Every caring mother can share her experience of worrying about children’s illnesses, especially if it concerns infants.
There is definitely no need to panic when identifying signs of disease; precious time is wasted. What to do if ulcers are detected on the tongue and which specialist to contact will be discussed in the article.
What is this disease?
Herpetic stomatitis is a pathological process that develops in the mucous membrane lining the oral cavity. The causative agent of this disease is herpes simplex virus type 1. In children under the age of five, this virus is detected in 60% of all cases. By adolescence, it is detected in the vast majority of people. Herpes stomatitis in children develops during the baby’s first contact with the virus. This occurs most often before the age of three.
The high incidence is explained by:
- low level of production of own antibodies;
- immaturity of cellular immunity;
- the fact that the baby does not receive antibodies from mother's milk;
- high reactivity of the child's body.
If the baby is bottle-fed, he may get sick in the first months of life. Viral infection often goes into a latent state. It persists in the nerve ganglia.
Causes
The cause of the development of the pathology is the herpes simplex virus type 1. It belongs to DNA viruses belonging to the Herpesviridae viral family. The pathogen multiplies rapidly in the epithelial cells of the oral mucosa. Then it enters nearby lymph nodes (submandibular) and continues to reproduce in them. Then it enters the blood and migrates to the parenchymal organs (spleen, liver, kidneys). There it multiplies and enters the bloodstream again. As a result, it again appears in large quantities in the epithelial cells of the skin and mucous membranes. They are massively defeated. It is localized in the oropharynx, oral cavity, nose, lips, and nearby skin. Stomatitis and herpes of the skin and mucous membranes develop when the infection generalizes simultaneously.
Children become infected with it as follows:
- through contact and everyday life (using shared utensils, toys, through kissing);
- airborne (coughing, sneezing);
- from a sick mother to the fetus through the placenta or during childbirth.
A baby can become infected from sick adults, children, and carriers.
The following factors contribute to the development of the disease:
- previously suffered inflammatory processes;
- previous antibiotic therapy;
- deficiency of microelements and vitamins in the body;
- mechanical damage to the skin and mucous membranes;
- insufficient fluid intake;
- poor oral hygiene.
In children, the virus is especially easily transmitted through contact. The infectious process quickly spreads to healthy areas.
Associated symptoms and what they indicate
Diagnosis of the disease is carried out taking into account the accompanying symptoms.
- Small sores on the tongue and lips may indicate a viral infection - herpes
Temperature indicates an inflammatory process. This is typical for candidiasis, herpes, allergies, and aphthous stomatitis.
- Ulcers located under the tongue appear due to injury, candidiasis, and somatic diseases.
- On the tip of the tongue, sores most often form due to mechanical damage to tissue.
- Accompanied by plaque ulcers due to candidiasis and problems with the gastrointestinal tract.
- Small sores on the tongue and lips may indicate a viral infection - herpes. Thrush ulcers often spread to the lips.
- On the tongue and throat, ulcers are formed as a result of mechanical trauma, malocclusion, dehydration, vitamin deficiency, and the use of medications with a high concentration of active substances.
- Ulcers in a baby indicate possible problems with the internal systems of the body. May indicate an allergic reaction, vitamin deficiency, mechanical damage to the tongue, fungal or viral infection.
Classification
According to the flow, acute, chronic, and wave-like variants of the pathology are distinguished. The following degrees of severity of the pathological process are distinguished:
- Mild - it is typically characterized by a slight increase in body temperature, moderate inflammation of the mucous membrane in the mouth, and enlargement of regional lymph nodes. Rashes form on the mucous membrane and skin.
- Medium – high temperature rises. Severe weakness and sudden deterioration in health. The baby begins to vomit and the pain in the mouth increases. Significant rashes appear in the mouth and the skin around it.
- Severe - a severe headache is added to the pathological process. High temperature rises, severe muscle pain. Not only regional but also distant lymph nodes enlarge. The rashes are located not only in the oral cavity, but on the skin next to it. They appear on the mucous membrane of the eye, on the eyelids, and on other parts of the face.
The severity of the pathology depends on the viral load (the amount of virus in the body) and the general reactivity of the body.
Preventive measures
Diseases characterized by the formation of ulcers on the tongue can be avoided if preventive measures are taken in a timely manner:
- If, after the measures taken, ulcers appear on the tongue again, it is recommended to undergo a more thorough examination.
visit the dentist regularly;
- Brush your teeth and mouth twice a day with high-quality toothpaste;
- teach your child to rinse his mouth after every meal to remove small particles;
- strictly adhere to restrictions regarding the consumption of foods that cause an allergic reaction;
- develop a diet so that it contains 65-70% fresh vegetables and fruits;
- take vitamin complexes to maintain immunity;
- protect the child from stress.
If, after taking measures, ulcers appear on the tongue again, it is recommended to undergo a more thorough examination. This sign may indicate problems with the digestive system or other diseases.
Clinical manifestations
Stomatitis in children is characterized by a gradual onset of the disease. Clinical signs of the disease do not appear immediately after infection. The incubation period is typical for this pathology; it lasts from two days to three weeks.
Symptoms of herpetic stomatitis in children appear starting from the prodromal period.
Each period has its own clinic:
- Latent – lasts up to two weeks. The child's sleep is disturbed and he refuses to eat. The baby becomes restless and whiny. He has increased salivation, possible nausea and vomiting. The lymph nodes are enlarged and painful on palpation.
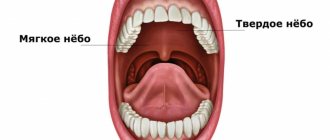
- The height of the disease - at this time rashes appear on the skin and mucous membranes. They are located on the soft, hard palate, gums, cheeks, lips and tongue. They are group or single, up to three millimeters in size. They are thin-walled bubbles filled with a clear liquid. Their formation lasts up to four days. The vesicles quickly open, then erosions and painful aphthae form. They are shallow ulcers covered with a white coating. The mucous membrane in the mouth is swollen and bleeding. The child develops a high temperature of up to 40 degrees. A runny nose, cough, and conjunctivitis occur.
- Fading - aphthae, erosions gradually heal and epithelialize. These formations heal without scarring. Often there is a wavy course of the disease. The periods of appearance of rashes alternate with rises in temperature.
The illness usually lasts up to two weeks. In children under one year of age, generalization of the process is possible. The development of sepsis, damage to all internal organs and meninges is likely.
Angular stomatitis in a child
Causes
In children, seizures are most often a manifestation of allergies, and can also appear while taking antibiotics. The mechanism is as follows: when using antibiotics, the microflora of the oral cavity is disrupted (both harmful and beneficial microbes die), against this background, space is freed up in which Candida fungi settle. It is these fungi that eventually cause the formation of buttocks.
Similar erosions can appear against the background of herpetic lesions, injuries, allergies, dry lips and cracks. It is important to determine the cause of their appearance and only then prescribe treatment.
Symptoms
Angular stomatitis (jams) - erosions with crusts that appear in the corners of the mouth - is also a fairly common form of stomatitis.
Treatment
- Antiseptics (chlorhexidine, miramistin) - use a gauze swab or ear stick to treat the surface of the wound.
- Keratoplasty (solcoseryl, oil solution of vitamins A and E) - applied to a dry surface after antiseptic treatment.
- Fighting the cause of the disease (if it is an allergy, we remove the allergens and prescribe antihistamines, if it is due to antibiotics, we prescribe drugs to restore the microflora and antifungal ointments, etc.).
Diagnostics
A patient suspected of having this disease is examined by a dentist. He asks the child’s parents about how the disease progressed. The diagnosis is established on the basis of the characteristic clinical picture of stomatitis, revealed during examination, anamnesis and characteristic complaints. Upon examination, typical mucosal lesions are revealed.
To confirm the diagnosis, laboratory testing of scrapings of the oral mucosa, the contents of ulcers, the patient’s saliva and blood is used.
The following are used for research:
- cytopolymerase chain reaction;
- immunofluorescence method;
- serological blood tests (RSC, ELISA, immunoglobulin M test);
- HSV test for the detection of immunodot G-specific glycoprotein.
These methods are used only for severe infections, as they are quite expensive.
Children's tongue diseases: what to do if painful ulcers appear in your baby's mouth
Among all the organs of the human body, the tongue is given special importance. It is with its help that we can distinguish the tastes of our favorite dishes, determine the consistency and temperature of products. In addition, the organ takes a direct part in verbal communication. Therefore, when suspicious tumors, inflamed areas and plaque appear on it, a person begins to experience severe discomfort and inconvenience. Anxious parents especially have a lot of fears and worries about this when signs of the disease are observed in young children. Today we will talk about what tongue diseases can appear in a child and what ulcers on the body of the organ usually indicate.
What are the types of tongue diseases in childhood?
Treatment
Treatment of herpetic stomatitis in children with mild and moderate forms is carried out on an outpatient basis. In severe cases and the development of complications, the baby is hospitalized. Treatment is carried out under the supervision of a pediatric dentist or periodontist.
Children are prescribed bed rest and a diet with pureed, non-irritating food. He is given separate hygiene items and dishes. Plenty of warm fluids are recommended.
The following drugs are prescribed:
- Non-steroidal anti-inflammatory drugs (Nise, Paracetamol, Nurofen) are used to relieve temperature and inflammatory reactions.
- Antihistamines (Clemastine, Loratadine) are used to relieve swelling of the mucous membranes.
- Antiviral drugs (Famciclovir, Acyclovir, Zovirax) are used at the beginning of treatment or in severe cases.
- Immunomodulators (Lysozyme, Gamma globulin, Thymogen) are used to enhance immunity.
During treatment, vitamin-mineral complexes and fish oil are used in monthly courses.
Local drugs that act directly on the mucous membrane are widely used.
For local treatment of herpetic stomatitis the following are used:
- antiseptics (Hexoral, Miramistin) - they are used to rinse the mouth every four hours for two weeks;
- ointments and gels with anesthetics (Kamistad, Lidochlor gel) are used for pain relief, they are lubricated with mucous membranes three times a day for up to two weeks;
- antiviral agents (Ganciclovir, Acicovir) - destroy the viral cell, gums are treated with these ointments five times a day, two weeks;
- proteolytic enzymes (Trepsin, Chymotrypsin) are used to cleanse the necrotic surfaces of ulcers; they are washed with these solutions twice a day.
- rinsing with decoctions of medicinal herbs (calendula, chamomile, sage) is carried out after each meal for up to two weeks;
- epithelializing ointments (Solcoseryl, Methyluracil) are used to enhance the healing of erosions and ulcers, used in the recovery stage, used up to four times a day for ten days.
Physiotherapy is applied locally. Irradiation of affected mucous membranes with ultraviolet and infrared rays is used.
Chronic aphthous stomatitis
Causes
Aphthous stomatitis is caused by staphylococcus, a microorganism that is found in large quantities in dental plaque and lives in carious cavities. Every person has this microbe and usually does not manifest itself in any way, but against the background of immune disorders. Often aphthous stomatitis can develop against the background of allergies, gastrointestinal diseases or injuries to the oral mucosa. Another factor in the development of the disease is dirty hands. This disease is often associated with children putting unwashed toys into their mouths, thereby increasing the total number and variety of microbes in the mouth.
Symptoms
Most often, manifestations of chronic aphthous stomatitis occur on the lips, transitional fold, gums, under the tongue and on the tongue - in places where the mucous membrane can be injured by teeth or spicy food.
- Minor change in general health. Characterized by enlargement of the submandibular lymph nodes, fever and weakness.
- On an externally unchanged mucosa, aphtha appears - a spot 5-10 mm in size, slightly rising above the surface of the mucosa, covered with a whitish film tightly fused to the mucosa and surrounded by a bright red rim. Aphthae are very painful when touched. Most often there are one or two aphthae, less often – several.
Must remember! It is necessary to accurately determine the type of stomatitis: herpetic or aphthous. With herpetic stomatitis, there are many small blisters that turn into erosions and sometimes merge with each other, and rashes on the lips are possible. With aphthous rashes, larger, single rashes occur only in the mouth. If you have stomatitis, you should definitely consult a dentist to determine the type of stomatitis and choose the right treatment tactics.
Treatment
Elimination of the factor that caused the disease:
- exclude all allergens (citrus fruits, chocolate, brightly colored foods...);
- if you are taking medications that can cause allergies, then you also need to take this into account (tell your doctor what you are taking and for how long);
- exclude rough, spicy, salty, sour foods;
- if stomatitis is caused by allergies, antihistamines (suprastin, loratadine) are prescribed;
- If the aphthae is due to injuries from sharp edges of a tooth or filling, it is necessary to put the tooth in order.
- in the first 3-4 days, treatment of aphthae is carried out exclusively with antiseptics (rinses, gels). You can use chlorhexidine, rotokan, miramistin, givalex, stomatidine, listerine, chamomile and calendula decoctions - you can take any of these drugs (or any other analogue). Use according to the instructions (there are preparations in ready-made form, and there are those that need to be diluted). Rinse (or wipe the mucous membrane in small children) 3-4 times a day.
- after 3-4 days, epithelializing agents are added: solutions of vitamins A and E, rosehip or sea buckthorn oil, solcoseryl.
- If relapses occur frequently, you should pay attention to your general health. In some cases, only joint treatment with an immunologist, gastroenterologist, endocrinologist and other specialized specialists can help cope with the disease.
Must remember! Aphthous stomatitis is, first of all, a microbial lesion. Oral hygiene, adherence to personal hygiene rules, as well as timely treatment of caries, caries complications, and removal of tartar in many cases are sufficient to avoid aphthous stomatitis.
Prevention
Preventive measures are aimed at preventing infection. This presents certain difficulties, since the vast majority of the population is infected with it. It is better if the child gets sick from it at an older age.
For this it is recommended:
- avoid contact with infected people;
- will provide personal utensils and personal hygiene products for the child;
- Kissing people with herpetic rashes is prohibited;
- strengthening the baby's immune system.
It is recommended that the child be provided with adequate nutrition and regularly given vitamin and mineral complexes.