From this article you will learn:
- why does the socket hurt after tooth extraction,
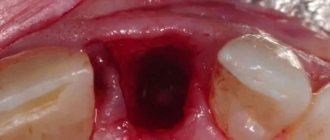
- what is alveolitis: photos and videos,
- How is alveolitis treated?
The article was written by a dental surgeon with more than 19 years of experience.
Alveolitis is a classic complication that occurs after tooth extraction and consists of the development of inflammation of the socket of the extracted tooth. Often alveolitis is also called “dry socket” (this is due to the fact that the alveolar bone in the depths of the socket is exposed due to the loss of a blood clot).
On average, alveolitis develops after tooth extraction in 3-5% of cases, but this applies to teeth of any location with the exception of wisdom teeth. When the latter are removed, alveolitis occurs in 25-30% of cases, which is associated with the greater complexity and traumatic nature of the removal process.
Dry socket after tooth extraction: photo
You can see what normal healing of a socket should look like (at different times from the moment of extraction) in the photo in the article: → “What a socket should look like after tooth extraction”
What should gums normally look like after tooth extraction?
When a tooth is pulled out, a hole remains in its place, which immediately fills with blood. During the first 30 minutes after surgery, the bleeding stops and the blood clots. A burgundy blood clot forms, completely covering the wound and performing a protective function. If healing proceeds normally, then after 1–2 days the blood clot changes its color from dark red to whitish, covered with a yellow film. This color is explained by the presence of a special fibrin protein in the clot, which is produced by the body during blood clotting.
The wound gradually heals, its edges come closer together, and granulation tissue is actively formed on the surface, which, in the case of normal healing, almost completely covers the hole already on the seventh day after extraction. But if the removal was difficult and traumatic, then the regeneration process is slower and can take up to 3 weeks. Next, young bone tissue is formed at the site of granulation - this lasts another 2-3 months.
Important! The recovery process is painless, but in the first 5 days after extraction the patient may suffer from the natural physiological consequences of the intervention: pain, non-infectious inflammation, redness and swelling of the gums. However, every subsequent day a positive trend should be observed - the unpleasant sensations begin to subside.
Tip three: limit your consumption of certain foods
To prevent an unpleasant odor from appearing from the socket after tooth extraction, everything must be done to ensure that the protective clot in the wound remains intact. And dietary habits in the first few days play an important role in this.
“After removing my wisdom tooth, I had a terrible smell from the socket. It just smelled like some kind of rot, but the hole was still huge after the operation. There was no pain. I went to the doctor to find out what was wrong, because at work our tables are very tightly spaced, and I’m sure that all my colleagues could easily smell this stinking smell. The doctor cleaned something there, and the stench went away immediately. It turned out that food was clogged into this deep hole, and this food was rotting, and I was unable to clean it out on my own. Now I’m afraid that I might get full again, I can’t imagine how to eat until all this drags on. I’ll chew for a week on only one side of my jaw...”
Anna, review from 32top.ru
You cannot eat for the first 2 hours after surgery, but after half an hour you can already drink water. It is better to avoid eating cold, hot and solid foods for 2-5 days. You also need to exclude spicy and salty foods from your diet, because they can cause additional discomfort, irritation of damaged mucous membranes and slow down the healing process.
After the procedure you need to take soft, warm food
You should not consume foods and drinks that increase blood flow to the head and increase blood pressure: coffee, pepper, pomegranate, garlic, cinnamon, citrus fruits, ginger. Alcohol is prohibited. Such foods and drinks can cause swelling and bleeding, which will wash away the protective clot.
In the first days, give preference to soft, liquid and warm foods. Chew on the side of the jaw opposite the one where surgery was performed.
If your doctor suggests removing a tooth, consider immediately replacing it with an implant. Today there is a one-time method of implantation - you do not have to wait for the hole to heal. True, if the specialist’s recommendations are violated, an unpleasant odor after tooth extraction and simultaneous installation of an implant can also occur, but not against the background of alveolitis, but against the background of peri-implantitis.
Symptoms of the pathological process
| Symptom | Features of the flow |
| "Dry hole" | Without a blood clot: if for some reason it did not form (for example, due to a blood clotting disorder) or was washed out/damaged due to the careless actions of the patient, then the pathological inflammatory process in it may begin on the second day after extraction |
| Wound festering after tooth extraction | A dirty gray coating forms on the wound, less often it can be black. During pressure, pus may be released from the hole or gum around. There may also be pieces of food in the wound itself. |
| Painful sensations | At first, the pain is weak and aching, and only intensifies when you press on the wound or eat food. If left untreated, the pain becomes acute, radiates to the jaw and head, and is not relieved by analgesic drugs. |
| Bad breath | The putrid odor persists even after hygiene procedures and the use of “mouth fresheners” |
| Deterioration of general condition | Temperature rises to 38.0°C. It becomes difficult to chew and swallow food, as well as open your mouth. Lethargy and weakness. In some cases, not only swelling of the gums appears, but also swelling of the soft tissues of the face, as a result of which the symmetry of the face is disturbed |
Important! Observing a similar situation, some patients try to squeeze out the pus, pick at the wound, clean it of plaque, or pull out the clot with a toothpick or cotton swab. Such actions are prohibited! They are unacceptable, as they can lead to even more serious complications and the advancement of pus into the deeper layers of tissue.
Reviews
I recently went to have my lower molar removed because all that was left was a stump that was no longer suitable for a crown. The removal went quickly and without almost any pain, they prescribed me to rinse my mouth and sent me to treatment at home.
The very next day, severe pain began in the place where the tooth used to be and the gums became swollen. Another terrible bad breath appeared. In the end, I came to the doctor who pulled my tooth the day before. She looked and advised me to “brace up” and apply a heating pad with ice to my swollen cheek. After a couple of days, the swelling subsided, but the gums did not hurt any less. I took Nurofen several times a day. But the pain never stopped, so I went to that aunt again.
They took a picture and told me everything was fine, but there were sharp bones from where my tooth used to be. So they decided to remove them. It was very painful when they picked at my gums again and removed these “bones”, then they put gauze, forced me to bite and sent me home.
Within a couple of hours, hellish throbbing pains began, so I decided to go to a nearby private clinic, where everything was explained to me. It turns out that my tooth was removed poorly, there were many pieces left from the destroyed tooth and bones from the jaw, so it all mixed with infection and produced pus. With an injection, they cleaned it all out with absolutely no pain, put a gauze pad with ointment on top and gave me recommendations. On the same day I felt better, so I didn’t go back to the doctor who removed my tooth.
Why complications develop
Usually the gums around a tooth that has recently been removed fester because the wound has become infected. But how could pathogens end up in the hole? In some cases, the hole could already be primarily infected. This often happens when extraction is performed against the background of an inflammatory process caused by deep caries, pulpitis, periodontitis, as well as cysts and granulomas.
But the wound can also become infected a second time, that is, the problem develops due to external factors. Let's list them:
- the blood clot did not form initially or fell out of the wound after some time: then the hole remains defenseless against bacteria living in the mouth, as well as against saliva and small pieces of food. There are many reasons why a clot did not form or did not survive: traumatic removal, chronic diseases, non-compliance with recommendations after extraction,
- During the procedure, the doctor did not perform asepsis of the wound well enough and did not remove small fragments from it: for example, remnants of a root. Or fragments of hard carious tissues, tartar and plaque that have fallen into the hole from neighboring units. This often happens if the extraction is carried out urgently, without proper preparation and sanitation of the oral cavity,
- during the rehabilitation period, the patient did not take good care of the wound and performed unacceptable actions: for example, chewed on the sore area or cleaned it with a brush, actively rinsed the mouth or touched the intervention area with fingers/tongue,
- Inflammation of the gums is sometimes provoked by internal diseases of the body: in particular, the stomach and intestines, as well as the nasopharynx.
“There are situations when the blood clot in the socket is completely intact, but acute inflammation of the gums still develops. This happens because fragments of the extracted tooth remain inside the wound. But it should be noted that in good clinics and with experienced doctors this situation is simply excluded, since an X-ray examination is carried out at each stage of extraction,” says dental surgeon D.V. Kolikov.
Causes of inflammation
The disease can develop only after tooth extraction. Most often, the hole formed after removal heals within a day after the operation, and the patient feels better. But if the blood clot that covers the open wound moves or becomes deformed, an infection can penetrate into the hole, in which case alveolitis of the gums develops. As a result, the surface of the wound heals for a long time, and the patient suffers from complex discomfort.
Predisposing factors for the development of inflammation:
- Surgical injuries during complex removal. The more complex the operation, the more pronounced the postoperative inflammation of the bone tissue will be, and the more likely the release of direct plasminogen activators.
- Complex extractions associated with tooth segmentation, osteotomy, detachment of the mucoperiosteal flap. Complex operations increase the chance of developing alveolitis 10 times.
- Removal of wisdom teeth. The denser, less vascularized bone tissue adjacent to the figure eights is prone to the formation of dry sockets.
- General diseases of the patient. Alveolitis often occurs against the background of concomitant diseases. For example, patients with diabetes mellitus or immunocompromised patients are more susceptible to alveolitis due to impaired healing processes in the tissues.
- Taking oral contraceptives. The estrogen contained in these drugs may indirectly enhance the fibrinolytic process, causing the breakdown of the blood clot.
- Smoking. The direct connection between smoking and alveolitis has been repeatedly proven clinically. According to studies, the risk of socket inflammation in smokers increased 4-5 times compared to non-smokers. The incidence increased by more than 20% in patients who smoked 1 pack per day and by 40% in patients who smoked immediately before and after surgery.
- Dislocation of a bunch. If the socket is handled carelessly and there is negative pressure (for example, due to drinking through a straw), alveolitis may develop.
- Bacterial infections. Dentists agree that bacterial infections are the main risk factor for dry socket.
- Poor oral hygiene. The incidence of alveolitis increases significantly with poor oral hygiene.
- Excessive use of local anesthetics. According to some studies, excessive use of an anesthetic with a high concentration of a vasoconstrictor can provoke ischemia and make it difficult for the socket to fill with blood. This condition also increases the risk of alveolitis.
In fact, alveolitis is a fairly rare disease. According to statistics, it affects approximately 3% of patients who have undergone tooth extraction surgery. More often than not, the socket is not formed properly when lower incisors and molars are removed.
But alveolitis is especially common when removing lower wisdom teeth: according to experts, in approximately 20% of cases, the removal of “eights” with difficult eruption is complicated by alveolitis. In addition, it is believed that the risk of developing the disease is inextricably linked with age. This is explained by the fact that metabolism slows down, immunity is weakened, and the regenerative abilities of the body deteriorate.
When removing which teeth complications most often arise?
In clinical practice, there are common cases when the gums fester after the removal of a wisdom tooth. After all, the “eights” are massive and have many winding roots. They often have an incorrect position in the bone or do not erupt completely. Their extraction is always complex, multi-stage and traumatic. After manipulation, a large wound remains in the oral cavity, which is the entrance gate for any infection.
The problem is very common when removing teeth from the lower jaw, since the bone here is very massive. To extract the roots from it, the doctor has to make significant efforts, and the infection that gets into the wound quickly spreads deep into the tissue and covers large areas.
As noted above, a complication in the form of inflammation of the gums often occurs when removing teeth that have been severely damaged by trauma or dental disease, as well as those with a cyst or granuloma at the root.
Alveolitis photo of the hole
Often the hole may look normal, that is, without pronounced deviations, but this can be seen in the photo. But here you can consider the presence of a narrow inlet. It is also not very clear whether a clot is present in this case. Of course, making a diagnosis under such circumstances is very difficult. To do this, the doctor will have to conduct a full examination, which is performed using modern technology. And only because of the constant, very often in the form of increasing pain, smell from the open socket, tumor of the gingival tissue, can alveolitis be suspected.
Extraction complications: types, features
If after tooth extraction the hole, as well as the gums around it, soft and bone tissues fester, this may indicate various complications of extraction. Let's look at the most common of them in more detail.
Alveolitis
This is the disease that usually starts it all. Actually, alveolitis is a purulent inflammation of the socket of an extracted tooth, resulting from tissue infection. The pathology most often develops because the patient damages the protective clot, or the clot does not form at all.
There are several forms of alveolitis: serous, purulent and chronic. The first form manifests itself already 2–3 days after extraction and is characterized by moderate pain and the absence of any noticeable symptoms. But if you do not start treatment, then already on days 4–7 the patient is faced with a purulent form of the disease, accompanied by acute pain and a sharp deterioration in well-being. If you do not consult a doctor during this period, the inflammatory process becomes chronic, when all the symptoms weaken, but tissue damage continues.
Cyst
Many patients think that a cyst can only form above a tooth or under a tooth that is located in the oral cavity. However, swelling can also occur where the root has recently been removed. The pathology may be primary or secondary. Primary develops when an element with a cyst was removed, but the doctor did not completely clean it and remove it.
A secondary tumor appears in cases where the specialist did not do a good job of curettage and cleaning the hole from small fragments. Then small fragments of the root or walls of the extracted tooth are covered with a protective shell, that is, a cyst is formed. This form of pathology may not manifest itself for a long time, but if a person’s immunity drops, the cyst breaks through, causing sharp pain and an acute inflammatory process. Fistula tracts may also form, through which pus will leak out or into the internal tissues.
Gingivitis
Interestingly, gingivitis can also develop not only where teeth are present, but also where they are not. Usually, after removal, traumatic gingivitis occurs, which occurs due to excessive pressure on the tissue and severe damage to it. With this disease, the gums become inflamed, red and swollen; they can itch, hurt, and bleed from eating solid foods and when brushing.
Traumatic gingivitis appears locally, but if it is not treated in a timely manner, the inflammation will begin to spread to neighboring areas and after some time will become generalized, that is, it will affect the entire row. Additional factors can contribute to the rapid development of this disease: poor oral hygiene, accumulation of soft and hard bacterial plaque, consumption of sweet and soft foods, weak immunity.
Suppuration of hematoma
Some patients develop a hematoma, which is a large bruise, after extraction. The problem arises due to traumatic root extraction, damage to blood vessels and capillaries during the procedure, and also due to poor blood clotting. Typically, the hematoma gradually resolves on its own or under the influence of medications prescribed by the dentist. But it also happens that it can fester, then the patient’s cheek swells and severe pain appears. Cases of hematoma suppuration often occur in people with diabetes, since their tissue regeneration processes are impaired and healing occurs very slowly.
Flux or periostitis
If alveolitis is an infection of the socket of an extracted tooth, then flux is an infection of its periosteum. That is, bacteria penetrate into deeper layers in the absence of timely treatment of superficial inflammation.
The symptoms of the pathology are characteristic: acute pain, swelling of the gums and face, facial asymmetry, inability to open the mouth, general and local increase in body temperature. The cheek of people who have gumboil “burns.”
Osteomyelitis
If the gums fester after tooth extraction, and a person starts the process and does not know what to do, then the infection penetrates into the deeper layers of the tissue and can affect the bone. Often osteomyelitis is a complication of flux or cyst.
This is a very dangerous disease that needs to be treated in a hospital setting. If the treatment technique is incorrect or there is no treatment, there is a very high probability of pus from the affected tissues entering the bloodstream, damage to internal organs, pulmonary failure and the development of sepsis. Also, complications of osteomyelitis often include a fracture of the lower jaw, destruction of the mandibular joint, atrophy and severe thinning of bone tissue, and destruction of teeth located adjacent to the lost one.
Phlegmon
Gum suppuration can lead to phlegmon, when the inflammatory process spreads to the soft tissues of the face. This is an extremely unfavorable complication1 of extraction. Inflammation has no defined boundaries and therefore very quickly affects more and more new areas. The pathology is fraught with severe intoxication of the body, changes in shape and disruption of facial aesthetics. It is better not to let it develop; the patient will need long-term rehabilitation and more than one cosmetic surgery to tidy up his appearance.
Read about the signs and consequences of phlegmon in the feature article on the website.
How to treat alveolitis?
Effective treatment of such a disease can cause objective difficulties. The dentist must have extensive experience in the field of surgery in order to build a suitable plan for future treatment and implement it.
The treatment process for alveolitis consists of the following stages:
- Anesthesia of the affected area using local or trunk anesthesia.
- Washing out food particles, saliva and blood clot residues from the socket using a syringe and a blunt-tipped needle. To do this, use warm antiseptic solutions: furatsilin, hydrogen peroxide, manganese solution, chlorhexidine.
- Particles of tissue decay, food, bone or tooth root fragments, granulations that remain after washing are removed using a sharp surgical spoon. Actions must be carried out with great care, since it is impossible to injure the walls of the hole.
- Repeated rinsing of the extracted tooth socket with antiseptic solutions.
- Drying with a sterile cotton swab.
- Dust with anesthetic powder.
- Applying a gauze bandage with iodoform impregnation or an anesthetic and antiseptic bandage "Alvogyl".
As a dressing, you can also use biological antiseptic tampons, a hemostatic sponge with kanamycin or gentamicin, and paste preparations with antibiotics. The bandage performs a protective function, preventing mechanical, biological, chemical irritants and pathogens from entering the inflamed hole.
Pain in the socket with serous alveolitis disappears forever after such treatment. After two to three days, the inflammatory process subsides. If treatment is carried out when the disease has already taken a purulent form and the pain has become more intense, a strip of gauze with an anesthetic and antiseptic solution is inserted into the hole: alcohol tincture of propolis, camphorophenol liquid. Blockades (impregnation of soft tissues at the site of inflammation) of an anesthetic in combination with lincomycin, as well as the Traumeel solution, administered according to the principle of a conventional injection, are quite effective.
Proteolytic enzymes are used to cleanse the socket of tissue that has undergone necrosis. To do this, a gauze strip moistened with a solution of crystalline chymotrypsin or trypsin is inserted into the well. Enzymes gradually break down dead tissue and clean the wound surface.
Physiotherapy must be present during the treatment process. Apply: microwave therapy, fluctuarization, infrared laser rays, ultraviolet irradiation. Baths with a solution of manganese or sodium bicarbonate have good antiseptic properties.
Among medications, the patient is prescribed complex vitamins, analgesics and sulfonamide drugs. If there is a threat of further development of the disease, antibiotic therapy is carried out. This is daily:
- Treating the hole with antiseptics;
- Carrying out a blockade;
- Changing the bandage.
The procedures continue until the pain stops completely. After a week, the walls of the socket begin to heal and become covered with young mucous tissue, but signs of inflammation may still be present in the clinical picture. After a couple of weeks, the swelling subsides, the mucous membrane takes on a normal, pink color.
Is it possible to treat gums at home?
In a situation where the gums are festering, it is important to understand how to treat the pathology. Naturally, any doctor will tell you that you need to immediately seek professional medical help, and this will be the only right decision. Making an appointment with your doctor is very important! But if it is impossible to visit a specialist right now, before visiting the clinic, you can carry out antiseptic treatment of the oral cavity with herbal decoctions (chamomile, sage), Chlorhexidine or Miramistin. Do not rinse vigorously or intensively. Just put some liquid in your mouth, hold it for 2-3 minutes, then spit it out. Repeat as often as possible, up to 10–12 times a day.
For pain, you can take pills from your home medicine cabinet. Read about the best and most effective of them here. But remember that at home you can only suppress the symptoms of the pathology for a short time, but you will not be able to cure it on your own.
Bad breath – is it always a pathology?
We have already found out that only the smell of iodine can be considered normal, provided that the doctor tamponed the hole with the appropriate turunda after the extraction procedure. This smell goes away on its own after a few days.
There is another smell (and taste) that does not indicate the presence of a pathological process for several days after extraction - it is steel, metallic, or even iron. It appears against the background of the fact that the damaged socket and the tissues around it secrete ichor, and it, like blood, has exactly that smell. True, in this case these two concepts should not be confused. Because bleeding for several days is normal, bleeding is abnormal and requires urgent medical attention.
A metallic taste may be present for several days.
People with poor blood clotting, diabetes mellitus and high blood pressure, smokers, and women taking hormonal contraceptives are more at risk of bleeding that does not stop for a long time, accompanied by a characteristic metallic odor. If you have at least one of these factors, then before tooth extraction, be sure to inform your doctor so that he can prescribe you the appropriate medications for maintenance therapy.
If the smell is stale, putrid, rotten, this is a signal of a pathological process and is always a reason to consult a doctor.
What actions are prohibited?
After extraction, the doctor usually gives recommendations on what can be done and what absolutely cannot be done. So, to avoid complications, you need to exclude hard, spicy and hot foods from your diet. Do not overheat or perform physical activity. It is not recommended to eat on the side of the jaw where the wound is located. If, however, the gums of an adult or a child become inflamed and fester, then some actions can cause even more harm:
- active mouth rinses,
- the use of hydrogen peroxide and soda: these drugs further irritate damaged tissues and dissolve the protective clot,
- applying garlic, lard and other products to the wound: this can cause a burn. Products can become a medium for the accelerated proliferation of pathogenic bacteria,
- attempts to remove pus, plaque, food debris from the wound using fingers, brushes, sticks and toothpicks, as well as various sharp objects,
- warming up the inflamed area: this will contribute to the spread of infection and damage to neighboring areas, increasing swelling,
- taking painkillers that thin the blood: for example, Aspirin,
- taking antibiotics and self-medication.
Symptoms for an urgent visit to the dentist
When such an unpleasant symptom as pain and bad breath intensifies, the temperature rises, the gums swell, and dental surgery may even be required. It is important to see a dentist on time.
- The doctor will carefully examine the oral cavity and the surgical area.
- A small spoon is used to diagnose the hole.
- If alveolitis develops, special therapy is prescribed. First, anesthetics are introduced, then plaque and pathogenic microbes are removed.
- Then the wound is treated with an antiseptic, and the necessary medications are applied.
- Stitches may be needed.
You should contact the dentist when the gum tissue is swollen, you feel severe pain, your cheek and neck are swollen. In such a situation, pus collects in the wound area. The dentist prescribes rinsing, disinfection procedures, painkillers, and antibiotics. With severe tissue injury, an abscess may develop. At risk are those patients who do not follow the doctor’s recommendations. Remember that timely contact with a doctor is the key to quick treatment.
Treating Suppuration at the Dentist's Office: What to Expect
If you identify alarming symptoms, you need to consult a doctor as quickly as possible, because the treatment of alveolitis is faster and easier than phlegmon and osteomyelitis. And if alveolitis is treated in the dentist’s office and does not cause serious health complications, then purulent inflammation of soft and bone tissues is eliminated within the hospital, and after that the patient faces a long and often difficult rehabilitation.
So, if you find pus in your gums after tooth extraction, you should immediately go to the doctor. The specialist will conduct an examination, administer anesthesia and begin treatment. First, the dentist will curettage the hole, that is, remove the clot from it, clean it of necrotic masses and food debris, and remove fragments of roots and hard tissues. Then the wound is washed with antiseptics, after which the doctor can place a medicine in it and apply stitches.
The specialist will also prescribe you products that you will need to use at home until the tissues are completely healed: antibiotics (Sumamed, Azitral), antiseptics, gels and ointments (Metrogil Denta, Cholisal, Asepta). In some cases, an additional course of physiotherapy using laser or ultraviolet light may be prescribed.
To quickly eliminate discomfort, speed up tissue regeneration and prevent complications, at first it is better to eat mainly soft and liquid foods, give up smoking and bad habits, and carefully but carefully carry out oral hygiene.
What can you do at home -
After the acute symptoms of inflammation have subsided, there is no need for antiseptic turundas inside the socket, because they do not help the wound to heal (epithelialize) faster. At this stage, the best treatment method will be to fill the hole with a special Dental adhesive paste (Solcoseryl). This drug has an excellent analgesic effect (after 2-3 hours the pain will practically stop, and after 1-2 days it will go away completely), and also speeds up healing many times over.
Scheme of use - this paste is added to a hole that has been washed with an antiseptic and slightly dried with a dry gauze swab (completely filling the hole). The paste is perfectly fixed in the hole and does not fall out of it. There is no need to remove the paste from the hole, because... it slowly dissolves on its own, giving way to growing gum tissue. The only thing that may be required is to periodically add it to the hole.
How to rinse the hole from food debris -
In some situations (when the turunda has fallen out of the hole, and there is no way to see a doctor right away), it may be necessary to wash the hole. After all, after each meal, the hole will become clogged with food debris, which will cause new inflammation. Rinsing will not help here, but you can easily rinse the hole with a syringe.
Important : from the very beginning you must bite off the sharp edge of the needle from the syringe! Next, bend the needle a little and fill a 5.0 ml syringe with a solution of Chlorhexidine 0.12-0.2% (it is sold ready-made in every pharmacy for 20-30 rubles). Screw the needle tightly so that it does not fly off when pressing the syringe plunger! Place the blunt end of a bent needle into the upper part of the socket (do not insert too deeply to avoid injuring the tissue), and rinse the socket under pressure. If necessary, do this after every meal.
In principle, after this the hole can be dried with a gauze swab and treated with Solcoseryl. We hope that our article on the topic: Alveolitis after tooth extraction, symptoms, treatment - turned out to be useful to you!
Sources:
1. Higher prof. the author’s education in surgical dentistry, 2. Based on personal experience as a dental surgeon, 3. National Library of Medicine (USA), 4. “Outpatient surgical dentistry” (Bezrukov V.), 5. “Propaedeutics of surgical dentistry” (Soloviev M. .).
Comments
When can you brush your teeth after tooth extraction? And is it possible to immediately use an irrigator if you can’t use a brush?
Vita (01/14/2020 at 00:45) Reply to comment
- You cannot use a brush on the first day after tooth extraction. On the second day, you can use a brush, but you must avoid the area where the intervention was performed. As for the irrigator, it should not be used during the first week after tooth extraction.
Editorial staff of the portal UltraSmile.ru (01/18/2020 at 09:22) Reply to comment
My wisdom tooth was removed, the hole was treated and sewn up. after treatment everything heals well, it doesn’t hurt, but the smell is strong, dental, not putrid, some kind of medicinal, it drives me crazy, it seems to me that everyone around me feels it. My job involves close communication with people. What should I do?
Irina (08/27/2021 at 11:04 pm) Reply to comment
Write your comment Cancel reply
Therapeutic treatment
Treatment is carried out according to a standard scheme and it is important to start it in a timely manner:
- Cleaning the hole from food debris, plaque, and dead tissue;
- A thorough inspection of the hole, checking for the absence of roots and foreign elements;
- Washing the wound with hydrogen peroxide;
- Drying the wound;
- Putting anti-inflammatory drugs into the hole.
After treatment, the doctor gives recommendations to the patient on oral care. A few days later, the patient comes back for an examination to make sure that the treatment has given positive results and the wound is healing. It is important to rinse your mouth with herbal decoctions at home. Do not eat hard foods. For pain relief, you can use Nimesil or Ketanov.
Additional physiotherapy treatment (click to expand)
Physiotherapeutic treatment is an important addition to drug therapy; with the help of physiotherapy, the intensity of inflammation can be significantly reduced and healing time can be accelerated. For alveolitis, the following techniques are used:
- UV therapy - the hole is irradiated with short-wave ultraviolet light, which kills pathogenic microorganisms and reduces the level of inflammation.
- SMV therapy is a method of treatment with an electromagnetic field, based on the effect of centimeter waves on the area of inflammation. The procedure helps improve blood circulation and metabolism, due to which toxic substances are removed from tissues faster and regeneration processes are accelerated. SMV therapy also has an analgesic effect.
- UHF therapy – the body is exposed to a high-frequency electromagnetic field. For alveolitis, UHF therapy is used if the patient's regional lymph nodes are enlarged.
- Electrophoresis – medications are injected into inflamed tissue using electrical impulses. For post-extraction alveolitis, electrophoresis is used to reduce pain. For this purpose, solutions of novocaine, lidocaine, trimecaine are used.
- Fluctuarization is a treatment technique with pulsed currents of a sinusoidal shape with a low frequency. As a result of the procedure, blood circulation and lymph flow improves, swelling resolves, and the level of inflammation decreases.
- Laser therapy - the hole is exposed to infrared laser radiation, which has an anti-inflammatory effect, reduces swelling and redness of soft tissues, and accelerates healing.