Human health is a very fragile and unpredictable thing, and diseases often appear out of nowhere. This also applies to oral diseases. If you are faced with such an unpleasant problem as a sore in the mouth, then you would probably like to know how to get rid of it.
The appearance of wounds on the human oral mucosa is usually accompanied by pain and causes discomfort while eating or talking. But many people, despite these symptoms, choose not to seek help from a doctor. Some people simply ignore the problem, while others try to self-treat the disease at home. Both of these approaches give positive results only in rare cases.
The presence of any wounds and damage covering the palate indicates health problems in an adult or child. This situation should not be left to chance; you should seek help from a dentist. Only he will be able to diagnose the disease and prescribe appropriate treatment. If you are concerned about wounds in your mouth, then you can contact the LeaderStom network of dental clinics to solve this problem. We will help you cope with the situation and will make every effort to quickly cure the disease.
— 15% on the first visit
Causes of childhood stomatitis
There are 6 main factors that can provoke the occurrence of stomatitis in the mouth in infants:
- infections;
- mechanical damage;
- physical agents;
- chemical burns;
- allergic reactions;
- poor oral hygiene.
All conditions that cause immunodeficiency in a child predispose to the occurrence of such a pathology: chronic diseases of internal organs, vitamin deficiencies, the presence of foci of chronic infection in the body, stress, climate change. Dr. Komarovsky notes an increase in the incidence of stomatitis in children who often suffer from ARVI.
Infectious forms of the disease are the most widespread. Most often, herpetic stomatitis occurs. Also, lesions of the mucous membranes of the oral cavity can appear against the background of various infections: smallpox, measles, rubella, entero- and adenoviruses. Banal staphylococci and streptococci, which normally live in small quantities in the mouth of every baby, also play a huge role in the development of the inflammatory process. Their effect increases only when the child’s immunological status decreases.
Quite often, after taking antibiotics (especially if the course of treatment is long), infants develop a fungal infection of the oral mucosa - candidiasis or thrush, which can also trigger the development of stomatitis.
Children, especially young children, learn about the world around them through taste. Therefore, babies constantly put into their mouths all the objects that are at their disposal. Thus, mechanical trauma to the mucous membranes simply cannot be avoided. And take into account the fact that objects are not always clean, inflammation forms very quickly. A child can independently injure the mucous membrane by biting it with his teeth. This is observed very often in dreams with neuroses.
When teething, gums are sometimes injured, which, coupled with the baby’s reduced immunity during this period, leads to a strong inflammatory response.
Of the physical agents, the most common cause of stomatitis is exposure to hot food. In this case, microburns occur on the mucous membranes, at the site of which inflammatory foci are formed.
Chemical burns occur due to accidental exposure of the oral mucosa to potent substances. In everyday life, this could be vinegar, high-concentration hydrogen peroxide, alcohol or eau de toilette, perfume, various paint solvents or liquid cleaning products.
Anything can act as an allergic component in the development of stomatitis. For example, harmless candy, toothpaste, chewing gum, various drinks, medications and food. Often, allergic stomatitis occurs in infants during the period of introducing the first complementary foods.
Sores in the mouth as a sign of aphthous stomatitis
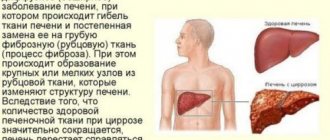
Wounds in the mouth can arise as a result of the development in a person of a separate independent disease of the oral mucosa, caused by the growth and development of pathogenic microorganisms. But, in addition, the cause of such wounds may also be hidden in the general somatic condition of an adult or child.
In most cases, mouth ulcers are symptoms of a disease such as canker sores. Stomatitis is a lesion of the human oral mucosa that occurs as a result of an atypical reaction of the immune system to foreign irritants. Depending on the nature and causes of the disease, stomatitis can be of various types: ulcerative, herpetic, allergic, vesicular, etc. But people most often have to deal with the aphthous form of this disease.
Let's name the main symptoms of aphthous stomatitis:
- The appearance of round ulcers (ulcers) in a person’s mouth, which are grayish in color and surrounded by a red, inflamed rim. Ulcers are located either separately or in groups and have different sizes.
- Painful sensations in the affected areas of the upper and lower palate of a person that occur during eating, drinking, or talking.
- Deterioration of a person’s general well-being, weakness.
- Temperature increase. But this is not a mandatory symptom; it occurs in most cases in children, since they are more difficult to tolerate aphthous stomatitis in the oral cavity.
- Enlarged submandibular lymph nodes. This symptom of aphthous stomatitis also occurs more often in children than in adults.
Symptoms and signs
How to recognize stomatitis in children? Despite the abundance of causes that cause this disease, all forms of stomatitis have common clinical symptoms:
- The first signs of such a pathology are slight redness on the mucous membranes, which can be localized both on the gums and on the palate, on the tongue or on the lip.
- Gradually, the redness gives way to swelling, round or oval ulcers appear, covered with a whitish or gray coating on top and surrounded by a red cushion. These ulcers are very painful and prevent the child from leading a normal life, eating or sleeping.
- As the inflammatory process becomes more severe, small ulcers merge into one large one.
- Local signs of stomatitis are accompanied by general symptoms: the child’s temperature rises, weakness, and lack of appetite appear.
One of the features of the course of the disease is the appearance of vomiting with stomatitis. It is caused by increased work of the salivary glands and increased excitability of the baby’s nervous system due to severe pain.
The mechanism of occurrence and symptoms of stomatitis
As noted above, the symptoms of stomatitis are ulcers that appear in the oral cavity (on the palate, in the cheeks or on the tongue), which bother a person, causing him pain. The mechanism of occurrence of such erosions is associated with the response of the human immune system to foreign irritants, which, for example, are viruses or bacteria.
Stomatitis manifests itself in such forms as herpetic, aphthous, allergic, vesicular, catarrhal, etc. In any case, the manifestations of stomatitis disease are expressed in lesions of the human oral mucosa or tongue, only depending on the variety they are of a different nature.
Types of childhood stomatitis and their main manifestations
The classification of childhood stomatitis is based both on the cause of the disease and on some distinctive features in the clinical course of such pathology. We will tell you how to determine this or that type of disease in our article later.
Catarrhal stomatitis
It is the mildest and most common form of the disease. In this case, multiple inflammatory foci appear on the mucous membrane of the gums, cheeks or lips, covered with a whitish coating, but without the formation of aphthae or ulcers. In this case, the child will complain of pain in the mouth when eating, drinking or talking, increased salivation, bad breath, and general weakness.
With catarrhal stomatitis, the mucous membrane is very susceptible to injury and bleeding, even during normal activities: brushing teeth, eating. When inflammatory foci are localized only on the gums, the clinical picture of stomatitis will resemble gingivitis.
Ulcerative stomatitis
The ulcerative form is a consequence of untreated catarrhal stomatitis. In this case, against the background of edematous foci of redness, multiple ulcerations are formed, which gradually increase in size, spread deep into the tissue of the mucous membranes or merge with each other.
The child complains of severe pain in the oral cavity, which intensifies when trying to brush his teeth or eat, and the smell of his breath becomes putrid. General health worsens: body temperature rises, weakness and body aches occur.
Young children are capricious, refuse to eat, and have trouble sleeping.
Gangrenous stomatitis
The gangrenous form of the disease is a continuation of catarrhal and ulcerative forms. A characteristic sign of this pathology is the spread of the inflammatory process deep into the tissues of the jaw with the development of extensive necrosis, which can involve the bones and spread to other anatomical areas.
The condition of a child with gangrenous stomatitis is extremely serious. There may be disturbances of consciousness, severe weakness, and the smell of rotting meat from the mouth. Regional lymph nodes are enlarged and painful on palpation.
Candidiasis (fungal or milk) stomatitis
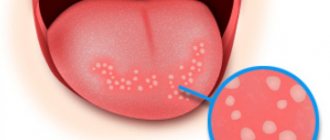
Candidal stomatitis is characterized by specific symptoms. At the onset of the disease, children have dry mouth. Subsequently, a burning sensation and an unpleasant aftertaste appear. A white coating in the form of small dots is deposited on the mucous membrane. As the process progresses, the points merge into a large lesion that resembles a curdled mass. Such plaque is difficult to remove, exposing the inflamed surface of the mucous membrane.
Fungal stomatitis often occurs without fever, and the general condition is little affected.
Infectious stomatitis
The phenomenon of stomatitis can also be observed in some infectious diseases. With scarlet fever, the typical picture on the mucous membranes of the mouth will be supplemented by specific manifestations of the disease: a pinpoint rash on the skin and a “crimson tongue” - the surface of the tongue is bright red, shiny with hypertrophied papillae.
With diphtheria, damage to the gums will be combined with the detection of dense grayish films on the tonsils or in the throat. In this case, a paroxysmal cough with episodes of suffocation will be noted.
Allergic stomatitis
The allergic form of stomatitis most often affects children over 4 years of age. It is characterized by a clear connection with the action of the allergen, a rapid increase in symptoms and their rapid extinction with adequate treatment. The clinical picture in this case is similar to the ulcerative version of the disease - ulcers or aphthae form on the mucous membranes, covered with a whitish coating and surrounded by a focus of redness. Quite often, this pathology occurs in the form of chronic stomatitis with periodic episodes of exacerbation.
Traumatic stomatitis
In cases of mechanical trauma, a significant focus of infiltration appears on the mucous membrane, which ulcerates as the inflammation progresses. When burned by hot drinks, a bubble often appears, after opening which a fairly deep ulcer is exposed. A distinctive feature of the traumatic form of the disease is a clear connection with trauma or thermal burn of the oral mucosa and the formation of a single lesion.
In case of severe inflammation, local symptoms may be accompanied by general symptoms: fever, malaise, headache.
Herpetic stomatitis
In herpetic stomatitis, the main morphological element is small blisters located against the background of a hyperemic mucous membrane. They quickly open and erosions form, which are covered with fibrous plaque. The lesions can be localized separately or merge into a single affected area.
Erosion is extremely painful, the child refuses to eat, is capricious, sleep is disturbed, and in severe cases there is a significant increase in body temperature. In this case, typical herpetic lesions can be found not only in the oral cavity, but also on the face or other parts of the body.
Bacterial (purulent) stomatitis
Most often, bacterial stomatitis appears due to constant improper oral care or microbial sore throat. The clinical picture is typical for stomatitis: initially foci of inflammation appear, which then transform into deep ulcers covered with abundant purulent plaque.
At the same time, purulent deposits on the tonsils are detected, the child’s general well-being suffers, body temperature often rises significantly, and the cervical, submandibular and clavicular groups of lymph nodes enlarge.
Vesicular stomatitis
Vesicular stomatitis is an infectious disease. Its causative agent is vesiculovirus, a virus transmitted from sick animals to people. The incubation period of this disease is 5-6 days, during which children may complain of fatigue, weakness, and slight chills. Subsequently, small painful blisters with whitish contents appear on the mucous membranes of the oral cavity. Similar elements appear in the area of the feet and hands.
The general symptoms are very similar to a banal acute respiratory infection: the body temperature rises, there may be signs of rhinitis and conjunctivitis. If the intestines are damaged, there may be dyspeptic symptoms: diarrhea or constipation.
Why does aphthous stomatitis occur?
As noted above, the causes of aphthous wounds in a person’s mouth can be both local and general somatic in nature. Let's look at the main ones.
Local causes of aphthous stomatitis:
- Mechanical damage to the human oral mucosa. Such injuries occur as a result of a person eating hard and tough foods. Often, even a small scratch on the roof of the mouth can cause aphthous stomatitis.
- Thermal lesions of the human oral mucosa. The occurrence of wounds and the development of aphthous stomatitis in this case provoke burns of the mucous membrane, which a person could receive by consuming hot drinks or food.
General somatic causes of wounds in the human oral cavity:
- Heredity factors. The predisposition to the occurrence of aphthous stomatitis in the mouth may be determined by genetic reasons. Therefore, there is a risk of developing this disease and the manifestation of a chronic form of stomatitis (when ulcers on the mucous membrane appear regularly) in people whose parents also suffered from this disease.
- Somatic diseases. Aphthous stomatitis often develops in people who suffer from any secondary somatic diseases. For example, these could be diseases of the digestive system and gastrointestinal tract.
- Weak immunity. For this reason, children are susceptible to oral ulcers because their immunity is not yet fully developed. In a child, aphthous stomatitis is more severe than in an adult and is accompanied by an increase in temperature and a deterioration in general well-being. Against the background of colds, immunity is also often reduced, and aphthous stomatitis occurs in the person’s mouth.
- Avitaminosis. With an incorrect diet, a person does not receive enough substances necessary for the successful functioning of the body. Due to a lack of vitamins C and B or microelements such as selenium, folic acid, zinc or iron, in some cases aphthous stomatitis occurs in a person’s mouth.
- Allergy. An allergic reaction associated with eating foods such as citrus fruits, nuts (especially peanuts), chocolate, red berries (strawberries, wild strawberries) or foods containing gluten (cereals, pasta) in some cases leads to the appearance of canker sores. wound in a person's mouth.
- Stress. When a person finds himself in a stressful situation, he spends significant resources to cope with the current problem. This leads to a loss of strength, decreased immunity and a general weakening of the body, as a result of which wounds form in the person’s mouth and he develops aphthous stomatitis.
Nutritional Features
Due to the fact that painful ulcers appear in the mouth with stomatitis, any meal gives the baby discomfort. Therefore, the diet during the period before recovery should have a number of features.
- All food taken should be warm and at a temperature as close as possible to body temperature. This will prevent unnecessary irritation and will not cause acute pain.
- Since chewing is quite painful, portions should be reduced by about a third, but the frequency of meals should be increased.
- When feeding your baby, you should give preference to dishes with a soft consistency, and it is better to postpone dense and dry foods until complete recovery.
- It is worth giving preference to products with a neutral taste. These are potatoes, bananas, pears, pumpkin.
- Until recovery, spicy, salty and sour foods are completely excluded from the child’s diet.
- To make eating less painful, you can purchase thick straws for cocktails and crush all food so that it can be drunk.
- The emphasis is on healthy foods rich in microelements and vitamins. For example, buckwheat, oatmeal, and rice can be recommended for cereals. It is preferable to give your baby cauliflower and broccoli as vegetables.
Is stomatitis contagious?
Infectious variants of the disease are quite easily transmitted from sick children to healthy ones. Most often, the infection spreads through airborne droplets from saliva during normal talking, coughing or sneezing.
The herpes virus can pass from an infected mother to the child during childbirth or during breastfeeding in the event of an exacerbation of herpetic inflammation.
We must remember that some forms of infectious stomatitis may well be transmitted through shared objects. This is especially true for cutlery, toys and personal care products. Therefore, if a child gets stomatitis, it is necessary to take measures aimed at preventing the possibility of its transmission to healthy children.
- If there is another child in the family, then it is worth protecting him from communication with the sick baby for at least a few days.
- It is imperative to provide the patient with individual household items that can be processed separately from the belongings of the rest of the family.
- If a case of stomatitis is detected in a kindergarten, it is recommended to disinfect all toys that healthy children may come into contact with.
Treatment of sores on the tongue
After determining the type and provoking factor of the disease, treatment is prescribed. Therapeutic dentistry is aimed at combating the damage itself, as well as the disorders that occur in the patient’s body. The course of treatment involves the prescription of medications and traditional healers. To increase the body's defenses, it is recommended to take vitamin complexes that include vitamins B and C. It is important to follow a diet that excludes hot, sour, salty, and spicy foods. A fungal infection does not allow the consumption of dairy and sweets. Therapy consists of the following stages:
- Healing, in which tissue is locally affected to eliminate pain, remove necrotic layers, and stimulate regeneration. It is necessary to treat caries, restore damaged fillings, correct bites, and grind the sharp edges of crowns.
- Antimicrobial therapy eliminates the provoking factors of the disease. Prescribed drugs against fungi, viruses, antihistamines and antibacterial drugs, rinses, applications, laser therapy, phonophoresis.
- General measures eliminate diseases of internal organs. They can be carried out in infectious diseases, pulmonology and other departments.
Drug therapy
Ulcerative formations require the following treatment:
- Pain is eliminated with the help of analgesics, which have a positive effect on inflamed tissue. These are Metrogyl Denta, Asepta-gel, Cholisal.
- If the disease is of an allergic nature, therapy includes taking antihistamines: Suprastin, Fenkarol, Tavegil.
- Bacterial lesions, when ulcerations are localized at the tip of the tongue, on the sides, at the root, require antiseptic substances: Miramistin, Chlogexidine.
- Gels for viral infections are prescribed in cases of herpes-related disease. This is Acyclovir, Oxolin.
- For aphthous stomatitis, sulfonamides and corticosteroids are prescribed.
Folk remedies
Quick treatment at home involves supplementing drug therapy with traditional medicine recipes. A solution made from the juices of Kalanchoe and aloe has high therapeutic effectiveness. It is used for rinsing. Plants relieve inflammation, heal damage, and eliminate abscesses. Decoctions of cinquefoil, St. John's wort, calendula, and chamomile are useful. Plants are antiseptic. Treatment should continue for 7-10 days. A solution based on hydrogen peroxide and water will disinfect and relieve pain.
An application of grated raw potatoes wrapped in gauze will remove the burning sensation. Local immunity will increase if you use freshly squeezed carrot juice, which should be diluted by half with water. Rinse the mouth with this solution at least 3 times a day.
How many days do people suffer from stomatitis and what to do at the first signs of it?
How long does stomatitis last? This question is of great concern to parents of sick children, since all the symptoms of the disease are unpleasant and cause discomfort to the child.
The duration of the disease depends on its form. Acute variants of stomatitis with adequate drug treatment resolve within 14 days.
If the disease does not go away for a month or more, then they talk about the chronic course of such a pathology. In this case, it is possible to alternate periods of subsidence of clinical symptoms and their exacerbation - recurrent stomatitis.
If you suspect signs of stomatitis in your child, you should urgently consult a doctor who will tell you how to numb the mucous membrane and prescribe comprehensive treatment. If it is not possible to visit a doctor as soon as the first symptoms of the disease begin, then it is possible to independently numb the mouth with local drugs (Dentinox, Kalgel). And you can’t delay medical consultation!
Diagnostics
To make a correct diagnosis, patients must undergo modern diagnostic methods in dentistry. In addition, the doctor interviews the patient and examines the oral cavity. Research includes:
- Staining with special dyes allows you to clearly visualize the damage.
- Laboratory tests of cytological type.
- Histological studies of cells.
- Biochemical tests.
- Immunological and microbiological examinations.
- Diagnosis of allergies.
If the situation is complex, the patient may be referred to other specialists for consultation. The dentist will determine the stage of the disease, find out its causes and nature, and draw up a symptomatic picture. If necessary, the patient is examined by a pulmonologist and a neurologist. After their consultation, the list of instrumental and laboratory activities can be supplemented.
Possible complications
The prognosis for the disease is usually favorable. However, incorrect or untimely treatment can lead to the development of complications:
- The addition of a secondary bacterial infection, accompanied by a worsening of the sick child’s condition.
- Sometimes severe necrotizing forms of stomatitis lead to osteomyelitis - destruction of the bone tissue of the jaw.
- Persistent or frequent stomatitis can provoke the loss of teeth from both the primary and permanent sets.
- The presence of a chronic purulent inflammatory focus in a child’s body negatively affects the state of immunity, and also, under the influence of unfavorable factors, can lead to blood poisoning - sepsis.
How to cure stomatitis on the tongue?
At the first signs of stomatitis, specialists at the LeaderStom clinic recommend contacting a dentist for diagnosis and prescribing appropriate treatment. A person’s attempt to cope with a stomatitis disease that appears on the tongue on his own may not only not lead to the desired result, but on the contrary, increase the symptoms of the disease. The drugs that are used to treat stomatitis on the tongue can be divided into local therapy drugs and medicinal formulations that have a general effect on the human body. Let's take a closer look at each of these forms.
Treatment of stomatitis with local therapy:
- Treatment of stomatitis ulcers on the human tongue with antiseptic gels, ointments and sprays.
- Rinsing the mouth with antiseptic solutions, which can be purchased at the pharmacy (chlorhexidine, miramistin, etc.) or prepared yourself using medicinal herbs such as chamomile or calendula.
- In order to relieve the pain symptom, doctors recommend using local preparations containing lidocaine for a person with stomatitis formations on the tongue.
General therapy for stomatitis:
Depending on the cause that provoked the stomatitis disease, antibacterial, antiviral, antifungal or antihistamines are used. Such drugs are prescribed to a person only by a dentist or therapist. To relieve the symptoms of stomatitis, modern antipyretic and painkillers are used.
Taking vitamin complexes allows you to compensate for the lack of essential microelements in the body, which for one reason or another a person does not receive with food, and vitamin deficiency, as is known, is one of the factors that can provoke stomatitis on the oral mucosa and tongue.
For stomatitis, immunomodulatory drugs are also used - drugs that increase human immunity. They can be of both plant and medicinal origin. All patients, regardless of the reasons that caused stomatitis on the tongue, are recommended by doctors to take these medications.
Drugs are also used to treat somatic diseases. The use of such remedies is necessary if the cause of stomatitis on the tongue lies inside the body. Chronic diseases of certain systems, and especially the human gastrointestinal tract, weaken the body and contribute to the launch of an immune reaction, manifested in the formation of stomatitis ulcers on the palate and tongue.
Prevention in infants
Preventive measures should begin in a newborn child immediately after he is discharged from the maternity hospital. For the first days and months of life, it is necessary to adhere to thorough disinfection of toys, bottles during artificial feeding, or to treat the nipples immediately before applying to the breast.
«
An important point is regular visits to the dentist from the first teeth. It is necessary to carefully care for your baby’s oral cavity and use only special toothbrushes and toothpastes, preferably those recommended by the doctor.
Pain and burning of the tongue: how to treat?
Probably every gastroenterologist in his practice has encountered a patient with complaints of pain or burning of the tongue. Turning to this specialist in the first place is probably due to the following logical chain: the tongue is in the oral cavity, where the digestion process begins, which means that if a problem arises, you should visit a gastroenterologist. Old publications also come to the aid of patients and doctors of other specialties, in which chronic diseases of the digestive organs were considered as the causes of burning tongue.
But is it really that simple? Is pain and burning of the tongue a separate disease and who should treat it?
A little history and terminology.
Pain/burning in the tongue has many synonyms: glossalgia, glossodynia, stomatodynia, glossopyrosis, oral paresthesia, neurogenic glossitis, tongue neurosis, glossalgic syndrome. This condition is traditionally part of the so-called burning mouth syndrome or “burnt mouth syndrome,” in which pain/burning sensations are localized in various areas: tongue, upper palate, gums, lower lip, pharynx.
Burnt mouth syndrome (SMS) was first described back in 1880; in the 20th century, the term glossodynia, i.e., appeared. pain in the tongue, since unpleasant symptoms from the tongue were most common. This syndrome was first identified as a separate disease in 2004.
Almost all existing review articles and recommendations consider glossodynia within the framework of the SOP. General recommendations for the diagnosis and treatment of ROP may be applicable to the special case of glossodynia.
Definition
The International Association for the Study of Pain has designated glossodynia and oral burning as chronic pain, specifically “burning pain of the tongue or other mucous membranes of the mouth.”
Later, a detailed definition was given for ORS: “a burning sensation or sensation of altered sensitivity in the oral cavity, repeated daily for more than 2 hours a day for more than 3 months, without obvious causative lesions on clinical examination and examination.”
Epidemiology
Data on the prevalence of ROP and tongue pain/burning separately still vary from study to study. The average incidence of all cases of oral burning (including but not limited to tongue burning) is 0.1-3.7% of the population. Women suffer from this syndrome 2.5-7 times more often than men, especially often over the age of 60 and after menopause.
Common causes of pain and burning in the mouth.
There are two groups of reasons why patients notice a burning sensation in the mouth:
1) Primary (idiopathic), when there are no diseases of the oral cavity and other organs and systems, this will be the true SOR.
2) Secondary, caused by local (localized in the oral cavity) and systemic causes (autoimmune diseases, deficiency conditions, etc.)
Causes of secondary burning sensation in the mouth/burning tongue.
Possible causes of secondary burning sensation in the oral cavity are diverse and, oddly enough, are rarely associated with pathology of the digestive organs. A review published in 2022 on this problem identified the following conditions and diseases responsible for the occurrence of burning sensation in the mouth:
Local factors:
A. Diseases, conditions and damage to the oral cavity:
- fungal infection (eg candidiasis)
- lichen planus
- pemphigoid
- pemphigus
B. Trauma
1) Mechanical
2) Chemical
A. From the patient's side:
- toothpastes with abrasives
- use of mouth rinses with ethyl alcohol
- medications such as aspirin (applied to the sore tooth); over-the-counter medications containing phenols, peroxide, sulfuric acid
- vitamin C (citrus fruits)
- sour drinks
- lozenges and cough suppressants with high menthol content
b. From the dentist:
- Irrigation of the oral cavity with solutions containing methyl methacrylate, formaldehyde, formocresol, sodium hypochloride
- acrylic resin
- eugenol
3) Thermal: spicy or hot food or drink
C. Parafunctional habits
- Tongue sticking out, cheek biting, excessive tongue brushing
- mouth breathing
D. Xerostomia or impaired quality/quantity of saliva
- consequences of radiation or chemotherapy, Sjogren's syndrome, pathology of the salivary glands
- side effects of medications (antihistamines, antidepressants, diuretics, steroid hormones, non-steroidal anti-inflammatory drugs, amphetamines)
- smoking
E. Allergic reaction/contact hypersensitivity
- products, additives, flavors
- colorings and flavors from oral care products
- dental materials (nickel sulfate, cobalt, zinc)
System factors
A. Deficiency conditions: decreased levels of iron, zinc, folic acid, vitamins B1, B2, B6, B12
B. Endocrine pathology
- diabetes
- hypothyroidism
- hormonal disorders (changes in cortisol/sex hormone levels)
C. Autoimmune diseases
- Sjögren's syndrome
- lichenoid reactions
- systemic lupus erythematosus
D. Other diseases
- gastroesophageal reflux disease
- celiac disease
- multiple sclerosis
- Parkinson's disease
- Fabry disease
E. Medicines
- angiotensin-converting factor inhibitors
- antiretroviral therapy
F. Peripheral and central neuropathies
- diabetic polyneuropathy, neuropathy due to renal failure, neuropathy due to systemic connective tissue diseases, neuropathy due to HIV infection, postherpetic neuropathy, neuropathy due to chemotherapy
As can be seen from this huge list, most cases of burning of the tongue and in the oral cavity in general are caused by a dental problem/pathology, neurological, endocrine and autoimmune diseases. Gastroenterological causes (for example, gastroesophageal reflux disease) are rather the exception to the rule.
Primary burning sensation in the oral cavity (BOR) and its causes.
If there are no indications of secondary causes of burning in the oral cavity, most likely there is a true SOR. This is an independent disease, the cause of which is still unclear. In its development, the role of psychological factors and mental disorders, changes in the nerve endings and conductive nerve fibers of the oral cavity, as well as the central nervous system is assumed.
Clinical manifestations of ROP.
Symptoms that may bother patients with ROP are:
1) Pain and/or burning in the mouth of varying intensity. Some patients describe these sensations as tingling or irritation, as well as impaired sensitivity. The pain often occurs spontaneously, is often symmetrical and does not necessarily affect only one area. In the case of glossodynia, pain/burning is most often localized in the anterior 2/3 of the tongue, on its back, and lateral surfaces. The pain is minimal in the morning immediately after waking up, increasing in intensity throughout the day. Eating spicy, hot foods and drinks, as well as stress and fatigue increase the pain/burning sensation.
2) More than 70% of patients, in addition to pain/burning, note changes in taste, a decrease in its intensity, as well as the appearance of a foreign taste (bitter, metallic, or a combination of both). Most often, the sensation of sweet and salty tastes is reduced, and sour tastes are perceived more intensely.
3) Dry mouth (xerostomia) is noted by 46-67% of patients with SOP, while according to research data, an objective decrease in the amount of saliva is not observed in them.
4) Association with burning/pain from other mucous membranes has also been described in patients suffering from ROP. Most often this is a burning sensation in the rectum and genital tract. An alternative may be a feeling of dry mucous membranes (eyes, genital tract in women)
5) Night sleep disturbances are common (in 80% of cases) in people with SRS
6) Anxiety and depression are frequent companions of SOR and glossodynia separately. A meta-analysis of clinical studies showed that anxiety conditions increase the risk of developing RAS by 2.6 times, and depression by 3.2 times. Cancerophobia, social phobia, neuroticism, etc. are also often noted.
7) ODS is characterized by an association with other diseases that manifest as chronic pain: fibromyalgia, chronic back pain, chronic pelvic pain, irritable bowel syndrome, etc.
Treatment of SOR.
1) Patient information and support
Many patients with chronic oral burning and pain do not understand why their symptoms persist for so long. An important task of the doctor is to explain to patients with SRS the possible mechanisms of the formation of unpleasant sensations. Patients should be reassured that their symptoms are not imaginary or related to any form of cancer. This support will reduce anxiety, depression, fear and frustration, especially in individuals who have had previous unsuccessful treatment experiences.
2) Local therapy
Local use of clonazepam in the form of mouth rinses showed good results in reducing the severity of pain/burning in the mouth. There is encouraging evidence for the topical use of capsaicin (a chili pepper alkaloid) in low concentrations.
3) Systemic therapy
Tricyclic antidepressants, antidepressants from the group of serotonin and serotonin/norepinephrine reuptake inhibitors, clonazepam, and antiepileptic drugs (pregabalin and gabapentin) are actively used as drugs for the treatment of ORA. The use of alpha-lipoic acid has shown little effectiveness.
4) Non-drug psychotherapy
Given the frequent association of ODS with anxiety disorders, phobias and depression, non-pharmacological psychotherapy is an integral part of the treatment of this problem. Cognitive behavioral therapy, individual and group psychotherapy should be considered as methods of choice.
5) Physiotherapy and alternative treatments
Low-level laser therapy and acupuncture have been studied as methods for reducing pain. These methods were effective in some people with cerebral obstruction, but are not widely used.
Conclusion.
Identifying the causes of pain/burning in the oral cavity is a challenge for doctors of different specialties, but their friendly work allows us to solve the problem and improve the quality of life of patients.