et al. J Amer Acad Derm 1999;40:208-13. (Study EM9405)
121. Hansson C et al. Acta Derm Venereol (Stockh) 1993;73:231-233.
122. Order of the Ministry of Health of Russia dated October 13, 2017 No. 804n “On approval of the range of medical services.
123. Order of the Ministry of Health dated October 8, 2018 No. 707n “On approval of qualification requirements for medical and pharmaceutical workers with higher education in the field of training “Health and Medical Sciences”
124. 124. Starostina L.S. Helping control pain in children: advice from a pediatrician. Medical advice. 2021;(1):263–268. doi: 10.21518/2079-701X-2021-1-263-268
Intolerance to local anesthetics. Drug selection algorithm
The article discusses the problem of choosing a drug for local anesthesia from the point of view of preventing the development of adverse reactions associated with its clinical use, and provides the basic rules for selecting a drug in risk groups.
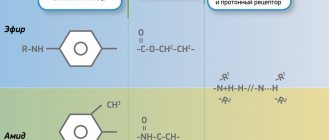
Table. Classification of local anesthetics
Introduction
Efficiency and safety are the main requirements for pharmacological drugs used for the treatment, prevention and diagnosis of diseases, as well as the main criteria for the successful use of drugs in clinical practice. Simultaneously with the increase in the number of drugs, the possibility of developing various undesirable reactions also increases. Adverse reactions that occur when using drugs occur in 1/10 of the world's population, but only 10% of them are caused by drug hypersensitivity [1]. These reactions may vary in clinical presentation, severity and have different outcomes.
As a rule, the pharmacological properties of therapeutic and diagnostic drugs are well known. However, a doctor cannot always predict hypersensitivity reactions [1].
An adverse reaction to a drug is an unexpected undesirable effect that occurs when using a drug in a therapeutic (preventive, diagnostic) dose.
Drug allergy is an increased sensitivity to a drug, which is based on immunological mechanisms.
Types of adverse reactions that occur when using drugs
There are two types of adverse reactions that occur when using pharmacological agents.
The first type of reactions are predictable side effects associated with the pharmacological action of drugs, depend on the dose used, can occur in any patient, and account for 75% of all adverse reactions to pharmacological agents. Pharmaceutical reference books and instructions for the use of drugs contain indications of the possibility of developing such reactions. The following are examples of predicted adverse reactions:
- toxicity of the drug;
- toxic reactions associated with overdose and/or accumulation of the drug;
- reactions caused by the pharmacological properties of drugs;
- reactions caused by the interaction of drugs;
- teratogenic effect of drugs;
- carcinogenic effect of drugs;
- mixed reactions [2].
Adverse reactions of the second type are unpredictable and are associated with reactivity and sometimes genetic characteristics of the patient. Let's name the options for unpredictable side reactions:
- Non-allergic congenital hypersensitivity (idiosyncrasy). Caused by enzyme deficiency.
- Drug hypersensitivity:
- allergic hypersensitivity (true allergic reactions: immunoglobulin E (IgE)-mediated and non-IgE-mediated). Immunological mechanisms are involved in these reactions;
- non-allergic hypersensitivity (pseudoallergy). It develops without the participation of immunological mechanisms [2].
Non-allergic congenital hypersensitivity (idiosyncrasy, fermentopathy) is a deficiency or incomplete activation of an enzyme involved in drug metabolism. Drugs or diagnostic agents can affect enzyme systems involved, for example, in the inactivation of serum kinins. If there is a deficiency of glucose-6-phosphate dehydrogenase, the use of oxidizing agents can lead to the development of hemolytic anemia in the patient. Sulfonamides, nitrofurans, and vitamin K preparations can also induce hemolysis in this group of patients.
Non-allergic hypersensitivity reactions, or pseudoallergic reactions, do not have immunological mechanisms, but can mimic the symptoms of an allergic reaction. The development of pseudoallergic reactions when using pharmacological agents may be associated with the direct or indirect release of histamine from mast cells and basophils, which occurs under the influence of the drug used. Some drugs are capable of non-immune activation of the complement system through the alternative pathway. As a result, activation intermediates with anaphylotoxin properties accumulate, which leads to increased membrane permeability, mast cell degranulation and histamine release. Pseudoallergic reactions may have other mechanisms. Non-steroidal anti-inflammatory drugs, salicylates, tartrazine can cause disruption of arachidonic acid metabolism. Accumulation of bradykinin may occur during treatment with angiotensin-converting enzyme inhibitors. When sulfites are used, sulfur oxide is formed, which has bronchoconstrictor properties [2].
Allergic reactions are distinguished by the participation of immunological mechanisms in their formation. Such reactions occur in a small number of patients, and their development is unpredictable. Being diagnosed with a drug allergy is a very serious decision. In case of erroneous denial of a drug allergy to a drug, its further use can lead to a tragic outcome. When drug allergies are overdiagnosed, the patient is deprived of the opportunity to use a whole group (sometimes several groups) of drugs that he sometimes needs [3, 4].
When using drugs, the development of psychophysiological adverse reactions is possible. They can occur in patients with hysterical neurosis, with autonomic disorders, as well as in patients who have suffered severe complications of drug therapy in the past.
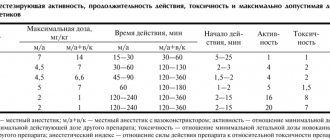
Classification of local anesthetics
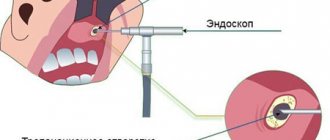
The emergence of a large number of modern, low-toxic local anesthetics (LA) has led to an expansion of their use in various fields of medicine and, unfortunately, to an increase in the number of patients who develop various adverse reactions when prescribed. Local anesthetics are drugs that reversibly inhibit the generation and conduction of impulses in peripheral nerves and nerve endings, which leads to loss of sensitivity in limited areas of the body [5, 6]. Types of local anesthesia vary depending on its clinical use in different areas of medicine:
- superficial anesthesia - application of MA to the skin, conjunctiva of the eye, mucous membrane of the nasal cavity, mouth, tracheobronchial tree, urinary tract, ear cavity;
- infiltration – dentistry, minor surgical interventions;
- conduction anesthesia - injection of a drug into the area of a nerve or plexus;
- epidural - injection of LA between the dura mater and the periosteum lining the inner surface of the spinal canal;
- spinal – injection of LA directly into the cerebrospinal fluid;
- intravenous regional anesthesia.
The use of this group of drugs is not limited to the field of medicine. In beauty salons, before painful procedures, MA is applied to the skin or injected. The patient may become sensitized to the drug and forget that he received procedures from a cosmetologist using MA. Most often, when interviewed, the patient does not mention such use of MA and almost never knows which drug was used. This is one of the reasons for various severity and sometimes fatal complications of various cosmetic procedures.
The chemical structure of LA determines their physicochemical characteristics and clinical properties. Local anesthetics consist of a hydrophobic (lipophilic) aromatic group, an intermediate ester or amide chain, and a hydrophilic secondary or tertiary amino group. Most MAs are tertiary ammonium bases, which are used in the form of solutions of water-soluble salts, mainly hydrochlorides. Basically, drugs differ in lipid solubility, binding to tissue proteins and dissociation constant [5, 6].
Depending on the intermediate chain, MAs are divided into esters and amides (table). The first group of local anesthetics (ester group) includes esters of benzoic acid (cocaine, Bencaine), esters of para-aminobenzoic acid (procaine, butamben), esters of aminobenzoic and benzoic acids (tetracaine). Ether MAs are relatively unstable in solutions and are quickly hydrolyzed in the body by pseudocholinesterase and some other esterases. One of the hydrolysis products is para-aminobenzoic acid, which can cause allergic reactions. The plasma half-life of these drugs is very short, so their tissue distribution is poorly understood.
The second group of MAs (group of amides) includes amides of heterocyclic and aromatic acids (Sovcaine, Novocaine), amides of aromatic amines - anilides (lidocaine, bupivacaine, mepivacaine, ropivacaine, etc.). Amide MAs are relatively stable in solution and are slowly hydrolyzed by liver microsomal enzymes. The rate of metabolism of different drugs is quite variable: prilocaine is the most rapidly metabolized drug, bupivacaine the slowest. In patients with impaired liver function, amide MAs may have a toxic effect due to prolongation of the drug's half-life; a decrease in hepatic blood flow leads to a slower inactivation of LA.
A small amount of drugs is excreted unchanged by the kidneys. A significant proportion of LA after administration enters the systemic circulation. The amount of absorbed drug and its peak plasma concentration depend on the dose and the presence of a vasoconstrictor in the solution (especially during conduction and infiltration anesthesia). The same dose of LA is associated with a different risk of toxic effects and depends on the anesthesia technique, the degree of tissue vascularization and interaction with tissue lipids. Anesthetics are actively absorbed through the mucous membranes. The binding of MA to plasma proteins affects pharmacokinetics and pharmacodynamics. Anesthetics of the ester group bind to plasma proteins slightly (
Cross-reactions of local anesthetics
Many drugs have similar chemical structures and have cross-allergenic properties. Among ether group MAs, cross-allergic reactions are quite common. A patient who is allergic to Novocaine should not use Anestezin, Dicaine. Cross-allergic reactions between drugs from the amide and anilide groups are quite rare. Research results (application tests) indicate the possibility of developing cross-allergic reactions between lidocaine, prilocaine, and mepivacaine. There are no cross-allergic reactions between drugs of the first (ether) and second (amide) groups. According to numerous data, the use of MAs from the group of amides and anilides leads to the development of adverse reactions, both allergic and non-allergic, much less often.
MAs of the ester group, being derivatives of benzoic, aminobenzoic and para-aminobenzoic acids, have common antigenic properties with drugs having a para-amino group and a benzenesulfonamide group [2, 4]. The para-amino group contains Novocaine and other benzoic acid esters; Menovazin, Anestezol, Almagel A and other combination drugs; Novocainamide; sulfonamides; para-aminobenzoic acid and its derivatives; para-aminosalicylic acid and its derivatives; ethacridine lactate. Sulfonamides have a benzenesulfonamide group; sulpiride; sulfonylurea derivatives (glycemic agents, sulfourea); diuretics containing a sulfamide group linked to a benzene ring; thiazide diuretics; carbonic anhydrase inhibitor; sotalol; para-aminobenzoic acid derivatives; para-aminosalicylic acid. If you are allergic to drugs of these groups, you cannot use MA of the ester group.
The patient may become sensitized when using medications that contain LA. Thus, benzocaine (Anestezin) is included in the preparations Almagel A, Anbital, Bellastesin, Pavestezin, Menovasin, and Anestezol suppositories. Lidocaine is contained in the preparations Aurobin, Lidactone, Strepsils Plus, Procto-Glivenol suppositories, Lidochlor (gel for topical use, contains lidocaine hydrochloride and chlorhexidine gluconate).
Procaine (Novocaine) is included in Solutan, Hemoroid ointments and suppositories, Sulfocamphocaine (a complex compound of sulfocamphoric acid and Novocaine). Trimecaine is contained in ointments Dioksikol, Dioksizol, Levosin.
In practice, cross-reactivity of pharmacological agents is not always taken into account. We must not forget that complex preparations may contain a substance to which the patient is sensitized.
Side effects of local anesthetics
Local anesthetics can cause toxic, allergic and pseudoallergic reactions. Most of the side effects that occur when using MA are associated with vegetative-vascular disorders, fear of surgery or dental procedures, toxic, hysterical reactions. Sometimes vasoconstrictors included in some local anesthetics have side effects. True allergic reactions to LA occur rarely [7, 8].
Toxic reactions
Local anesthetics and their metabolites are weak bases and easily cross the blood-brain barrier. The toxic effect is manifested by effects on the central nervous system (CNS), peripheral nervous system, cardiovascular system, and blood [5, 6, 7]. These reactions most often occur with an absolute overdose, when the dose of the drug is exceeded, or with a relative overdose associated with impaired drug metabolism. MAs have a “narrow therapeutic corridor,” that is, the interval between the maximum therapeutic and minimum toxic dose is small. Toxic reactions can also develop in diseases of the liver and kidneys.
The intensity of toxic reactions is divided according to severity [6]. Mild toxic reactions are manifested by depression of the central nervous system, lethargy, dizziness, drowsiness, nausea, tachycardia, and fluctuations in blood pressure. Severe toxic reactions are manifested by increased reflex excitability, motor restlessness, vomiting, the appearance of nystagmus, tremors, visual and auditory disturbances, severe arterial hypotension, bradycardia, and bradyarrhythmia. In severe toxic reactions, heart rhythm disturbances, angina attacks, tonic, clonic convulsions, paralysis of the respiratory and vasomotor centers, and cardiac arrest are possible.
MAs suppress cortical inhibitory pathways, resulting in uncontrolled activity of the excitatory component. The stage of unbalanced excitation with a further increase in the level of the drug can turn into generalized inhibition of the central nervous system. When applied in too large doses, LA can have a toxic effect on nerve tissue. The effect of MA on the cardiovascular system is associated with both a direct effect on the myocardium and an indirect effect on autonomic nerve endings. Typically, cardiovascular complications develop after the onset of neurological symptoms. All MAs, except cocaine, reduce the force of heart contractions and cause vasodilation, which leads to arterial hypotension. Collapse often develops when high doses of anesthetic are used, but sometimes when relatively small doses of drugs for infiltration anesthesia are used.
It is known that the administration of large doses of prilocaine can lead to the accumulation of a metabolite that is capable of converting hemoglobin into methemoglobin. High levels of methemoglobin are tolerable for healthy people, but can cause decompensation in patients with heart and lung diseases [7, 8, 9].
Non-allergic hypersensitivity (enzymopathy)
A lack of enzymes involved in the metabolism of drugs, or their incomplete activation, can lead to the development of adverse reactions. Insufficient pseudocholinesterase activity may impair the metabolism of essential MAs.
Allergic reactions
True allergic reactions to MA, in the formation of which immunological mechanisms take part, develop quite rarely and account for about 1% of all adverse reactions to this group of drugs. Immediate reactions, IgE-mediated, can manifest as urticaria, angioedema, symptoms of allergic rhinitis, conjunctivitis, anaphylaxis reactions, the severe degree of which is anaphylactic shock. Contact reactions at the site of LA application (swelling, hyperemia) are more common. There are known cases of delayed reactions that can occur several hours after administration of the drug and manifest themselves in the form of various exanthems, erythroderma, erythema nodosum, and in rare cases, allergic vasculitis [10, 11, 12].
Pseudoallergic reactions
Non-allergic hypersensitivity reactions are characterized by the fact that they are mediated by the same mediators as true allergies; clinical manifestations imitate allergies, but immunological mechanisms are not involved in their formation. The mechanism of such reactions may be associated with direct nonspecific release of histamine from basophils and mast cells or activation of the complement system through an alternative pathway. Clinically, pseudoallergic reactions can manifest themselves as various exanthemas, anaphylactoid shock, skin hyperemia, generalized itching, acute rhinitis, bronchospasm, and dysfunction of the gastrointestinal tract. The severity of such reactions depends on the rate of LA administration, its concentration, route of administration, as well as the content of mast cells at the site of drug administration. The development of true allergic reactions does not depend on these factors.
Groups at risk of adverse reactions to local anesthetics
There are groups of people whose risk of adverse reactions is increased. This applies to any adverse reactions to MA [12, 13]. The risk group for the development of adverse reactions to the use of MA includes:
- persons who have previously suffered reactions to MA;
- patients with an allergic disease (the presence of an allergic disease in a patient is a risk factor for the development of anaphylaxis);
- patients with coronary heart disease (CHD), unstable angina, receiving beta-blocker therapy;
- patients with intended administration of a large volume of LA;
- patients in whom MA is used frequently, at short intervals, which happens during oral sanitation, prosthetics, etc.;
- pregnant and lactating women;
- patients with a pronounced fear reaction before the procedure;
- elderly patients.
In elderly patients, the development of adverse reactions may be associated with a decrease in body size, water volume, and muscle mass. In such patients, the volume of distribution of drugs decreases. With age, the glomerular filtration rate and renal tubular function decrease (by approximately 30% by age 65%), blood flow in vital organs slows down, the binding capacity of blood plasma decreases, and the metabolizing function of the liver suffers. Concomitant diseases can lead to impaired metabolism and excretion of drugs. Hypoalbuminemia leads to a decrease in the binding of drugs to proteins and an increase in the free active fraction of the drug [14].
The role of vasoconstrictors, preservatives and stabilizers in the development of adverse reactions when using local anesthetics
Many LA cause vasodilation and are therefore rapidly absorbed from the injection site. To increase the potency and duration of action, vasoconstrictors are often added to MA, which reduce the systemic toxicity of anesthetics and increase their therapeutic index by slowing absorption. To block the conduction of impulses along nerve fibers, only one MA is sufficient, but to prolong its action and enhance the effect, vasoconstrictors such as Adrenaline (epinephrine), Noradrenaline (norepinephrine), Mesaton (phenylephrine), Octapressin (felypressin) are used. A vasoconstrictor is necessary to contract blood vessels, slow down the absorption of local anesthetic, and create a high concentration of the latter at the injection site. This enhances the effect of anesthesia and reduces toxic effects [5, 6, 7].
Adrenaline is the most powerful vasoconstrictor. It can have an undesirable effect on the adrenergic receptors of the heart (tachycardia), blood vessels (severe vasoconstriction), liver, cause an increase in blood sugar levels, and promote contraction of the uterine muscles. A possible increase in intraocular pressure in narrow-angle glaucoma and cardiac decompensation in patients with cardiovascular diseases can be dangerous. Some MA solutions used in dental practice contain the vasoconstrictor felypressin. This non-catecholamine vasoconstrictor in its chemical structure resembles vasopressin, a hormone of the posterior pituitary gland. Felypressin affects only peripheral blood vessels and has no effect on the heart. It can be used in patients with coronary artery disease and other diseases in which the use of catecholamine is contraindicated.
There are forms of local anesthetics that do not contain vasoconstrictors. Information about the content of the vasoconstrictor and its concentration is important when choosing a drug for anesthesia in risk groups.
Those at risk for developing adverse reactions to a vasoconstrictor include:
- patients with cardiovascular diseases (hypertension, coronary heart disease, heart failure);
- pregnant women (risk of uterine muscle spasms);
- elderly patients (comorbidities and basic therapy for many of them);
- patients receiving treatment with glucocorticosteroids (high doses, long-term use of which can affect the condition of the adrenal glands), tricyclic antidepressants, monoamine oxidase inhibitors, drugs with alpha-adrenergic blocking activity, rauwolfia drugs, thyroid-stimulating hormones (these individuals may have a high sensitivity to adrenaline) [15] .
The preservative (parahydroxybenzoate), which is part of MA, serves to increase the shelf life of drugs. The presence of this component in the drug also requires an analysis of its tolerability [6, 12, 13]. Parahydroxybenzoates are included in various cosmetics, creams, toothpastes and can cause contact allergic reactions. A related chemical compound - para-aminobenzoic acid - is a metabolite of Novocaine, that is, people who are allergic to essential MAs are likely to develop an allergic reaction to preservatives - parahydroxybenzoic acid esters. There is a danger of developing allergic reactions to preservatives in persons allergic to drugs containing a para-amino group and a benzenesulfonamide group.
Stabilizers (sodium or potassium disulfite) are added to solutions containing epinephrine to prevent oxidation and increase the stability of the vasoconstrictor [5, 7, 13]. They can cause undesirable reactions with hypersensitivity to sulfites and the development of bronchospasm in patients with bronchial asthma.
Thus, to make a decision on the use of a specific local anesthetic, information about the drug itself, the somatic status of the patient and all the drugs he uses, including topical ones, is necessary.
Principles for selecting a local anesthetic in risk groups
In patients with coronary artery disease, the use of catecholamines can increase myocardial hypoxia, therefore, MA is used without vasoconstrictors or in a minimal dose of the latter, the drug is administered slowly.
In patients with diabetes mellitus, MA without catecholamines is used or felypressin is used as a vasoconstrictor.
For kidney diseases, the least toxic MAs with rapid metabolism are recommended.
In case of liver diseases with impaired liver function, MAs that are metabolized in the liver should not be prescribed, since the toxicity of MAs increases due to decreased blood flow and hypoproteinemia. For such patients, ether anesthetics, which are not metabolized by the liver, are preferable.
For pregnant and lactating women, the least toxic MAs, short-acting, are used.
For glaucoma, MA without vasoconstrictors is used; Felypressin can be used as a vasoconstrictor.
In elderly patients, drugs without catecholamines or with minimal concentrations of catecholamines are used for local anesthesia [12, 13, 15].
Patients with allergic diseases are a special group of people. To decide on the use of MA in these patients, a detailed allergic and pharmacological history is especially important. Information about concomitant diseases and their basic therapy is required. The tolerability of both the MA itself and the vasoconstrictor, preservative and stabilizer contained in the solution should be taken into account. In patients with sulfonamide intolerance, ethereal MAs should not be used. For patients with bronchial asthma, it is dangerous to use MA containing stabilizers (sodium and potassium disulfites) due to the risk of developing bronchospasm. Information about previous reactions to drugs of other groups will help to avoid the development of cross allergic reactions. It is preferable (taking into account the medical history) to prescribe MAs of the amide group without stabilizers and preservatives. It is especially dangerous for such patients to exceed the dose! The patient must have a “Passport of a patient with an allergic disease”.
Prevention of adverse reactions to local anesthetics
1. It is necessary to compare the risk of possible complications with the negative consequences of refusing to use MA.
2. The tolerability of local anesthesia should be clarified if it has been performed previously.
3. If an allergic reaction to MA has been observed in the past, a drug belonging to a different group should be used. Thus, if the “suspected” drug is an ester derivative, drugs of the amide group can be used. In case of a reaction to MA containing an amide group, it is possible to use another amide compound (the possibility of cross-reactions between lidocaine, prilocaine and mepivacaine is assumed) [13].
4. In case of severe previous reactions (both allergic and non-allergic), it is necessary to stop using MA.
5. It is necessary to determine the degree of risk not only of the surgical intervention itself, but also of the use of local anesthesia.
6. Do not use drugs whose tolerability is questionable.
7. Premedication according to indications.
Premedication
Before surgery, in patients with allergic diseases in the acute phase, antihistamines (chloropyramine or clemastine) and glucocorticosteroids (prednisolone, dexamethasone) are administered parenterally. The dose of drugs and the frequency of their administration depend on the patient’s condition, concomitant diseases and the basic therapy used by the patient [4].
Persons with pronounced fear reactions (these persons are at risk) are recommended to take sedatives before manipulation [13].
When is it necessary to perform diagnostic tests with local anesthetics?
It is not always possible to find out which particular MA previously caused the reaction. In some cases, it is not possible to determine the nature of the reaction (allergic, pseudoallergic, toxic) only on the basis of anamnesis. Unfortunately, there are still no laboratory tests whose results can be trusted 100%. In some cases, specific IgE antibodies to certain MAs are determined. But these tests are informative only for immediate allergic reactions, IgE-mediated. The presence of specific Igs belonging to other classes weakly correlates with clinical manifestations and is not considered a reliable sign of allergy. The State Scientific Center “Institute of Immunology of the Federal Medical and Biological Agency of Russia” has developed and successfully used a test for inhibition of natural leukocyte emigration in vivo according to A.D. Ado, including with MA. Laboratory tests that are widely used today give a high percentage of false positive results. Some techniques are labor-intensive, expensive, and require a well-equipped immunological laboratory, which makes them difficult to use for routine examination. There are no reliable tests that could identify the possibility of developing a pseudo-allergic reaction. In rare cases, it is necessary to select a specific drug, namely if:
- Previously, when using MA, the patient experienced any side effects, the mechanism of which is not clear;
- there are no medical documents describing the clinical symptoms of reactions that occurred previously;
- the measures that were taken to stop the reaction that occurred are not known;
- There is no information about the drugs used for anesthesia and whether the patient received any concomitant therapy for the treatment of other diseases during this period of time [3].
And a few more rules that need to be followed when selecting a drug for local anesthesia.
- Skin and provocative tests with MA are carried out only according to strict indications, but are not used to satisfy the curiosity of the doctor or patient!
- No tests are performed on a drug that has previously caused reactions. For samples, MAs of another group are selected.
- Diagnostic tests are performed only by an allergist. The selection of the drug is carried out immediately before using MA. The examination is carried out in the treatment room. Must have an anti-shock kit!
- Before the drug selection procedure, the patient signs an informed consent.
- The patient should not use antihistamines at the time of examination (discontinue the drug 5–7 days before).
- A necessary condition is that MA should not contain a vasoconstrictor, preservative or stabilizer.
- The LA should not be cross-reactive with the drug that previously caused the reaction.
After maintaining 15-minute intervals, a prick test or a prick test with undiluted MA is performed (assessment of the reaction to test control and histamine is required). If a negative reaction is obtained, then 0.1 ml of the drug, diluted 1:100, is administered subcutaneously; if there is no reaction, the next dose of MA is 0.1 ml, diluted 1:10. Then 0.1 ml of undiluted drug is administered, and if there is no reaction, the patient receives a dose of 1.0 ml and 2.0 ml at fifteen-minute intervals [3].
The test results are assessed immediately; in the conclusion, it is clarified that currently no allergy to this drug has been identified; the total dose of LA administered to the patient is always indicated. The patient must remain under medical supervision for an hour [3].
There should not be a long time interval after selecting the drug until it is used. Knowing the peculiarities of the formation of drug allergies, one cannot exclude the possibility of sensitization over a long period of time.
Is there polyvalent intolerance to MA? It happens, but extremely rarely and most often of non-allergic origin. For such patients, they try not to use local anesthesia, and if necessary, general anesthesia is performed.
Conclusion
Thus, before performing a surgical or other intervention using a local anesthetic, the doctor must not only assess the scope of the operation and its risk for the patient, but also answer the questions:
1. Which MA can be used in this patient? It is necessary to take into account toxicity, duration of action, and the chemical group to which the drug belongs.
2. Is it possible to use MA with a vasoconstrictor? If possible, then with what vasoconstrictor (catecholamine or felypressin) and in what dose?
3. Does this MA contain preservatives and stabilizers and can they be used in this patient?
4. Does this patient need to consult an allergist? If consultation is necessary, what questions should he be asked?
5. Does the patient need premedication? What medications are needed and in what dose?
Very often, a careful analysis of the answers to the questions listed above helps to avoid complications.