Local anesthetics (local anesthetics) are medications that cause loss of sensitivity in nerve endings or block the transmission of nerve impulses along fibers.
It is important not to confuse local anesthesia with general anesthesia. With local anesthesia, there is a loss of pain, temperature and tactile (touch) sensitivity, while the effect is limited to a small area of the body around the site of injection of the drug - the local anesthetic. In addition, with local anesthesia, the patient is conscious, unlike general anesthesia.
Types of anesthesia
There are three main types of local anesthesia:
- Superficial (terminal) - develops at the site of application of the local anesthetic, most often on the mucous membranes - eyes, mouth, stomach, etc., as well as on the surface of the skin;
- Conduction - develops when a local anesthetic is introduced into a large nerve trunk, and sensitivity is lost in those areas for which this nerve is responsible (a separate type of conduction anesthesia is epidural anesthesia, when a drug solution is injected into the space above the dura mater of the spinal cord - sensitivity is lost in the lower part of the body);
- Infiltration – occurs when tissues of the human body are layer-by-layer soaked with a solution of local anesthetic (the most common type of local anesthesia).
A group feature of drugs for local anesthesia is the obligatory presence of the suffix –CAIN in the name, thanks to which the local anesthetic can be immediately recognized among other drugs.
Trimecain (Trimecainum)
Synonyms: 2,4,6 - diethylaminoacetic acid anilide trimethylacetylate hydrochloride. Trimecaine is similar in pharmacological action to lidocaine. Its anesthetic activity is 2-3 times higher than novocaine, it acts faster and longer, and does not irritate tissues. Trimecaine is somewhat more toxic than novocaine, especially in higher concentrations. The drug dilates blood vessels and is used in dental practice with vasoconstrictors. Indications for use • Infiltration anesthesia for interventions on the upper jaw. • Conduction anesthesia. • Superficial anesthesia of the oral mucosa. In addition, trimecaine, like lidocaine, can be used for ventricular extrasystoles and tachyarrhythmia. Contraindications Contraindications are hypersensitivity to trimecaine, weakness of the sinus node, AV block, severe bradycardia, cardiogenic shock, liver and kidney pathology. Method of application It is used mainly for conduction and infiltration anesthesia, less often for surface anesthesia. Used for injection in the form of a 2% solution, topically - in the form of a 3-5% ointment. To slow down absorption, add adrenaline to the trimecaine solution (0.1% solution, 1-2 drops per 5-10 ml of trimecaine solution). The maximum total dose for injection is 300 mg. Interaction with other drugs Vasoconstrictors enhance and prolong the effect of trimecaine. Preliminary administration of tranquilizers and sleeping pills increases the effect of trimecaine.
Indications for use
Local anesthetic preparations are widely used in dentistry for infiltration anesthesia - during tooth extraction (removal) and minor operations on the periodontium (gums).
In order to achieve superficial anesthesia, local anesthetics are used in ophthalmology - in the form of eye drops during operations on the conjunctiva (for laser vision correction, removal of foreign bodies from the eye) and the cornea.
In addition, local anesthetics for superficial anesthesia are used for wounds, minor surgical operations on the skin and mucous membranes, and for ulcers, including gastric ulcers - some local anesthetic preparations (for example, benzocaine) are part of combination drugs that reduce the acidity of gastric juice (antacids).
Certain drugs (lidocaine) are used in endoscopic diagnostics to facilitate the procedure - anesthesia of the pharynx before inserting a tube through the mouth or nose; placement of a urinary catheter.
To achieve conduction anesthesia, local anesthetics are used for pain relief during childbirth (epidural anesthesia), operations on the pelvic organs and lower extremities.
The local anesthetic lidocaine, in addition to its local anesthetic effect, has an antiarrhythmic effect, so it is also used for heart rhythm disturbances - arrhythmias.
Additives to anesthetics:
1) Vasoconstrictors
Vasoconstrictors - added to increase the effectiveness of local anesthesia, as well as to slow down the entry of anesthetics into the bloodstream.
Adrenalin
Adrenaline is used most often. A relatively safe dilution of adrenaline is a concentration of 1:200,000, which can only be achieved in capsule preparations.
Norepinephrine
Norepinephrine is used less frequently as a vasoconstrictor. Norepinephrine, unlike adrenaline, is less dangerous in patients with cardiac pathology (coronary heart disease), but the risk of developing a hypertensive crisis with concomitant hypertension is higher.
Used instead of adrenaline for thyrotoxicosis and diabetes. Contraindicated in glaucoma.
Filipressin (octapressin)
Filipressin is a synthetic drug that does not have a direct effect on the heart. The effect is associated with its direct effect on the smooth muscles of blood vessels. Contraindicated during pregnancy, because may cause myometrial contractions.
Undesirable systemic effects of vasoconstrictors:
- rise in blood pressure,
- tachycardia,
- heart rhythm disturbances,
- angina attacks,
- centralization of blood circulation,
- headache.
Risk group when using vasoconstrictors
: patients with glaucoma, thyrotoxicosis, diabetes mellitus; patients taking drugs rauwolfine, thyroid hormones, tricyclic antidepressants, antidepressants - MAO inhibitors.
2) Preservatives
Parabens
(methylparaben
–
methyl 4-hydroxybenzonate, ethylparaben)
Parahydroxybenzoic acid esters (parabens) are used as preservatives, which have antibacterial and antifungal effects.
It must be remembered that parabens are included in various cosmetics, creams, toothpastes and can provoke contact dermatitis, so there is a real danger of an allergy to the local anesthetic drug.
Para-aminobenzoic acid (PABA), which is a metabolite of novocaine, has a similar structure to parabens, which can cause cross-allergic reactions. Many drugs (sulfonamides, oral antidiabetic drugs, furosemide, etc.) are derivatives of PABA. Therefore, it is not advisable to use drugs containing parabens if you have a drug allergy to the listed medications.
The presence or absence of parabens in the local anesthetic drug is indicated by the manufacturer. Parabens can cause sensitization of the body and anaphylactic shock.
3) Stabilizers
Sulfites
(sodium or potassium disulfite) are used as vasoconstrictor stabilizers. Allergy to sulfites is most common in patients with bronchial asthma (frequency - about 5%), so you should be especially careful when treating such patients. Sulfites cause edema, urticaria, bronchospasm through irritant receptors, nervous and vagal reflexes.
Classification of local anesthetic drugs
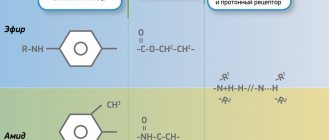
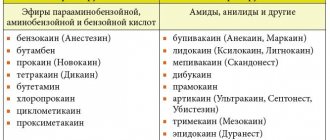
Local anesthetics are classified according to their clinical use (depending on the type of anesthesia caused), as well as according to their chemical structure:
- Agents that are used only for superficial anesthesia: para-aminobenzoic acid esters: benzocaine, tetracaine;
- substituted acetanilide amides: bumecaine, prilocaine.
- para-aminobenzoic acid esters: procaine;
- substituted acetanilide amides: lidocaine.
Articainum
Synonyms: ultracaine, ubistezin, articaine INIBSA, alfacaine, brilocaine, septonest. 4-Methyl-3-[2-propylamnopropionamido]-2-thiophenecarboxylic acid methyl ester. The first local anesthetic of the amide group, having a thiophene ring instead of a benzene ring and an additional ether group, was synthesized in 1969 by H. Rushing et al.
The drug is inferior to lidocaine in fat solubility, which makes it less likely to be absorbed into the blood and enter tissues and organs. To obtain adequate local anesthesia in dentistry, it is used in the form of a 4% solution. Articaine has the highest ratio of activity and toxicity, i.e. has a wide range of therapeutic effects, which makes it the drug of choice for children, the elderly and those with a history of liver and kidney pathology. Compared to other amide anesthetics, it has the largest plasma clearance (3.9 l/min) and the shortest half-life. T1/2 of articaine is about 20 minutes and depends on the content of the vasoconstrictor in the solution. It is not found in breast milk in clinically significant concentrations, indicating its benefits when choosing local anesthetic agents for nursing mothers. The rapidity of metabolism and excretion of articaine determines the absence of accumulation when it is re-administered during a large volume of dental care. Despite the short half-life compared to other amide local anesthetics and high plasma clearance, the drug has an average duration of action. In terms of vasodilatory activity, articaine is similar to lidocaine, which necessitates its use with vasoconstrictors. The high local anesthetic activity of the drug makes it possible to reduce the vasoconstrictor content in its solution to 1:200,000. The low toxicity of articaine allows it to be used in a 4% solution, which has high anesthetic activity. Indications for use • Infiltration anesthesia of interventions on the upper jaw and in the anterior region, including premolars, of the lower jaw.
• Conduction anesthesia. • Intraligamentary anesthesia. • Intraosseous anesthesia. In commonly used concentrations, articaine does not have a surface anesthetic effect, but is superior to lidocaine, prilocaine and mepivacaine in activity during infiltration and conduction anesthesia, allowing the effectiveness of local anesthesia in dentistry in adults to be brought closer to 95-100%. Articaine has a higher activity in inflammation compared to other anesthetics used in dental practice. Since articaine loses its activity to a lesser extent during inflammation, it is the drug of choice for tissue anesthesia in severe purulent-inflammatory processes. Cautions In dental practice, before administering a local anesthetic, it is recommended to carry out an aspiration test to prevent intravascular administration of the drug. All articaine solutions containing vasoconstrictors should be prescribed with caution to patients with cardiovascular and endocrine diseases (thyrotoxicosis, diabetes mellitus, heart defects, hypertension, etc.), as well as those receiving β-blockers, tricyclic antidepressants and MAO inhibitors. If it is necessary to use articaine during pregnancy, lactation, for cardiovascular failure, diabetes mellitus, thyrotoxicosis, the drug of choice is a 4% solution of articaine with adrenaline 1:200,000 or articaine without a vasoconstrictor. Side effects Side effects on articaine preparations are observed in 0.13-0.26% of patients. • Allergic reactions (urticaria, angioedema, anaphylactic shock). • Swelling and inflammation at the injection site. • Moderately severe disturbances of hemodynamics and heart rhythm, headache and nausea.
• With accidental intravascular administration (especially 4% articaine solution containing 1:100,000 adrenaline), ischemia of the injection zone is possible, sometimes progressing to tissue necrosis. When using infiltration methods of administering articaine preparations with adrenaline 1:100,000, changes in hemodynamic parameters in patients are unlikely. To exclude an increase in blood pressure and an increase in heart rate (pulse) when using conduction anesthesia, which may be associated with intravascular entry of the drug, an aspiration test is required before administering the entire dose of the drug. Method of administration and dosage Articaine preparations are used for infiltration and conduction anesthesia. To achieve complete anesthesia when using a 4% solution of articaine with adrenaline 1:200,000 or 1:100,000, from 0.5 to 1.8 ml is used, in some cases an additional injection of 1.0-1.8 ml may be required. Reducing the concentration of articaine solution to 2-3% reduces the effect of the local anesthetic. The maximum dose for adults is 7 mg/kg. The maximum dose for children is 5 mg/kg. It is recommended to use no more than 1/2 of the maximum allowable dose.
Basics of local anesthetic treatment
Preparations for conduction and infiltration anesthesia are produced exclusively in the form of solutions for injection; they are classified as prescription drugs. The administration of these drugs is carried out strictly by medical personnel in a clinical setting and under the mandatory supervision of a doctor.
From the moment of administration of the local anesthetic to the development of local anesthesia, it takes from several minutes to half an hour - it all depends on the specific drug. Therefore, you need to wait for the effect of the drug and not re-introduce it - this is dangerous due to the development of the toxic effect of the local anesthetic.
The duration of the effect of local anesthetics is different and depends on the chemical structure of the drug: esters of para-aminobenzoic acid are quickly destroyed by special esterase enzymes in human tissues, while substituted acetanilide amides are insensitive to the action of these enzymes, and therefore have a much longer local anesthetic effect.
Types of Local Anesthesia
The type and dose of anesthesia will depend on many factors. These include patients' age, weight, allergies, body part being operated on, and any current health conditions.
Various drugs are used to block pain. They can be applied by injection or by applying a spray or ointment.
The drug works by targeting specific nerve pathways to prevent the nerves in the area of application from sending signals to the brain.
Typically, the drug takes effect within a few minutes and wears off within a few hours. A stronger and higher dose will last longer.
Cocaine was the first anesthetic, but is now rarely used. Lidocaine is currently the most widely used local anesthetic, but different drugs are used for different purposes.
For longer procedures, bupivacaine is more suitable, but it may be more painful when first used. Therefore, the anesthesiologist may use lidocaine first and then administer bupivacaine if numbness is required for a longer period.
Synthetic anesthetics are similar in structure to cocaine, but these drugs do not have the same potential for abuse.
Features of treatment with local anesthetics
For conduction and infiltration anesthesia, only sterile solutions of local anesthetics are used.
The effect of local anesthetics is weak or practically absent during inflammation - increased acidity (acidosis) is observed in inflamed tissues, which prevents the entry of local anesthetic drugs into the nerve cell, which is critical for the development of the drug’s effect.
Certain local anesthetics (articaine, lidocaine) can be combined with vasoconstrictor drugs, in particular with adrenaline (epinephrine). This helps the local anesthetic stay at the injection site longer without entering the systemic circulation. At the same time, the duration of the local anesthetic effect of the drug increases several times. In addition, adrenaline reduces the toxic effect of local anesthetics on the body.
Considering that local anesthetics (especially esters) often cause allergic reactions, before using these drugs it is advisable to determine individual sensitivity to them - inject the patient with a small amount of local anesthetic solution under the skin of the forearm and assess the reaction after five to ten minutes.
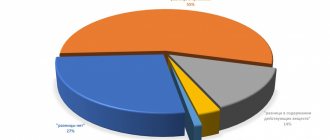
It is impossible to imagine modern dentistry without local anesthesia. Most therapeutic, some orthopedic and almost all surgical interventions are performed after preliminary anesthesia. Articaine-containing local anesthetics, widely used and deservedly considered the most effective and safe, allow many complications to be avoided if the rules of their use are followed correctly [3]. But they also use lidocaine and even procaine (Novocaine), and in maxillofacial surgery - ropivacaine for long-term intra- and postoperative pain relief, so doctors should be well aware of how great the risk of complications is directly associated with the use of local anesthetics (see diagram) .
Let us dwell on systemic toxic reactions to local anesthetics - one of the little-studied complications that can lead to a critical outcome. In contrast to allergic reactions, systemic toxic reactions to local anesthetics are common, especially when high doses of drugs are used. Over the past decades, scientists around the world have carried out a great deal of research and analytical work to study the toxic effect of local anesthetics on the human body and determine the leading signs that distinguish this complication from allergic reactions. The published results of statistical studies convincingly indicate that modern local anesthetic drugs are much less dangerous as allergens (the risk of allergy is 1:2,000,000 injections) and much more likely to cause systemic toxic reactions (the risk is estimated as 1:1000 injections) [12].
Systemic toxic reactions to local anesthetics in maxillofacial surgery and dental practice, in contrast to general surgery, where these drugs are administered in much larger quantities for the purpose of regional anesthesia, are less common, but this complication must be remembered due to the likelihood of a tragic outcome. .
The modern market provides dentists with a wide selection of local anesthetics. When determining the safest drug, it is important to focus primarily on its anesthetic index, duration of effective action and compatibility with other drugs taken by the patient. In table 1 provides information on the maximum doses, duration of action, activity and toxicity of local anesthetics.
Table 1. Anesthetic activity, duration of action, toxicity and maximum permissible dose of various local anesthetics Note. m/a - local anesthetic; m/a+iv/c - local anesthetic with vasoconstrictor; activity - the ratio of the minimum effective dose of novocaine to the minimum effective dose of another drug; toxicity - the ratio of the minimum lethal dose of novocaine to the minimum lethal dose of another drug; anesthetic index is the ratio of the potency of the drug to the relative toxicity of the drug.
The analgesic effect of a local anesthetic is determined by its vasoactivity, lipid solubility, ability to bind to proteins and acidity. Certain adjustments, of course, are made by the somatic status of the patients, as well as the pharmacological interactions that occur in the case of basic drug therapy.
The rate of onset of the analgesic effect, systemic absorption, metabolism and elimination of the local anesthetic determine its physicochemical properties. Thus, the lipid solubility and protein-binding characteristics of a local anesthetic depend on its affinity for the cell membrane of the neuron, which consists of fat (90%) and protein (10%). The higher the fat solubility of the drug, the easier it penetrates the membrane, and therefore the more effective. The better the anesthetic binds to protein, the longer its duration of action. The dissociation constant of the drug determines the rate of onset of the analgesic effect, as well as absorption and elimination.
After injection, part of the anesthetic diffuses onto the neuron membrane; the remaining drug enters the vascular bed. Increased absorption of local anesthetic equates to direct entry into the vessel; This should be especially feared in the acidic environment of the inflammatory focus. The amount of drug absorbed by the vessels depends on vascularization and the amount of blood flow in the anesthetized tissue, as well as the effect of the local anesthetic on the tone of the vascular wall. During infiltration anesthesia, amide anesthetics of medium and long action cause vasodilation, and ropivacaine (naropin), unlike other long-acting drugs (bupivacaine hydrochloride - marcaine), gives a vasoconstrictor effect. If a local anesthetic drug contains a vasoconstrictor, the rate of systemic absorption slows down, but there is a risk of developing tachycardia and atrial fibrillation.
Until recently, it was believed that the degree of systemic toxicity was strictly dependent on the concentration and amount of anesthetic administered. Thus, using lidocaine as an example (Fig. 1), peak levels of anesthetic concentrations in blood plasma were shown, which determine the possible clinical picture of a systemic toxic reaction.
Rice. 1. Dependence of the clinical manifestations of the systemic toxic reaction of lidocaine on the level of its plasma concentration.
However, according to recent publications, the described cases of systemic toxicity of local anesthetics in the practice of general and maxillofacial surgery have suggested that the manifestation of toxic reactions does not always depend on the excessive amount of administered anesthetic; even the doses of drugs recommended for use can cause this complication [6, 16, 18].
Clinically, the systemic toxic effect of local anesthetics is more often manifested by symptoms of central nervous system damage and less often by cardiovascular damage. Due to the variety of conditions that determine the timing and rate of entry of the local anesthetic drug into the vascular bed, the period of development of clinical symptoms of systemic toxicity varies within a fairly wide range - from 1-5 to >60 minutes [10].
Based on the severity of clinical symptoms, systemic toxicity of local anesthetics is divided into 3 degrees [2]. If its degree is mild (minor toxic reactions), the patient’s first complaints are tingling and itching in the area where the anesthetic was administered; these sensations may spread to the lips and tongue. At the same time, tinnitus and a metallic taste in the mouth appear. Breathing and hemodynamics are not impaired, moderate tachycardia may be observed. Since the patient's consciousness is preserved, changes in well-being, as a rule, do not go unnoticed; they cause the patient a certain anxiety, which increases as the symptoms intensify; a feeling of fear is often added. The clinical picture of the development of a toxic reaction may be limited to this; gradually the unpleasant sensations disappear without additional therapeutic measures, and the patient calms down. Most often, mild complications of local anesthesia go unnoticed by the doctor and are not recorded in the medical history. But if the patient’s subjective sensations are accompanied by trembling, twitching of individual muscles, nausea, possibly vomiting, and signs of impaired consciousness, in particular orientation, are noted, it should be understood that the toxic reaction develops and becomes moderately severe. With the maximum severity of clinical manifestations at this stage, the patient’s consciousness becomes confused, speech is impaired, numbness and retardation are characteristic, rapid breathing, decreased blood pressure, bradycardia, motor agitation or convulsions are noted. The appearance of seizures indicates that the systemic toxic reaction is becoming severe. Against the background of convulsions, loss of consciousness, decreased muscle tone, respiratory failure up to apnea, arrhythmias, asystole, relaxation and paralysis of the sphincters can occur. Without providing emergency care to patients in critical condition, including resuscitation measures with mandatory specific elements, death is inevitable.
A systemic toxic reaction to local anesthetics is not necessarily clinically manifested by all of the listed signs; some of them are often observed. An analysis of 93 cases of systemic toxicity of local anesthetics showed that the classic clinical picture developed in only 60% of victims; the predominance of pathological signs of the central nervous system with cardiovascular disorders is observed in 30.3% of cases, and only isolated cardiovascular disorders are described in 9.7% of patients [10].
The frequency of clinical signs indicating the development of a systemic toxic reaction following accidental intravascular administration of a local anesthetic is presented in Fig. 2.
Rice. 2. Frequency of development of clinical signs of toxic effects of local anesthetics [7].
Due to the complexity of conducting studies (it is impossible to perform them on humans!), the mechanism of development of systemic toxicity remains unclear. Today it is known that local anesthetics inhibit the process of oxidative phosphorylation, so the most severe disorders occur in the organs that are least adapted to anaerobic respiration metabolism, and this is primarily the brain and heart [2].
It is believed that the toxic effect on brain cells determines the ability of a local anesthetic to penetrate the blood-brain barrier and block sodium channels of excitable cell membranes, which causes toxic reactions of varying severity. If a convulsive syndrome occurs, the accompanying metabolic acidosis increases the uptake of the drug not only by brain neurons, but also by cardiomyocytes.
Cardiotoxicity is probably primarily determined by the ability of local anesthetics to reversibly bind to the intracellular part of the voltage-gated sodium channels of the cardiomyocyte, preventing them from opening and thereby preventing the generation of an action potential and its propagation along the nerve fiber. And the higher this ability of the anesthetic, the stronger its analgesic effect, but at the same time, the inhibitory effect on the conduction system of the heart [8].
All local anesthetics in high concentrations increase the refractory period of the heart, inhibit the excitability, contractility and conductivity of the myocardium - which means that in doses exceeding permissible concentrations, any of the local anesthetic drugs can cause severe depression of the myocardium. It is important to note that the clinical picture of systemic toxicity caused by lidocaine is manifested primarily by severe pathological reactions from the central nervous system; this allows the doctor to take the necessary measures to save the patient in time. And drugs that are more powerful than lidocaine, even in what is considered an acceptable plasma concentration, can, without causing convulsive manifestations or reducing myocardial contractility, provoke arrhythmias of varying severity [8].
Particular care when performing local anesthesia is required in patients with risk factors for systemic toxicity; these include anemia; hypoproteinemia; chronic heart failure with congestion; impaired liver and kidney function; endocrine and metabolic diseases; pregnancy; old age and young age (children). Compared with adults, young children have a significantly higher ratio of cardiac output and regional blood flow to body weight, and systemic toxic reactions develop more quickly in children due to the rapid increase in peak toxic drug concentrations in plasma. Thus, in a 3-year-old child after topical anesthesia, almost instantaneous absorption of the local anesthetic occurs, and the time for the onset of peak plasma concentration of lidocaine during infiltration anesthesia is comparable to that during its intravenous administration.
Special attention should be paid to the treatment of patients under sedation and general anesthesia using local anesthetics. The literature [10] describes 2 cases of systemic toxicity in infants 6 and 9 months old during uranoplasty under general anesthesia a few minutes after infiltration of local anesthetic (in one case, lidocaine, in the other, articaine). The emerging convulsive syndrome left no doubt about the diagnosis, and assistance was provided in a timely manner. Upon completion of postoperative rehabilitation, patients were discharged from the hospital without neurological deficit. Analysis of other episodes of systemic toxicity occurring during general anesthesia shows that signs of cardiovascular complications are more common because the central nervous system is blocked and early symptoms go unnoticed.
Prevention of toxic effects of local anesthetics
A systemic toxic reaction can be anticipated in cases of planned treatment of patients at risk, when the recommended dose of anesthetics is exceeded, or in non-compliance with anesthesia techniques. But, unfortunately, there is no guaranteed option to prevent this complication [15].
Prevention of systemic toxicity consists of strict adherence to instructions for the use of local anesthetics, correct execution of anesthesia techniques and careful attention to the patient both at the stage of preparation for treatment and during it.
During the initial consultation, be sure to find out complete information about the patient’s health. If you have concomitant somatic diseases, obtain an extract from the medical history indicating the diagnosis and the basic therapy recommended for use. If necessary, conduct additional examination. Before treatment, be sure to determine the patient’s physical condition and record the main parameters (blood pressure, heart rate, respiratory rate) in the medical history. Be sure to inform the patient about the possible risks and obtain his written consent for all planned interventions [3].
When choosing a local anesthetic drug, be sure to choose the least toxic of them, if the situation allows it. The use of long-acting local anesthetics is justified for long-term interventions that require prolonged postoperative pain relief, and only if a full set of resuscitation equipment is available.
Be sure to use the minimum effective dose of local anesthetic, choose a sufficient concentration and do not exceed the required volume of anesthetic. Consider the absorption capacity of the surrounding tissues at the injection site [4].
Before administering the anesthetic, be sure to perform an aspiration test and repeat it if you move the needle along the injection; Do not forget that the results of the aspiration test are false negative in approximately 2% of cases. To increase safety, use ultrasound guidance during injection whenever possible, although its effectiveness has not yet been studied and the risk of intravascular injection of anesthetic remains [5].
Be sure to inject the local anesthetic gradually, slowly (1 ml/min) or fractionally with pauses of 15-30 s. When introducing large portions of anesthetic, the injection interval must be increased to reduce accumulation [4].
Do not interrupt verbal contact with the patient during local anesthesia; be sure to monitor his reaction during manipulation and actively identify complaints - this increases the likelihood that the first subjective signs of a developing systemic toxic reaction will be noticed by you on time [3].
Below are the maximum permissible doses of local anesthetics most used in outpatient dental practice for children and adults (Tables 2-5).
Table 2. Maximum permissible doses of lidocaine 2%
Table 3. Maximum permissible doses of mepivacaine 2%
Table 4. Maximum permissible doses of articaine 4%
Table 5. Maximum permissible doses of mepivacaine 3%
Therapeutic measures for systemic toxic reactions
Until recently, the treatment of systemic toxic disorders caused by local anesthetics included the use of anticonvulsants, ensuring adequate oxygenation of the patient up to tracheal intubation followed by artificial ventilation, infusion therapy with large volumes of blood substitutes with the introduction of glucocorticosteroids and drugs that correct cardiovascular disorders. Carrying out cardiopulmonary-cerebral resuscitation, if necessary, did not include any special features; the complex was performed according to the general protocol [1].
Currently, along with measures to replace the patient’s vital functions, the priority in the treatment of systemic toxicity is to reduce and, if possible, eliminate the systemic effect of local anesthetics [13]. The recommended intravenous administration of lipid solutions, the effectiveness of which has been proven experimentally and clinically [9], allows the symptoms of toxicity to be relieved by binding lipophilic local anesthetics. The plasma concentration of drugs decreases, they are “washed out” (detached along the concentration gradient from the membrane of the neuron and cardiomyocyte) and removed with new portions of lipid. In addition, it is known that lipid-containing solutions are an energy substrate for cardiac mitochondria and this ability is in demand in the case of cardiotoxic reactions. The treatment regimen using Intralipid solution (20%) to eliminate systemic toxic reactions of local anesthetics was called “lipid rescue” [7].
The clinical picture of the severe stage of systemic toxicity of local anesthetics can develop rapidly, so it is very important to correctly assess the first symptoms and begin emergency care in a timely manner. Seizure syndrome remains an absolute indication for the use of benzodiazepines; it is more dangerous to treat it with propofol or ultra-short-acting barbiturates due to their own pronounced cardiodepressive effect. As in previous recommendations, one of the first measures to save the patient is to ensure adequate oxygenation by any available means, including tracheal intubation and mechanical ventilation with 100% oxygen. In case of ineffective blood circulation due to arrhythmia or asystole, resuscitation measures should be started immediately and continued for at least 60 minutes. Since local anesthetics do not cause irreversible changes in the myocardium, with sufficient oxygenation of the brain and the administration of lipid solutions during this time, there is hope for saving the patient. It is extremely important not to rush to stop effective resuscitation measures if systemic toxicity is caused by powerful anesthetics, because they take a long time to “wash out” [6]. When carrying out symptomatic therapy, if necessary, it is necessary to avoid the administration of lipophilic drugs - beta-blockers and calcium channel blockers, abandon vasopressin, use only amiodarone (cordarone) to relieve ventricular arrhythmias, reduce the dosage of epinephrine (adrenaline) to less than 0.1 mcg/day. kg or completely abandon its administration [13].
Literature sources [20] report that in case of a systemic toxic reaction to local anesthetics, rapid administration of large volumes of lipid solutions is not accompanied by significant complications, and their clinical effectiveness against the background of resuscitation measures allows one to avoid residual cardiac disorders and neurological deficits [10, 17].
For “lipid leaching,” any fat emulsion can be used, but Intralipid (20%) has proven itself to be the best [11]. Inactivation of local anesthetics with diprivan (propofol) should not be carried out due to the need for a large amount of the drug to obtain a positive result due to its low lipid content, and this is dangerous since diprivan has a direct cardiodepressive effect [15]. Today, it is recommended to relieve a systemic toxic reaction to local anesthetics with lipids, starting the administration of the drug when the first characteristic complaints or symptoms appear and at the same time being ready to perform a full range of resuscitation measures [6].
In each medical institution, including dental, where local anesthetics are used, it is necessary to have 1 liter of fat emulsion solution (Intralipid 20% - 500 ml or other), syringes for “lipid washing out” with a volume of 50 ml, peripheral intravenous catheters 14-16 G, Infusion systems, copy of the Lipid Rescue protocol [19].
After catheterization of the peripheral vein, the lipid solution must be administered as a bolus (Intralipid 20% - 1.5 ml/kg) using 50 ml syringes, then switch to drip infusion (Intralipid 20%, rate - 0.25 ml/kg/min) and Continue administering the drug at this pace for at least 10 minutes after blood circulation has stabilized. If it is not possible to stabilize blood circulation with this dose of lipid solution, it is necessary to repeat its bolus administration in the same dosage (Intralipid 20% - 1.5 ml/kg) and switch to an accelerated infusion of the drug (Intralipid 20%, rate - 0.5 ml/kg /min). The highest single dose of fat emulsion is acceptable - 10 ml/kg/min.
At the Euroanaesthesia 2010 forum in Helsinki (Finland), the European Board of Anesthesiology, together with the European Society of Anaesthesiology, adopted a declaration on patient safety in anesthesiology. It provides fundamental points that make it possible to prevent and avoid serious complications and prevent danger to patients. In particular, it is stated that all medical institutions that use local anesthetics “... must have protocols and facilities necessary in situations of systemic toxicity...” [14]. The Declaration of Helsinki has been endorsed by the World Health Organization, the World Federation of Societies of Anaesthesiologists and the European Patients Federation. Taking into account its specifics, each country has the right to refine and adapt the protocol for resuscitation using lipid solutions to its own conditions. We consider this task extremely important for our medical community.
The authors declare no conflict of interest.
Bumecaine
Synonyms: pyromecaine. Indications for use
Pyromecaine is used for superficial anesthesia for stomatitis, gingivitis, glossitis, pulpitis, to anesthetize the injection site and relieve an increased gag reflex. Method of administration and dosage Pyromecaine in dentistry is used only for superficial anesthesia: in the form of a 1% solution to suppress the gag reflex when taking impressions; A 1-2% solution and 5% pyromecaine ointment are used to anesthetize the mucous membranes. An ointment containing 5% pyromecaine and 5% methyluracil, which has an anti-inflammatory effect and stimulates regeneration processes, has been developed for dental practice. When treating inflammatory diseases of the oral cavity, the ointment can be used 1-3 times a day. The dose of ointment should not exceed 1 g.