Comparative characteristics of the use of local anesthetics in dentistry
Anesthesia is one of the pressing problems of dentistry. The most common and safe way to relieve pain is local anesthesia, the effectiveness of which largely depends on the type and method of use of the anesthetic. The problem of pain and anesthesia attracts the attention of doctors of all specialties, since after the first duty - saving a person’s life - the most important task was and remains to relieve him of pain.
For some people, fear of the upcoming treatment contributes to their refusal to avoid visiting the dental office under any pretext.
Which is subsequently fraught with complications without timely treatment of dental caries. This includes the occurrence of complicated forms of caries with the formation of chronic foci of odontogenic infection, which contribute to the development or aggravate the course of a number of foci of conditioned diseases and pathological conditions (rheumatism, nephritis, iridocyclitis, etc.), and the occurrence of acute purulent-inflammatory processes - periostitis, osteomyelitis , phlegmon and abscesses, which are sometimes life-threatening. Therefore, pain management is one of the most pressing problems of modern dentistry. Ensuring complete painlessness is very important in the daily practice of a dentist. Imperfect treatment methods, shortage of anesthetics, lack of motivation, and often incompetence of dentists contribute to the deterioration of the quality of qualified dental care provided to the population.
The purpose of this work is to identify the effectiveness of various anesthetics during surgical interventions against the background of acute and chronic inflammatory processes.
Mechanism of action
Penetrating through the nerve fiber membrane, anesthetics bind to the receptor in the area of sodium channels on the inner surface of the membrane. Blocking the membrane's sodium channels then prevents the generation of an action potential. Accordingly, the conduction of afferent impulses from receptors in the central nervous system and impulses along the autonomic nerves, and in high concentrations along the motor nerves, is also blocked. But the transmission of nerve impulses is temporarily blocked. When the action of local anesthetics wears off, the function of sensory nerve endings and conductors is completely restored. Local anesthetics act on any part of the nervous system and on any fibers: small fibers are more sensitive to the action of anesthetics than large ones. In this case, unmyelinated fibers are more easily blocked than myelinated ones. First of all, local anesthetics relieve pain, then taste, temperature and tactile sensitivity. Complete anesthesia, i.e. anesthesia is achieved by blocking the conduction of excitation along all groups of sensory fibers. After absorption of local anesthetics into the blood, systemic and toxic effects may develop. The central nervous system and cardiovascular system are most sensitive to the action of local anesthetics[1].
Comparative characteristics of local anesthetics
| Lidocaine | Mepivacaine | Artikain | |
| Plasma protein binding | 50% | 78% | 95% |
| Half-life in minutes | 96 | 114 | 29 |
| Anesthetic activity | 4 | 4 | 5 |
| Toxicity | 2 | 1,7 | 1,5 |
| Duration of anesthesia (in min) without vasoconstrictor | 30-60 | 45-90 | 60 |
| Duration of anesthesia (in minutes) with a vasoconstrictor | 120-130 | 120-130 | 180 |
| Maximum permissible dose (mg/kg) with vasoconstrictor | 7 | 6,6 | 7 |
| Maximum permissible dose (mg/kg) without vasoconstrictor | 4,5 | 4,5 | 5 |
| Speed of action | Fast | Fast | Very fast |
RATIONALE FOR THE CHOICE OF DRUGS FOR LOCAL ANESTHETICS
The effectiveness profile of local anesthetics is characterized by the following parameters:
– onset of anesthesia, which is defined as the time between injection and complete anesthesia;
– successful anesthesia, which is defined as the percentage of achieving complete anesthesia (electroodontodiagnosis, the patient’s reaction to the manipulation);
– effective dose - the dose that provides complete anesthesia;
– duration of anesthesia, which is defined as the duration of complete anesthesia;
– spread of anesthesia, which is defined as penetration into soft tissues and adjacent teeth (S. Malamed, 1990) [7].
Conclusion.
1. Ultracaine can be used in patients with hyperalgesia during traumatic interventions and if it is necessary to create severe ischemia to reduce bleeding during the intervention, regardless of the phase of inflammation.
2. Lidocaine is more rationally used during operations on soft tissues, periodontal disease, and removal of mobile teeth.
3. In patients with chronic inflammatory processes, local anesthesia with anesthetics with and without a vasoconstrictor did not make any significant difference.
4. In case of acute inflammation, it is more rational to use 4% ultracaine solution with a vasoconstrictor, due to the most effective anesthesia both in terms of duration and intensity.
The demographic situation in the world entails the emergence of a complex of economic and social problems caused by the changing role of older people in society. The creation of new means and techniques that help increase the duration of a person’s active life while maintaining basic physiological functions is one of the pressing problems of aesthetic medicine [1]. Cosmetology primarily involves preserving and improving appearance, preventing aging of the face and body, and rejuvenating programs without surgical intervention. The emergence of high-tech methods that make it possible to correct involutional changes in the skin, and the tendency to move from the use of non-invasive manipulations to more invasive techniques have made it possible for cosmetologists to successfully carry out anti-aging procedures, less often resorting to plastic surgery [2]. Most invasive procedures performed require preliminary anesthesia. Therefore, an urgent problem is the choice of anesthesia method for cosmetic interventions.
As a rule, local anesthesia is used in cosmetology, which includes application (superficial, topical, terminal), infiltration and regional [3]. Superficial anesthesia occurs when the local anesthetic comes into direct contact with tissue. With infiltration anesthesia, a local anesthetic is injected into the surgical area intradermally with a thin needle, which blocks the conduction of nerve impulses in the deeper layers of tissue. Regional anesthesia is based on the administration of a local anesthetic in close proximity to the nerve trunk innervating a specific area, and can be conductive, spinal, epidural or intravascular. More often, cosmetologists use superficial and infiltration anesthesia. The use of injection methods of anesthesia is not always justified, especially when there is a large number of elements to be removed, a large area of the treated surface, etc. Injection of anesthetics leads to rapid swelling and compression of blood vessels, which modifies the clinical picture, disrupting the visualization of blood vessels. These features make it difficult to perform injection contouring, laser and photocoagulation of benign vascular neoplasms and other cosmetic procedures. Also, injection methods are unsafe from the point of view of toxic effects. Severe and sometimes fatal toxic effects on the central nervous (CNS) and cardiovascular systems can occur with significant overdose of anesthetics. This occurs when large doses of anesthetics are inadvertently released into the systemic circulation [4]. Therefore, the safest method in the practice of a cosmetologist is the application method. This method best meets the requirements of a cosmetologist for anesthesia, since it has a minimal traumatic index, causes a small number of visible side effects, and provides the opportunity to carry out a one-step complex correction in a short time.
In cosmetology, any manipulation associated with violating the integrity of the skin barrier is performed with anesthesia to reduce the pain of the procedure. Invasive procedures include laser and radio wave destruction, electrocoagulation of benign neoplasms, mesotherapy, injection contouring, administration of botulinum toxin A, hair removal, especially in areas with thin sensitive skin (bio- and electrolysis, laser and photoepilation), derma-abrasion, skin graft transplantation , puncture biopsy.
Structure and properties of local anesthetics
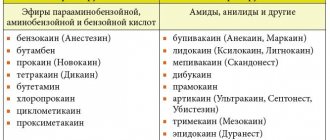
All local anesthetics have a similar chemical structure. They consist of a hydrophobic (lipophilic) aromatic group, a hydrophilic (secondary or tertiary) amino group, and an intermediate ester or amide chain. Depending on the type of intermediate chain, local anesthetics are divided into esters and amides (Fig. 1).
Rice. 1. The structure of local anesthetics.
Local anesthetics of the ester group include novocaine (procaine), benzocaine (anesthesin), tetracaine (amethocaine), etc. Amide anesthetics include lidocaine (xylocaine), prilocaine, mepivacaine, bupivacaine, ropivacaine, etc. Between these two groups There are important differences between local anesthetics. Esters are relatively unstable in solutions and are quickly hydrolyzed in the body by cholinesterase and some other esterases. One of the hydrolysis products is para-aminobenzoic acid, which is a common cause of allergic reactions. In contrast, amides are relatively stable in solution and are slowly broken down by liver amidases. In addition, hypersensitivity reactions to anesthetics of the amide group develop extremely rarely [4].
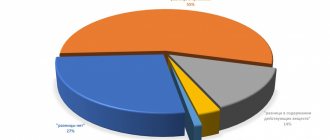
The chemical structure of local anesthetics determines their physicochemical characteristics and clinical properties (Fig. 2, 3).
Rice. 2. Properties of local anesthetics [4].
Rice. 3. Physico-chemical and pharmacological effects of local anesthetics [4].
When working with anesthetics, it is important for cosmetologists to know how quickly a particular drug will act, what the strength of anesthesia will be, how long the effect will last and what risks the presence of a particular component in the composition carries. There is a correlation between the lipid solubility of an anesthetic and its potency, which reflects the ability to penetrate the perineurium and neuronal cell membranes to reach the point of action in the axoplasm.
Binding to tissue proteins affects the duration of action of local anesthetics. For example, procaine binds weakly to proteins and its effect is short-lived. Lidocaine and prilocaine are moderately protein bound and have an average duration of action [4].
The dissociation constant (pKa) is the most important factor affecting the rate of onset of the effect. Low pKa values indicate rapid development of the reaction. For example, a reaction to lidocaine will develop faster than to tetracaine. The closer the pKa is to the physiological pH, the higher the concentration of the non-ionized fraction that penetrates the neuron membrane, the faster the local anesthetic begins to act. Having entered the cell, some of the molecules are ionized until a new equilibrium state is reached between the ionized and non-ionized fractions. Only ionized cation molecules interact with receptors in sodium channels. The degree of ionization of the anesthetic is of great clinical importance. For example, when it enters tissue with a low pH (for example, an inflammatory process at the injection site), the concentration of the ionized fraction of the anesthetic increases, and it takes more time for the effect to develop. However, other factors, such as the dose and final concentration of anesthetic in tissues, can also influence the rate of blockade development [4].
Effects on different sensory modalities
Local anesthetics reversibly block the conduction of nerve impulses in peripheral nerves and nerve endings. After the administration of the anesthetic, pain sensitivity first disappears, then temperature, tactile and proprioceptive [4]. Anesthetics used for topical anesthesia often do not lead to loss of tactile sensitivity, which does not indicate their ability to block pain sensitivity.
Systemic action of local anesthetics and influence on the inflammatory response
Since sodium channel blockade affects the propagation of action potentials throughout the body, it is not surprising that local anesthetics can produce systemic toxic effects. In addition to the side effects that are characteristic of all local anesthetics, there are also individual ones that are characteristic only of certain drugs.
Local anesthetics are characterized by a two-phase effect on the central nervous system. If they are not introduced too quickly, early symptoms appear first, then later, more severe ones. Low doses of lidocaine (2-4 mg/kg) have an anticonvulsant effect and are used to treat status epilepticus, but after administration of large doses, CNS excitation develops. As the concentration of local anesthetic in the plasma increases, numbness of the tongue and mouth, dizziness, blurred vision, slurred speech, muscle twitching and tremors, restlessness and confusion of speech are observed. If the concentration of local anesthetic in plasma exceeds a critical level (for lidocaine - 9 mcg/ml), a grand mal seizure may develop.
The dual effect of local anesthetics occurs when affecting the cardiovascular system. Low doses of lidocaine can eliminate some types of ventricular arrhythmias. An overdose of local anesthetics can cause profound arterial hypotension, bradycardia, bradyarrhythmia, and even cardiac arrest. Typically, cardiovascular complications develop after the onset of neurological syndromes (Fig. 4).
Rice. 4. Systemic effect of local anesthetics [4].
Allergic reactions to modern local anesthetics are very rare. Most often, skin reactions are observed with repeated use of ester group anesthetics; anaphylactic reactions occur much less frequently. The role of a hapten is a metabolite - para-aminobenzoic acid, which induces an immunological reaction. The existence of cross-sensitization between ether and amide anesthetics has not been proven. Rare allergic reactions to amide anesthetics in the vast majority of cases are caused by methylarabene, added as a stabilizer to multi-dose vials, or by the presence of preservatives in TMA [4].
The pain that a person experiences due to tissue damage is a consequence of the activation of peripheral and central sensitization mechanisms. These events cause inflammation and are accompanied by the release of a wide range of tissue plasma and neurogenic mediators and algogens in the area of damage. Local anesthetics, by blocking the mechanisms of peripheral sensitization, can significantly reduce catabolic reactions in the post-procedure period, prevent or reduce the development of swelling, redness, and inflammation.
The results of the studies showed the inhibitory activity of local anesthetics in therapeutic concentrations (lidocaine 0.25-4%, tetracaine 0.25-4%) against a number of pathogenic bacteria, herpes viruses and fungi. Thus, local anesthetics have a complex local anti-inflammatory effect, and their use can shorten the patient’s recovery period [5].
History of the use of topical local anesthetics for anesthesia of the skin
The history of the use of topical anesthetics for the skin and mucous membranes goes back more than 130 years. The first local anesthetic, described by A. Niemann (1860) and put into practice by doctors Koller and Anrep in the 70-80s of the last century, was cocaine. Despite its widespread use, this anesthetic had a number of serious disadvantages, such as short duration of action, addiction, and most importantly, high toxicity, which led to many cases of severe and even fatal poisoning.
Methods with low concentrations and the introduction of adrenaline (1892), which ensured slower absorption due to its vasoconstrictor effect, made it possible to somewhat reduce the toxicity of cocaine-based anesthetics.
The discovery of novocaine in 1904 by the German chemist A. Eichhorn ushered in a new era in regional anesthesia. Applications of novocaine solution had a weak analgesic effect for manipulations on the skin.
In 1943, the Swedish scientist N. Lofgren managed to introduce a new class of local anesthetic substances by synthesizing lidocaine. The drug became the “anesthetic of choice”, replacing novocaine as the “gold standard”.
In 1957, S. Monash, and in 1971, J. Adriani, N. Dalili, in search of an ideal drug for local anesthesia of the skin, showed that some local anesthetics, although they had an anesthetic effect on the skin, but none of the proposed drugs was not sufficiently clinically effective. After 10 years, it was proposed to use 5 or 10% amethocaine (tetracaine), dissolved in dimethyl-sulphoxide (DMSO, dimethyl-sulphoxide), which ensures the penetration of the local anesthetic through intact skin. However, the drug was not widely used in clinical practice, since DMSO caused various pathological skin reactions associated with the release of histamine. In the 60s of the 20th century, 30% lidocaine was used for local anesthesia of the skin, but the use of such a high concentration of local anesthetic caused toxic complications without providing sufficient anesthesia.
In the late 70s (L. Оhlsen) [6], ketocaine (a local anesthetic with high lipophilicity) was developed, which was effective for anesthesia of the skin, but later its clinical use was discontinued due to the development of severe local skin reactions with blistering.
The invention of an anesthetic based on an eutectic mixture of lidocaine 2.5% and prilocaine 2.5% made it possible to satisfy two main requirements affecting penetration through intact skin and the provision of local anesthesia. Firstly, it must have a high concentration (in each fat drop the combined concentration of anesthetics reaches up to 80%), which allows it to overcome the lipophilic keratin structures of the skin, and secondly, it must contain a sufficient amount of water to moisturize the skin and improve the absorption of the drug through intact areas of the skin . The low content of anesthetics in the cream allows you to avoid toxic reactions, provided that the recommended doses (no more than 60 g) and areas of treated surfaces (no more than 600 cm2 for adults) are observed [7].
Practicing dermatologists and cosmetologists will be interested in a new drug - Acriol Pro
, which contains 2.5% lidocaine and 2.5% prilocaine (Fig. 5).
Rice. 5. Structure of amide-type local anesthetics lidocaine (a) and prilocaine (b). Note. 1 - hydrophobic aromatic group, providing passive diffusion of compounds through the membrane of nerve cells; 2 - hydrophilic center containing a tertiary (lidocaine) or secondary (prilocaine) nitrogen atom that interacts with the receptor on the inner surface of the nerve fiber membrane; 3 - aliphatic chain connecting the lipophilic and hydrophilic parts of the molecules.
Clinical studies of topical local anesthetics
In Russia, clinical studies using a cream with 2.5% lidocaine and 2.5% prilocaine were conducted by T.I. Zhigultsova et al. [8]. The study involved 382 patients aged from 2 to 60 years. Patients underwent various manipulations that required pain relief: biorevitalization ( n
=30), injection contour plastic (
n
=27), cosmetic tattooing (
n
=37), removal of benign skin neoplasms using diathermocoagulation (
n
=180), removal of hyperpigmentation, pigmented flat benign neoplasms such as Becker’s nevus, Spitz’s nevus using dermabrasion (
n
=22), microcrystalline dermabrasion (
n
=30), electrolysis (
n
=56). The authors noted a good analgesic effect for all manipulations performed. Side effects were observed in 9 patients and manifested as a temporary local reaction of the skin in the form of redness; in 4 patients, itching and burning were observed during application of the cream, which disappeared after removal of the cream.
The effectiveness of a cream with 2.5% lidocaine and 2.5% prilocaine was assessed for patients requiring aesthetic correction using permanent tattooing [9]. A good result of anesthesia and a high level of safety of using this cream have been shown in the category of patients who require one-stage complex correction (interciliary permanent tattooing is carried out simultaneously with correction of the lips with small volumes of contour plastic preparations and elimination/reduction of the depth and severity of wrinkles in the neck area with biorevitalizant preparations. Notes by the author the advantages of this anesthetic in areas of tattooing (eyebrows, eyelids), which have maximum pain during procedures, and the inconvenience of local injection anesthesia by introducing a local anesthetic by changing the shape of the tattoo object, which is also accompanied by the highest risk of possible complications.
All researchers note the availability of anesthesia using a cream with 2.5% lidocaine and 2.5% prilocaine, a sense of comfort, safety, relaxation in the patient and convenience during the procedure. However, pain is not only associated with physical impact - it can be provoked by suggestion. In a study by P. Aslaksen et al. [10] studied the extent to which knowledge of the effect of analgesic therapy influences the reduction of pain. Healthy volunteers ( n
=142) were divided into six groups. Participants in group 1 received anesthesia (2.5% lidocaine and 2.5% prilocaine cream) and were informed about it; in the 2nd group, anesthesia was performed, but they reported the expectation of hyperalgesia; participants in groups 3 and 4 received a placebo with the same information; in group 5 they received pain relief without information; in group 6 they received painful stimulation without anesthesia. Pain was stimulated by heating the skin area to 48 °C and was assessed based on the volunteers' feedback and blood pressure before and after applying the cream and pain stimulation. Results showed that pain was subjectively and objectively less severe in the group receiving positive pain relief information and greater in the hyperalgesia groups, regardless of drug or placebo use. These results indicate that emotional factors can significantly influence the effect of analgesia, so the product should be comfortable for patients to use.
In a double-blind, randomized, placebo-controlled study, 2.5% lidocaine and 2.5% prilocaine cream were used for cryotherapy of warts of the sole of the feet [11]. Cream ( n
=32) or placebo (
n
=32) was applied in a thick layer locally in the wart area under an occlusive dressing for 60 minutes. Anesthesia was well tolerated, but with deep lesions the effectiveness was insufficient.
Topical local anesthetics are used in the treatment of keloids. A cream with 2.5% lidocaine and 2.5% prilocaine showed better efficacy than a cream with a combination of lidocaine/tetracaine in laser treatment of tattoos and keloids in acne [12].
In a study by E. Hernandez et al. [13, 14] it was shown that the effectiveness of a cream with 2.5% lidocaine and 2.5% prilocaine is 2 times higher compared to 40% lidocaine ointment during laser procedures.
Thus, a number of conclusions can be drawn.
An urgent task of modern cosmetology is the selection of optimal anesthesia methods for carrying out invasive cosmetic procedures. Currently, topical local anesthetics with a minimal amount of active anesthetic are the preferred means of reducing procedural morbidity.
The emotional state of the patient significantly influences the effectiveness of anesthesia, so anesthesia should be convenient and comfortable for the patient.
The combination of 2.5% lidocaine and 2.5% prilocaine is widely used for anesthesia in the practice of dermatologists and cosmetologists throughout the world. In Russia, only this combination has registration status as a medicinal product. The results of Russian and foreign studies allow us to conclude that this combination is highly effective and safe, and a number of advantages, such as the presence of an anti-inflammatory effect, high compliance and long-term effects, allow us to recommend the combination of 2.5% lidocaine and 2.5% prilocaine as the drug of choice among local topical anesthetics.
For dermatologists and cosmetologists, a new drug from Akrikhin JSC - Akriol Pro
(2.5% lidocaine and 2.5% prilocaine). The use of this product meets modern healthcare needs and can be implemented as part of an import substitution program.
The authors declare no conflict of interest.
Choice of local anesthetic
articaine anesthetics are recommended and widely used (Zoryan E.V., Rabinovich S.A., Matveeva E.G., 2007; Rabinovich S.A., Vasiliev Yu.L. , 2011). This is due to a number of pharmacological properties. Articaine 4% has relatively low fat solubility compared to lidocaine and mepivacaine and passes less through histohematic barriers.
The metabolism of articaine occurs much faster compared to other anesthetics. Thus, the half-life (t1/2) of articaine is 20 minutes, t1/2 of lidocaine is 90 minutes, t1/2 of mepivacaine is 114 minutes.
Other amide anesthetics: mepivacaine, lidocaine - are the anesthetics of choice in pediatric dentistry for a number of reasons. In the Russian Federation, 2% lidocaine is not available in carpuled form and its use in pediatric practice is limited by the capabilities of outdated technology: ampoules, plastic syringes, large-sized and diameter needles.
Mepivacaine 3% does not contain preservatives or vasoconstrictors. This anesthetic is recommended for use if a child has a concomitant pathology and is intended for short-term interventions. In children with bronchial asthma, the use of 3% mepivacaine (without epinephrine) for local anesthesia is indicated (Zoryan E.V., Rabinovich S.A., Matveeva E.G., 2008). This is due to the fact that this drug does not contain sulfites (epinephrine stabilizer), which can cause an attack of bronchospasm.
Children with pathologies of the cardiovascular system, including congenital ones in the compensation stage, are at risk of developing complications. The use of vasoconstrictors in this category of patients is relatively contraindicated. If possible, non-vasoconstrictor anesthetics should be used, such as 3% mepivacaine.
anesthetic_activity_and_toxicity
Local anesthetics of the ester groupAnesthetics of the ester group undergo hydrolysis in tissues more quickly, since the ester bonds are unstable.
In the blood, their hydrolysis is accelerated by pseudocholinesterase. Anesthetics of this group act for a short time. DICAINE.
Synonyms: Amethocaine, Anethaine, Decicain, Felicain, Foncaine, Intercain, Medicain, Pantocain, Pontocaine hydrochloride, Rexocaine, Tetracaini hydrochloridum, Tetracaine hydrochloride, etc. Due to high toxicity (10 times more toxic than novocaine), the drug is used only for topical anesthesia of the mucous membrane membranes of the mouth and nose.
It is advisable to use 0.25%, 0.5% and 1% solutions. In some cases, most often when anesthetizing small areas, 2–3% solutions of dicaine can be used. The highest single dose of the drug for adults is 0.09 g (3 ml of a 3% solution). Since the drug is easily absorbed and a slight excess of the therapeutic dose can cause severe intoxication and even death, it is not used in pediatric dentistry. ANESTHESIN.
Synonyms: Benzocaine, Aethylis aminobenzoas, Anaesthalgin, Anaesthicin, Anaesthin, Benzocain, Ethoforme, Ethylis aminobenzoas, Ethyl aminobenzoate, Norcain, Parathesine, Rhaetocain, Topanalgin, etc. The substance is not soluble in water.
Can be used for superficial anesthesia in the form of powders or 5–20% oil solutions. For anesthesia of wound and ulcerative surfaces, it can be used in the form of a 5–10% ointment. The highest dose for adults: single dose 0.5 g, daily dose 1.5 g. NOVOCAINE.
Synonyms: Aethocain, Allocaine, Ambocain, Aminocaine, Anesthocaine, Atoxicain, Cerocain, Chemocain, Citocain, Ethocain, Genocaine, Herocaine, ISOCain, Jenacin, Maresaine Minocain, Naucain, Neocaine, Pancain, Paracaine, Planocaine, Polocainum, Procaine, Procaini Hydrochloridum , Procaine hydrochloride, Protocaine, Sevicaine, Syncaine, Syntocain, Topocaine, etc. In terms of activity, novocaine is 4–5 times inferior to dicaine.
For infiltration anesthesia, 0.25%, 0.5% and 1% solutions are used, and for conduction anesthesia, 1% and 2% solutions are used. It must be taken into account that with the same total dose of the drug, the higher the concentration of the solution used, the higher the toxicity. The drug has moderate vasodilating properties. The highest single dose for adults: when using a 0.25% solution, no more than 500 ml (1.25 g); 0.5% solution - 150 ml (0.75 g); 1% solution - 75–100 ml (0.75 g) and 25–30 ml of 2% solution (0.5 g). The total dose should not exceed 2 g. With the resorptive effect (the effect of drugs or toxic substances that manifests itself after they are absorbed into the blood) of novocaine, depression of the central nervous system, moderate analgesic, and anti-shock effect are noted. The drug has a ganglion-blocking, vasodilating, antiarrhythmic effect, and improves microcirculation. Novocaine is low-toxic, but often causes allergic reactions (stomatitis, dermatitis, Quincke's edema and even anaphylactic shock). With increased sensitivity to novocaine, the patient experiences dizziness, weakness, drop in blood pressure, collapse, shock. Therefore, when collecting anamnesis, you should pay attention to the patient’s tolerance not only to novocaine, but also to other anesthetics similar in structure to novocaine (anesthesin and dicaine), since there may be cross-allergy to them. Novocaine reduces the activity of sulfonamides, since one of its metabolites is para-aminobenzoic acid, and the antimicrobial effect of sulfonamides is based on competitive antagonism with para-aminobenzoic acid. Local anesthetics of the group of complex amides
Local anesthetics of the amide group are inactivated more slowly in the body, are not destroyed by blood cholinesterase, act longer, and therefore are more effective.
Their main advantage is that they diffuse better into the tissue at the injection site, act faster, have a larger anesthesia zone and stronger interaction with tissue, which prevents the local anesthetic from entering the bloodstream. LIDOCAINE
. Synonyms: Xycaine, Xylocaine, Lidestin, Acetoxyline, Alocaine, Anestacon, Anestecain, Astracaine, Dolicaine, Dulcicaine, Esracaine, Fastocaine, Leostesin, Lidestin, Lidocaine, Lidocard, Lidocaton, Lignocain, Maricain, Nulicaine, Octocaine, Remicaine, Solcain, Stericaine, Xycain, Xylesin, Xylocain, Xylocard, Xylocitin, Xyloton, Xylotox, etc. Lidocaine is the first amide anesthetic used in dentistry, it is four times more effective than novocaine and approximately twice as toxic, has a deeper and longer-lasting anesthetic effect than novocaine. This allowed it, in the 50s, to become one of the most popular anesthetics used in dentistry. According to its chemical structure, lidocaine is an acetanilide derivative. Unlike novocaine, it is not an ester, is metabolized more slowly in the body and acts longer than novocaine. Due to the fact that during its metabolism in the body there is no formation of para-aminobenzoic acid, it does not have an antisulfonamide effect and, unlike novocaine, can be used in patients receiving sulfonamide drugs. Along with local anesthetic activity, lidocaine has pronounced antiarrhythmic properties. Lidocaine is a strong local anesthetic that causes all types of local anesthesia: terminal, infiltration, conduction and is considered the ancestor of all amide drugs. Compared to novocaine, it acts faster, stronger and longer. The relative toxicity of lidocaine depends on the concentration of the solution. In low concentrations (0.5%) it does not differ significantly in toxicity from novocaine; with increasing concentration (1% and 2%), toxicity increases (by 40–50%). For infiltration and conduction anesthesia in dentistry, a 2% anesthetic solution is used, and for terminal (application) anesthesia of the oral mucosa, a 10% aerosol solution produced abroad (lidestin) is used; in surgery, the aerosol is used when changing dressings and opening abscesses etc. The aerosol can contains 750 doses of 10 mg lidocaine. The amount of sprayed drug depends on the surface to be anesthetized. In adults, the dose should not exceed 200 mg, i.e. 20 sprays; in children over 2 years of age, 1–2 doses of the drug are prescribed once. The aerosol should not come into contact with the eyes. Lidocaine, used in doses that do not cause seizures, has a sedative effect. The drug is contraindicated in patients with severe liver pathology. The highest single dose for adults is a 2% solution up to 20 ml. With rapid entry of the drug into the bloodstream, a decrease in blood pressure and collapse may be observed; reducing the hypotensive effect is achieved by administering vasoconstrictors. Contraindications for the use of lidocaine are as follows: sick sinus syndrome in elderly patients;
- severe bradycardia;
- cardiogenic shock;
- severe liver disorders;
- hypersensitivity to the drug.
Pregnant and lactating women should be prescribed lidocaine according to strict indications. In children under 2 years of age, the use of lidocaine aerosol is allowed only after its preliminary application to a cotton swab. In case of overdose, psychomotor agitation, tremor, clonic-tonic convulsions, collapse, and central nervous system depression are observed. To treat this complication, short-acting barbiturates and benzodiazepine tranquilizers are used. With the simultaneous administration of lidocaine and beta-blockers (drugs used for paroxysmal tachycardia, extrasystoles, angina pectoris, hypertension - Inderal, Trazicorcor), the resorptive effects (including toxic) of lidocaine may increase due to the weakening of its inactivation in the liver. In this case, the dose of the drug is reduced. It is irrational to prescribe lidocaine simultaneously with antiarrhythmic drugs - drugs used to treat paroxysmal tachycardia, atrial fibrillation and extrasystole (ajmaline, quinidine, etc.) due to increased cardiodepressive effects. Combined use with procainamide (an antiarrhythmic drug) can cause central nervous system stimulation and hallucinations. The combined administration of lidocaine with MAO inhibitors (antidepressants, for example, iprazide), polymyxin B (an antibiotic used for staphylo-, strepto-, pneumo-, gono- and meningococcal infections), diphenin (an anticonvulsant used to treat epilepsy) is also contraindicated. Storage: the drug should be stored in a place protected from light at room temperature. MEPIVACAIN.
Synonyms: Scandicain, Scandonest, Carbocain, Isocain, Mepivastesin, Mepicaton, Mepidont. Used for infiltration and conduction anesthesia in the form of a 3% solution, 2% solution with adrenaline (1/100,000) and norepinephrine (1/100,000). In terms of effectiveness and toxicity, a 2% solution of mepivacaine is approximately equal to a 2% solution of lidocaine (the drug does not cause a cross-allergic reaction with ether anesthetics). Unlike most active substances in anesthetic solutions, which have vasodilatory properties, mepivacaine has a vasoconstrictor effect, which allows the use of a solution with a reduced vasoconstrictor content. In this regard, a 3% solution of mepivacaine hydrochloride in therapeutic dentistry today is the drug of choice for patients for whom the use of vasoconstrictors is contraindicated. Contraindications for the use of mepivacaine are as follows:
- allergy to local anesthetics belonging to the same group;
- severe myasthenia gravis;
- low plasma cholinesterase levels;
- serious liver disorders: cirrhosis, hereditary or acquired porphyria.
The maximum single dose of the drug is 2.7 mg per 1 kg of body weight or 162 mg (3 carpules) for a weight of 60 kg. For children, the total dose should not exceed 1 carpule and is 1.33 mg per 1 kg of body weight. In case of overdose, clonic convulsions appear as a result of intoxication of the nervous system. ARTICAINE.
Synonyms: ultracaine, carticaine, septonest, ubistezin, etc. A drug for local anesthesia in dentistry.
Articaine is a local anesthetic of the amide type of the thiafene group. The drug provides a reliable anesthetic effect. Wound healing after surgical interventions proceeds without complications, which is due to good tissue tolerance and minimal vasoconstrictor effect. Due to the low content of adrenaline in articaine preparations, its effect on the cardiovascular system is weak: there is almost no increase in blood pressure and heart rate. Articaine preparations have low toxicity. However, articaine preparations produced by different companies under different trade names differ to one degree or another in composition: Ultracaine D-S
- 1 ml of the drug contains: articaine hydrochloride 40 mg, adrenaline hydrochloride 6 mcg.
Other ingredients:
sodium metabisulfite, sodium chloride, water for injection.
Ultracaine D-S Forte
- 1 ml of the drug contains: articaine hydrochloride 40 mg, adrenaline hydrochloride 12 mcg.
Other ingredients:
sodium metabisulfite, sodium chloride, water for injection.
Ubistezin Forte
- 1 ml of the drug contains: articaine hydrochloride 40 mg, adrenaline hydrochloride 12 mcg.
Other ingredients:
sodium metabisulfite, sodium chloride, water for injection
Septanest
- 1 ml of the drug contains: articaine hydrochloride 40 mg, adrenaline hydrochloride 10 mcg.
Other ingredients:
sodium metabisulfite, sodium chloride, EDTA, water for injection Articaine acts faster than lidocaine, the effect of the drug begins within 1–3 minutes, the duration of anesthesia is 60–180 minutes. It has a high diffusivity and degree of binding to plasma proteins (95%), low fat solubility. Articaine penetrates well into tissues, can provide anesthesia of the palate after buccal infiltration anesthesia and anesthesia of the pulp after infiltration anesthesia in the lower jaw from 35 to 45. The lipophilicity of articaine is less than that of other amide anesthetics, however, low toxicity in comparison with lidocaine and mepivacaine allows the use of this the drug in the form of a 4% solution of articaine hydrochloride with adrenaline (epinephrine) in dilutions of 1:100000 and 1:200000. Due to the fact that articaine preparations do not usually contain paraben (an antibacterial preservative), these anesthetics can be used in patients who are allergic to parahydroxybenzoates or chemically related structures. The stability of the anesthetic is achieved by high quality packaging (ampoules and carpules) and high chemical purity of the active substance. However, it should be remembered that Ultracain, produced in 20 ml bottles, contains 0.05 mg of methylparaben. The maximum single dose of the drug solution is 12.5 ml (7 carpules) for an adult weighing 70 kg (7.0 mg/kg articaine). When using articaine preparations, the following side effects are possible:
- From the central nervous system: depending on the dose used, cases of impaired consciousness up to its loss have been described; breathing problems; muscle tremors, involuntary muscle twitching, sometimes progressing to generalized convulsions; nausea, vomiting.
- On the part of the visual organs: blurred vision, transient blindness, diplopia (rare).
- From the cardiovascular system: moderately severe hemodynamic disturbances, manifested by a decrease in blood pressure, tachycardia or bradycardia.
- Allergic reactions: swelling or inflammation at the injection site; in other areas - redness of the skin, itching, conjunctivitis, rhinitis, angioedema of varying severity (including swelling of the upper and/or lower lip and/or cheeks, glottis with difficulty swallowing, urticaria, difficulty breathing). All these phenomena can progress to the development of anaphylactic shock.
- Local reactions: swelling or inflammation at the injection site.
- Other: headaches (probably associated with the presence of adrenaline in the drug). Other side effects caused by the action of adrenaline (tachycardia, arrhythmia, increased blood pressure) occur rarely, since the concentration of adrenaline is insignificant.
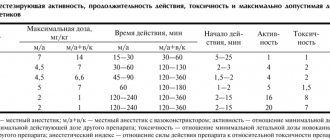
- Drug interactions: The hypertensive effect of sympathomimetic amines such as epinephrine may be enhanced by tricyclic antidepressants and MAO inhibitors. Interactions of this type have been described for epinephrine and norepinephrine when used as vasoconstrictors at concentrations of 1:25,000 and 1:80,000, respectively. Although the concentration of epinephrine in articaine preparations is significantly lower, this possibility should nevertheless be taken into account. Sometimes, accidental intravascular injection can lead to the development of ischemic zones at the injection site, in some cases progressing to tissue necrosis. Damage to the facial nerve, up to the development of facial paralysis, occurs only when the injection technique is violated. Comparative characteristics of local anesthetics
| Novocaine | Lidocaine | Mepivacaine | Artikain | |
| Plasma protein binding | 5,8 % | 50 % | 78 % | 95 % |
| Half-life in min. | – | 96 | 114 | 29 |
| Anesthetic activity* | 1 | 4 | 4 | 5 |
| Toxicity* | 1 | 2 | 1,7 | 1,5 |
| Duration of anesthesia (in minutes) without a vasoconstrictor | 15–30 | 30–60 | 45–90 | 60 |
| Duration of anesthesia (in minutes) with a vasoconstrictor | 4030 | 130120 | 130120 | 180 |
| Maximum permissible dose (mg/kg) with vasoconstrictor | 14 | 7 | 6,6 | 7 |
| Maximum permissible dose (mg/kg) without vasoconstrictor | 7 | 4,5 | 4,5 | 5 |
| Speed of action | Slow | Fast | Fast | Very fast |
The use of local anesthetics in recommended doses is relatively safe (with the exception of allergic reactions). Statistics of complications and side effects during local anesthesia are not very accurate and are more likely related to the error in the choice of drug and its dosage. The practice of using local anesthetics should take into account the individual maximum dose of the drugs used. It is usually determined according to the patient's body weight. The dentist should always strive to achieve effective pain relief using the minimum amount of anesthetic. Recommendations, in this regard, suggest using a dose not exceeding 50% of the maximum toxic dose. In cases where the volume of dental intervention requires the use of local anesthetics in a dosage exceeding 50% of the maximum dose, it is necessary to ensure the possibility of providing the patient with anesthesia, including free access for intravenous injections, oxygen inhalation, assisted or artificial ventilation. It is very important to collect the following anamnestic data before using local anesthesia:
- whether local anesthesia was previously used;
- were there any complications of local anesthesia;
- whether there were allergic reactions to local anesthetics;
- identify risk factors (chronic diseases).
Reference materials
| Indicators | [ Notes | |
| CHARACTERISTICS OF LOCAL ANESTHETICS | ||
| Action point | sensory nerve endings and conductors | |
| Chemical structure | weak grounds | |
| Solubility in water | sparingly soluble | |
| Water soluble form | hydrochloric acid salts of local anesthetics | |
| Mechanism of action | hydrolysis of the salt, release of the anesthetic base, highly soluble in fats and penetrating through the phospholipid membrane of the nerve fiber; interaction with membrane receptors; disruption of ion transport (primarily Na) across the membrane | |
| Pharmacological effect | blockade of nerve impulses | |
| Local anesthetics: | ||
| a) ester groups | novocaine, anestezin, dicaine | |
| b) amide groups | lidocaine, trimecaine, mepivacaine, articaine, bu-pivacaine | |
| Novocaine | ||
| Synonym | procaine | |
| pKa | 8,9-9,1 | |
| Hydrolysis rate | hydrolyzes slowly in tissues | |
| Advance speed anesthetic effect | the effect develops within 6-20 minutes | |
| Fat solubility | low | |
| Types of anesthesia | infiltration and conduction | |
| Duration of anesthesia | 1 5-30 minutes | |
| Effect on blood vessels | expanding | |
| Duration of anesthesia from vasoconstrictor | up to 60 minutes | |
| Effective concentrations for dental practice | 1-2% | |
| pH of solution without vasoconstrictor | 5,0-6,5 | |
| pH of solution with vasoconstrictor | 3,5-5,5 | |
| Metabolism | quickly hydrolyzed in the body by esterases in plasma, tissues and liver | |
| Indicators | Notes | |
| Local anesthetic activity | moderate | |
| Breadth of therapeutic action | big | |
| Maximum dose | 500mg | |
| Action on the central nervous system | depressing | |
| Other pharmacological effects | ganglion blocking, antiarrhythmic, antispasmodic, analgesic, antishock, antipruritic, improves microcirculation | |
| Side effects | allergic reactions, with hypersensitivity - general weakness, nausea, dizziness, hypotension, increased heart rate, collapse, allergic skin reactions, stomatitis, Quincke's edema, anaphylactic shock | |
| Overdose | dizziness, paresthesia, motor agitation, epileptic convulsions, shortness of breath, collapse | |
| Contraindications | hypersensitivity to the drug, congenital pseudocholinesterase deficiency, myasthenia gravis, hypotension, treatment with sulfonamides, purulent process at the injection site | |
| Cautions | use with caution in severe diseases of the heart, liver and kidneys | |
| Lidocaine | ||
| Synonyms | xycaine, xylodont, xylocaine, lignocaine, li-docart, luan, octocaine | |
| Chemical structure | amide derivative of xylidine | |
| pKa | 7,7-7,9 | |
| Hydrolysis rate | quickly hydrolyzes in tissues | |
| Speed of onset of anesthetic effect | the effect develops within 2-4 minutes | |
| Fat solubility | high | |
| Types of anesthesia | superficial, infiltration, conductive | |
| Duration of anesthesia | pulp anesthesia using 2% lidocaine - 5-10 minutes, soft tissue - 60-120 minutes; in dental practice, lidocaine with a vasoconstrictor is used; lasts up to 75 minutes | |
| Effect on blood vessels | actively dilates blood vessels | |
| Duration of anesthesia from vasoconstrictor | with the addition of adrenaline hydrochloride (1:50000 or 1:100000), the duration of pulpal anesthesia is 60 minutes, soft tissue anesthesia is 3-5 hours | |
| Effective concentrations for dental practice | for infiltration and conduction anesthesia in dentistry - 1-2% solution, for surface anesthesia - 4-10% solution; for terminal anesthesia of the mucous membranes, use no more than 2 ml of 10% lidocaine solution (200 mg) | |
| pH of solution without vasoconstrictor | 6,5 | |
| pH of solution with vasoconstrictor | 5,0-5,5 | |
| Metabolism | metabolized in the liver by microsomal oxidases | |
| Local anesthetic activity | is 2-4 times more active than novocaine | |
| Maximum dose | 4.4-6.6 mg/kg body weight for adults and children, but not more than 300 mg | |
| Other pharmacological effects | sedative and antiarrhythmic | |
| Side effects | headache, nausea, anxiety, dizziness, hypotension, collapse, tinnitus, blurred vision, bradycardia, allergic skin reactions, stomatitis, convulsive twitching, tremor, rarely - allergic reactions, anaphylactic shock | |
| Overdose | the phase of stimulation of the central nervous system is replaced by a phase of inhibition; drowsiness, blurred vision, pallor, nausea, vomiting, decreased blood pressure, muscle tremors, hypotension, vascular collapse, convulsions, depression of the respiratory center are observed | |
| Contraindications | hypersensitivity, weakness of the sinus node, atrioventricular block, severe bradycardia, cardiogenic shock, liver pathology, myasthenia gravis, epileptiform seizures (including history) | |
| Cautions | Use with caution during pregnancy and breastfeeding | |
| Mepivacaine | ||
| Synonyms | isocaine, mepivastezin, mepidont, scandicaine, scandonest | |
| Chemical structure | amide derivative of xylidine | |
| pKa | 7,6 | |
| Hydrolysis rate | quickly hydrolyzes in tissues | |
| Speed of onset of anesthetic effect | the effect develops within 2-4 minutes | |
| Fat solubility | less than lidocaine | |
| Types of anesthesia | infiltration, conductive | |
| Duration of anesthesia | the duration of pulpal anesthesia caused by 3% mepivacaine without a vasoconstrictor is 20-40 minutes, soft tissue anesthesia - 2-3 hours | |
| Duration of anesthesia from vasoconstrictor | addition of a vasoconstrictor (1:200,000 levonorderphin, 1:200,000 adrenaline) to a 2% solution of mepivacaine extends pulp anesthesia to 60 minutes, and soft tissue anesthesia to 3-4 hours | |
| Effect on blood vessels | does not have a vasodilatory effect | |
| Effective concentrations for dental practice | 3% solution without vasoconstrictor, 2% solution with vasoconstrictor | |
| pH of solution without vasoconstrictor | 4,5 | |
| pH of the solution with vasoconstrictor | 3,0-3,5 | |
| Metabolism | metabolized in the liver by microsomal oxidases of mixed function with the formation of inactive metabolites; Hydroxylation and M-demethylation play an important role in the biotransformation process | |
| Local anesthetic activity | is 2-4 times more active than novocaine | |
| Maximum dose | 4.4-6.6 mg/kg body weight for adults and children, but not more than 300 mg | |
| Side effects | mainly with intravascular administration of the drug: euphoria, depression, impaired swallowing, vision, bradycardia, arterial hypotension, convulsions, respiratory depression; allergic | |
| allergic reactions (urticaria, angioedema) are rare | ||
| Overdose | the phase of stimulation of the central nervous system (may not be expressed) is replaced by a phase of inhibition | |
| Contraindications | hypersensitivity, myasthenia gravis, severe liver pathology, porphyria | |
| Cautions | Use with caution in severe cardiovascular diseases, diabetes mellitus, in the elderly, during pregnancy | |
| Artikain | ||
| Synonyms | alfacaine, septonest, ultracaine, ubistezin, cytocartin, brilocaine | |
| Chemical structure | amide derivative of thiophene | |
| pKa | 7,8 | |
| Hydrolysis rate | quickly hydrolyzes in tissues | |
| Speed of onset of anesthetic effect | the effect develops within 1-4 minutes | |
| Fat solubility | lower than lidocaine | |
| Types of anesthesia | infiltration, conductive | |
| Effect on blood vessels | vasodilator effect | |
| Duration of anesthesia from vasoconstrictor | A 4% solution of articaine with a vasoconstrictor (1:100000 or 1:200000 adrenaline) provides pulp anesthesia from 45 to 75 minutes, and soft tissue anesthesia from 2 to 5-6 hours | |
| Effective concentrations for | 4% solution with vasoconstrictor (1:100000 or 1:200000 adrenaline) | |
| dental practice | ||
| pH of solution with vasoconstrictor 1:100000 1:200000 | 4,4-5,2 4,6-5,4 | |
| Metabolism | metabolized in the liver by hydrolysis; additionally, inactivation occurs in tissues and blood by nonspecific esterases | |
| Local anesthetic activity | is 3-5 times more active than novocaine | |
| Maximum dose | 5-7 mg/kg body weight for adults and children, but more than 500 mg | Not |
| Side effects | rarely: allergic reactions, swelling and inflammation at the injection site, headache, blurred vision, moderate hemodynamic and heart rhythm disturbances, diplopia, muscle twitching | |
| Overdose | the phase of stimulation of the central nervous system (may not be expressed) is replaced by a phase of depression, there is a disturbance of consciousness, respiratory depression, until it stops, muscle tremors, convulsions, nausea, vomiting, blurred vision, transient blindness, diplopia | |
| Contraindications | hypersensitivity to articaine, adrenaline, sulfites and other components of the solution, tachyarrhythmia, paroxysmal tachycardia, angle-closure glaucoma, bronchial asthma, blood cholinesterase deficiency, myasthenia gravis | |
| Bupivakaip | ||
| Synonyms | anecaine, marcaine | |
| Chemical structure | amide derivative of xylidine | |
| pKa | 8,1 | |
| Hydrolysis rate | hydrolyzes slowly | |
| Speed of onset of anesthetic effect | in 5-10 minutes | |
| Fat solubility | high | |
| Types of anesthesia | infiltration, conductive | |
| Action on blood vessels | vasodilator effect | |
| Duration of anesthesia from vasoconstrictor | A 0.5% solution of bupivacaine with a vasoconstrictor (1:200,000 epinephrine) provides pulp anesthesia from 90 to 180 minutes, and soft tissue anesthesia from 4 to 12 hours | |
| Effective concentrations for dental practice | 0.5% solution with vasoconstrictor | |
| pH of solution without vasoconstrictor | 4,5-6,0 | |
| pH of the solution with vasoconstrictor | 3,0-4,5 | |
| Metabolism | metabolized in the liver by microsomal oxidases of mixed function with the formation of inactive metabolites; Hydroxylation and M-demegylation play an important role in the biotransformation process | |
| Local anesthetic activity | is 8-10 times more active than novocaine | |
| Maximum dose | 1.3 mg/kg body weight of an adult patient, but not more than 90 mg | |
| Side effects | headache, dizziness, weakness, blurred vision, nausea, vomiting, rarely - allergic reactions | |
| Overdose | cardiac dysfunction, symptoms of central nervous system excitation, hypotension (up to collapse), bradycardia (up to cardiac arrest), ventricular arrhythmias, respiratory arrest, confusion, convulsions | |
| Contraindications | hypersensitivity to the drug or components of the solution, central nervous system diseases (meningitis, tumors, poliomyelitis), intracranial bleeding, severe hypotension, cardiac decompensation, pernicious anemia with neurological symptoms, severe hypoxia, hypercapnia, pregnancy, children (up to 1 2 years) | |
Risks and complications
Local anesthesia is generally considered very safe. For minor surgeries it is safer than general anesthesia.
There may be tingling and pain, and there may be bruising as you take the drug and wear it off, but this is usually minor.
A person who has had local anesthesia must be careful not to get hurt when they cannot feel pain, such as when biting their cheek after dental treatment.
Temporary side effects that affect some people include:
- blurred vision, dizziness and vomiting
- headache
- muscle twitching
- persistent numbness, weakness, or tingling
Some people may have an allergic reaction. The patient may experience hives, itching, and difficulty breathing.
Cyanosis may occur, in which the skin turns bluish due to poor circulation or insufficient oxygenation of the blood.
In very severe cases, a person may experience CNS depression, in which the central nervous system slows down too much, resulting in a decrease in breathing and heart rate. This can lead to cardiac arrest if blood stops pumping to the heart.
An overdose of local anesthetic can lead to seizures. This can be life-threatening.
Preparing for local anesthesia
If the patient is undergoing surgery with local anesthesia, the doctor should explain in advance how to prepare.
Patients should tell their doctor if they are using any medications, especially if they are blood thinning agents such as aspirin or warfarin.
Your doctor may instruct you not to eat anything for several hours before surgery. It is also important not to drink alcohol for 24 hours before taking the anesthetic.
In the doctor's office, the doctor applies a local anesthetic to the appropriate area of the body. It will start to feel numb.
The doctor will not act if the patient does not feel numb.
The anesthetic will prevent any pain, but the patient may still feel pressure during surgery.
Depending on what the procedure is and how anxious the patient feels, a sedative may be prescribed at the same time. This will help the patient feel calm and less anxious.
The doctor will monitor the amount of oxygen in your blood using a small device placed on your finger. In rare cases, a plastic nasal tube will be used to provide supplemental oxygen.