Patients often ask doctors at the NAVA dental clinic with this question.
Relatively recently, a general rule was practiced: one tooth could be removed during one visit to the doctor. Medical technology is changing dynamically, but it is still followed today.
Doctors practice simultaneous removal of several teeth when patients are diagnosed with inflammation of the periosteum, odontogenic sinusitis, there are injuries, difficult eruption of (“eights”) or loss of (baby) teeth, advanced dental root diseases and other pathologies. These procedures carry higher risks. They require the use of large doses of anesthetics, and this is unsafe for the body.
What does a dentist consider when choosing removal options?
For dental operations, 2 types of anesthesia are used: local and general. In the second case, the risks of an overdose of anesthetics and the occurrence of complications associated with them are practically absent, but the body receives an increased dose of analgesics, which can also not have the best effect on its condition.
In each case, when choosing a one-time removal of one or more teeth, the dental surgeon takes into account:
- Health group, the patient’s well-being, the presence of acute, chronic pathologies, allergic reactions to certain drugs.
- The likelihood of complications during general or local anesthesia (dizziness, disorders of the digestive system, impaired coordination of movements, functioning of the respiratory system, etc.)
- Dosage, side effects, indications and contraindications of drugs that should be used for pain relief.
- Is there a risk of damage to adjacent areas of the dentition when several teeth are removed?
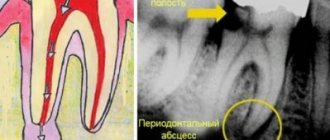
- The presence of various pathologies in the oral cavity, including periodontitis, periodontal disease.
- Psychological state of the patient - if he experiences a difficult-to-control fear of medical procedures, the number of the latter must be reduced to a minimum.
It is important to know: even with general anesthesia, it will not be possible to remove a large number of diseased teeth! This approach to getting rid of damaged parts of the dentition is dangerous because it slows down the healing process of wounds and significantly increases the risk of bleeding and inflammation.
Symptoms of hyperdontia in adults
Polyodontia affects permanent teeth more often than baby teeth. An adult usually develops dystopic and impacted supernumerary teeth.
Dystopic teeth are those that appear outside the dental arch. Most often they erupt on the lingual surface of the gums and in the palate. With this form of the disease, the patient typically:
- poor pronunciation of sounds;
- noticeable malocclusion;
- change in the usual arrangement of teeth: curvature of the angle at which they grow, as well as their rotation
- around its axis;
- frequent injury to the oral mucosa and, as a result, its inflammation;
- disruption of chewing processes, resulting in digestive problems.
Among other things, dystopic teeth often cause psychological problems. Due to a non-aesthetic, and sometimes completely unattractive smile, the patient becomes withdrawn and uncommunicative. Psychological problems, in turn, cause chronic diseases of the endocrine, digestive and nervous systems.
Impacted supernumerary teeth are teeth that do not erupt, but continue to remain in the bone tissue of the human jaw. Often they hardly make themselves felt until complications begin. Dentists diagnose this anomaly during a routine examination of the patient.
This abnormality in the number of teeth is accompanied by the following symptoms:
- normal teeth begin to loosen (the condition is considered pathological);
- the bone begins to protrude (if the impacted tooth is too close to the edge of the jaw);
- Aching pains appear periodically.
One of the most difficult situations is when extra teeth grow in place of impacted third molars. Wisdom teeth cannot grow and begin to negatively affect the roots of other teeth, which in turn can lead to serious complications.
About indications and contraindications for multiple removals
Simultaneous extraction of several teeth can be used when they are nearby. In such cases, the load during chewing food will be on the opposite part of the dentition, and the likelihood of complications (including alveolitis) will be minimal.
Dental surgeons at the NAVA clinic perform multiple tooth extractions if:
- Extraction of part of the dentition will take place without difficulty and severe bleeding.
- Neighboring (for example: baby) teeth are loose in their sockets.
- Injuries to the dentition have been diagnosed, and the affected parts must be urgently disposed of.
Multiple extractions are practiced in cases of extensive purulent lesions and jaw fractures. The main obstacles to the simultaneous removal of several teeth are cardiovascular diseases, high blood pressure, and slow blood clotting. In such cases, this extraction option is strictly prohibited.
Consequences of polyodontia disease
Polyodontia in humans can often be the cause of retention. This is a phenomenon in which normal teeth are unable to erupt due to the interference of supernumerary teeth. The former may remain in the jaw or take an abnormal position.
In addition, even if the complete incisor grows before the supernumerary one, the latter will be able to displace it. This will lead to the person being unable to chew food normally. And if several extra incisors grow at once, they can cause the loss of permanent teeth.
How to prevent complications?
The healing of the sockets, the risk of diseases in the oral cavity, and infection of the body directly depend on compliance with medical recommendations after tooth extraction.
To prevent complications from occurring, you should:
- Hold the cotton swabs that the dental surgeon placed in the sockets for at least 20 minutes.
- The first day after extraction, stop rinsing your mouth.
- From the second day, rinse it with water-salt solutions, decoctions of calendula, chamomile, oak bark, chlorhexidine and similar preparations.
- Avoid physical activity for several days, control your facial expressions, and do not touch the site of the operation with your hands.
Food and water can be consumed at least 3 hours after extraction (hot, cold, spicy, coarse foods are prohibited). As for alcohol and alcohol: you should abstain from the first for 3 days, from the second - for 48 hours.
General recommendations
High-quality compliance with the postoperative period will help to avoid complications and unpleasant consequences. Let's take a closer look:
- With such manipulation it is necessary to use a double dosage of an anesthetic substance. Therefore, it is not recommended to drive any transport during the day.
- At the end of surgery, time 4 hours. During this time, try not to eat food, then start with liquid meals.
- For 7 days, do not go to the bathhouse or lie in a hot bath.
- Limit physical activity to a minimum, try not to lift weights more than 1 kilogram.
- Rinse only from the third day as prescribed by the doctor.
- In the first two days, you can take painkillers if you experience discomfort. The specific drug and dosage are prescribed by the attending physician.
- If bleeding occurs, pain continues for more than three days, or other problems arise, visit your doctor immediately.
- If you take any medications on a regular basis, be sure to tell your doctor. Some pills may be limited for a couple of days, as some groups of medications thin the blood.
Each clinical case is individual!
At the same time, the question arises: is it possible to brush your teeth in the days after surgery? Only partially, and a number of precautions should be observed: do not touch the sockets with a brush, significantly reduce the usual amount of toothpaste, rinse the oral cavity slowly. After extraction, it is necessary to take painkillers, and in difficult cases, antibiotics and antihistamines. To ensure that procedures and medications do not harm the oral cavity and the body, they must be agreed upon with the specialists of the NAVA clinic. It is important to know: each treatment case is individual. And what helps one patient may be dangerous for another.
This article was checked and approved by the doctor Eduard Gennadievich Reunin.
Disadvantages of the All-on-6 technique
It's hard to talk about cons! The technique is actually very good and it allows you to solve all the patient’s problems in terms of chewing; it does not solve any of his other problems, but this technique is optimal for restoring dentition.
If a person is completely edentulous, that is, if the patient previously used a removable denture, or as a result of generalized periodontitis, the patient loses teeth and it is not possible to preserve the dentition, for example, as in this clinical case:
then in these cases this technique works 100% - it is a very good technique and it gives an excellent result.
On what implants is All-on-6 implantation performed?
All-on-6 implantation can be carried out on almost all implants that we use at the German Implantology Center - these are Astra Tech Sweden, Nobel Biocare, Straumann Switzerland and Ankylos Germany, see the following video about this:
All of these systems are excellent for this all-on-6 technique and give excellent results. Since all the systems that I listed, I’m not saying that this can only be done on them -
There are other implantation systems on which the all-on-6 implantation technique can be performed, but, in my opinion, the systems I have listed are optimally suited for this technique and give excellent results.
When All-on-6 uses basal implants
In our clinic, basal implants are used only in one case, when temporary fixation of the prosthesis is necessary. During the period of bone grafting or some other manipulation, when we cannot simply leave a person without teeth and we fix the structures on basal implants - this is only a temporary structure. We remove these (basal) implants after 3 or 6 months, depending on the situation, but we never leave them for permanent prosthetics.
All-on-6 for cancer and diabetes
Those patients who have some kind of malignant neoplasms and are undergoing treatment, if the patient is in remission and if this remission lasts more than 2 years and he tests tumor markers and everything is fine, then this patient can have implants installed, and we we install them.
Patients with diabetes are a fairly common disease now; we have many such patients.
Of course, we do not install implants as soon as the patient arrives and “everything is 6”, let us quickly install everything for you today - no, this is not our approach. The patient is interviewed, an anamnesis is collected, he is sent for tests, we look at sugar levels, what units, and communicate with the patient - this is type 1 diabetes, type 2 and we collect an anamnesis. And based on the anamnesis, we are already building a rehabilitation plan
:
How do you prepare for All-on-6 implantation?
Before starting the “all-on-6” operation, the patient sees an orthopedist. The orthopedist discusses in detail with the patient, finds out his wishes, assesses the situation, makes optical impressions, and sends him to CBCT in order to compare the optical impressions of the intraoral scanner and bone computed tomography.
And the complete rehabilitation is carried out first in digital form, when all the implants are placed in the right positions in the program, a surgical template is ordered, and we already know completely at the stage of the operation that everything has been predicted. We know in what place the implants will be installed, what diameter, what length, at what angle they will be installed, what orthopedic superstructure will be - this is necessary for fixing the prosthesis. That is, at the planning stages we do everything to eliminate force majeure during the operation and in order to get the result that we want to get - this is a good result.
What tests should be taken before All-on-6?
Before implantation of “all on 6”, we recommend that patients take a blood test, in which we will indicate both the patient’s sugar and hormonal parameters. And after this we can move on to further rehabilitation of the patient.
Anesthesia
Before the operation, complete anesthesia of the required area of the jaw is carried out. The most commonly used is local anesthesia, which is carried out using a carpule syringe and an anesthetic. Anesthesia of the lower jaw occurs 8-10 minutes after the injection. The duration of the analgesic effect depends on the drug used and is 2-4 hours. The operation itself is completely painless, but after the anesthetic wears off, the patient begins to feel pain. Therefore, after the procedure, the specialist gives prescriptions about the need to use medications (painkillers, anti-inflammatory, antimicrobial agents).
Complex tooth extraction: when is it necessary?
Clinical indications for which the dentist prescribes complex tooth extraction are as follows:
- the presence of an unerupted wisdom tooth in the jaw;
- if the figure eight is incorrectly positioned;
- when removing molars with two or three roots;
- with a severely damaged or twisted root;
- in case of fusion of the tooth root with the jaw bone tissue;
- in the presence of a fistula or cyst;
- with excessive fragility of the crown due to treatment with resorcinol-formalin composition.
The operation itself consists of several stages and is carried out under the influence of powerful anesthetics.
Stages of complex tooth extraction
Complex removal surgery is carried out only after x-ray diagnostics, during which the shape, length and depth of the roots are determined. If the patient has inflammation, he is prescribed treatment with antibacterial drugs.
Technique of the procedure
Wisdom tooth removal is carried out in the following order:
- the gum is separated from the neck of the tooth by making an incision in the soft tissue;
- if necessary, the interroot septum is sawed or sections of bone tissue are cut out at the location of the tooth;
- then, using forceps, the tooth is rocked and pulled out of the socket;
- Sutures are placed on the gum.
Painkillers are not required after the procedure, since the effect of the anesthetics is still present.