Removal of impacted teeth
Impacted teeth are those that did not erupt in time and remained in the thickness of the bone tissue, at different depths - in the dental arch or outside it.
Canines, premolars, incisors, unerupted and semi-erupted wisdom teeth may be impacted. They often do not have enough space in the dental arch; the gums around them can become inflamed and a pathological periodontal pocket can form. Impacted teeth are removed if they are associated with pain, discomfort, if they cause inflammation and orthodontic movement of them into the dental arch is impossible. Removing impacted teeth varies in complexity. Additional x-ray examination may be required before removal.
Removal of wisdom teeth (and buds)
The problems of wisdom teeth and frequent complications from their eruption or simple presence are relevant in modern surgical dentistry.
Wisdom teeth are also the eighth teeth, third molars. The rudiments of the third molars begin to form at 6-7 years of age, and the roots of the eighth teeth - at 15-17 years. Wisdom teeth finish forming at 21-22 years of age (in rare cases, at 25-27 years of age). Therefore, if wisdom teeth did not erupt until the age of 27, then it is pointless to expect that they will erupt on their own later.
A wisdom tooth is a rudiment that has lost its function in the process of human evolution. The jaw has become smaller, since the diet of modern people is dominated by soft food and the chewing load is low. At the same time, there are as many tooth rudiments left as there were thousands of years ago.
Sometimes, when wisdom teeth are optimally erupted, they can be used as autografts to replace the extracted teeth. But so far the possibilities of this procedure are limited.
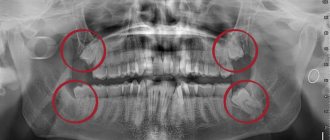
92% of adults have a complete set of third molars (one on each side of each jaw). At the same time, in more than 25% of people, wisdom teeth remain impacted, that is, they do not erupt at all. As a rule, this is due to a lack of space in the dentition. In 78% of cases, wisdom teeth erupt with complications. This may be pericoronitis, destruction, change in the position of adjacent teeth, malocclusion, tumor-like and/or cyst-forming processes, etc.
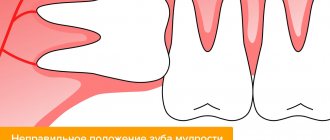
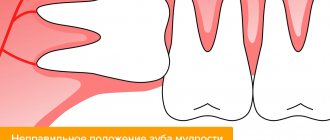
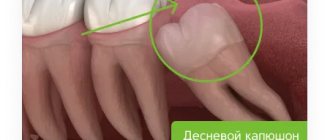
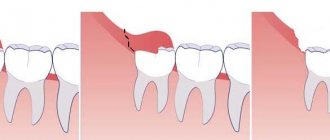
The eruption of wisdom teeth, in more than 80% of cases, is accompanied by various purulent-inflammatory complications and poses a threat to the patient’s health. A hood of mucous membrane is formed over the erupting tooth and a pocket is created around it, where plaque, food debris and bacteria actively accumulate.
This creates conditions for the development of purulent inflammation (the so-called pericoronitis), which, due to the proximity of the purulent focus to vital organs and structures, is a dangerous condition. Excision of the hood of the mucous membrane is only a temporary and not always effective measure, since it quickly recovers and makes further treatment difficult due to the formation of scars.
Materials and research methods
To accomplish the assigned tasks, 26 patients aged from 12 to 45 years old with a diagnosis of canine retention in the upper jaw were examined and treated. Of these, 10 patients (38%) were diagnosed with vestibular retention of the canines, and 16 patients (62%) were diagnosed with palatal retention of the canines.
In patients with vestibular retention of the canine in the upper jaw (10 people), a delay in the change of primary canines was observed in 6 patients (60%), edentulous lateral incisors in 2 patients (20%). Bilateral vestibular retention was detected in 2 patients (20%).
In patients with palatal retention of the canines on the upper jaw (16 people), a delay in the change of primary canines was observed in 12 (75%), edentulous lateral incisors in 4 (25%).
The presence of supernumerary tooth rudiments in the area of the impacted canine was noted in one patient. Bilateral palatal retention of the canines was detected in 2 patients.
Patients diagnosed with palatal impaction of the maxillary canine teeth were further divided into two separate groups, as the location of the canine can vary greatly and the treatment strategy depends on its location. The crown of the canines in patients of the 1st group was located no higher than the level of half the length of the incisor root, the crown of the canines of the 2nd group of patients was located above the level of half the length of the incisor root.
42 orthopantomagrams were analyzed, 10 targeted intraoral radiographs and 4 occlusal radiographs were taken.
Surgical exposure of 28 crowns of impacted canines was performed, of which 10 were vestibular impacted, 16 were palatally impacted.
Orthodontic traction was initiated by 28 impacted canines in the maxilla. During orthodontic treatment, 28 impacted canines were installed in the dentition, the position of the teeth and the shape of the dentition were normalized. Associated malocclusions accounted for 91% of the total. In 2 patients over the age of 30 years, impacted canine teeth were diagnosed with impacted canine ankylosis at the stage of orthodontic traction. The diagnosis was established on the basis of the absence of canine movement during 6 months of active orthodontic extrusion, the occurrence of deformation of the occlusal plane, and displacement of adjacent teeth. Ankylosed canines were removed, orthodontic treatment of associated occlusion anomalies was performed, and a space was prepared for prosthetic replacement of the missing canine using the implantation method.
The models determined:
- size, shape, position of individual teeth;
- the shape and size of the dentition in three mutually perpendicular planes;
- type of closure of the dentition;
- presence of diastemas, three;
- shape of the lateral incisor;
- the presence of a delay in the change of primary canines.
When studying diagnostic models of jaws, the methods of Pon and Corkhouse were applied.
In patients diagnosed with vestibular retention of canines in the upper jaw, narrowing of the upper dentition in the area of premolars and molars was found in 8 people (53% of cases), expansion - in 7 patients (46% of cases). Shortening of the anterior portion of the dental arch occurred in 12 patients (80%).
In 7 patients with palatal retention of the maxillary canines, shortening of the anterior portion of the dental arch was observed in 92% of cases. Expansion of the dentition in the area of premolars and molars was observed in 19 patients (62%), narrowing in 9 patients (29%).
The data obtained confirm the theory of the occurrence of canine retention in the upper jaw, according to which one of the reasons for the occurrence of vestibular retention of canines is the narrowing of the dentition, and palatal retention is their expansion.
Thus, orthodontic treatment of maxillary canine retention can be carried out at any age in the absence of contraindications and after a detailed diagnostic examination.
The strategy for orthodontic treatment of canine impaction in the upper jaw depends on the location of the impacted canine, its location relative to adjacent teeth, and the condition of the tissues surrounding the impacted canine.
Indications for orthodontic treatment of patients with impacted canines in the upper jaw are displacement in the mesiodistal direction relative to the upper dentition on the vestibular or palatal side, in the absence of resorption of the roots of adjacent teeth and when the angle of inclination of the impacted canine to the midline is no more than 500.
Caries of wisdom teeth and adjacent teeth
Due to the location of wisdom teeth, self-cleaning is poor and cleaning them with a toothbrush is difficult. This leads to the accumulation of plaque and microorganisms around the third molars and their rapid destruction by caries. In addition, wisdom teeth, due to their incorrect position, lead to damage to the teeth adjacent to them.
Since the space between the seventh and eighth teeth cannot be cleaned, the risk of caries increases sharply not only on the wisdom tooth, but also on the second molar next to it. Most often, the cervical region of the second permanent molar is affected, where the incorrectly positioned wisdom tooth rests. This leads to early loss of the seventh tooth.
Rules for retination
Traction takes place in two stages, each of which must be carried out in absolute accordance with the protocol. The process itself is quite labor-intensive and lengthy, so both the patient and the treating orthodontist should be patient. Upon completion of treatment, the patient will undergo a course of rehabilitation.
Locating the anomaly
The main task is to bring the pathology site to the required position. If the stage is successfully completed, it is possible not only to restore the damaged tooth, but also to maintain excellent periodontal condition.
To complete the stage, 2-3 visits to the dentist are needed. The doctor first cuts the periodontal fibers and then returns the root to its correct position. This is followed by a short period of healing and growth of periodontal fibers.
Determining the diagnosis
Diagnosis consists of x-rays and computed tomography (CT). From the x-ray, the doctor will understand whether there is retention, what is the angle of the cut and in what sector is the impacted element located.
CT makes it possible to draw up a detailed plan for further treatment with absolute accuracy.
Important: if the CT scan determines that the root of the impacted canine abuts the adjacent teeth, then they will certainly need to be removed.
Preparation stage
The dentist assumes the following actions:
- The inner part of the root is filled with a pin, which is equipped with a hook at the end.
- A wire spacer is placed on the adjacent teeth.
- Using a special elastic band, the root is attached to the crossbar. The rubber band gradually pulls the tooth out of the gum.
If the aesthetic side of the issue is important to the patient, then the dentist may offer a composite veneer for the period of traction. It will easily hide the defect.
Main part
The protocol for this operation divides the doctor’s actions into two parts: first, a place is prepared in the jaw for a new tooth, then the tooth is moved into the correct position. Most often, the operation involves complete exposure of the crown.
The main stages of the operation:
- Removing the crown of a problematic tooth.
- Installation of a lock on the defective and adjacent teeth.
- Pulling out the canine using an elastic band.
- Extraction of the canine using an elastic arch.
Orthodontic traction of an impacted tooth
This is the second part of long-term treatment. It begins with diagnostics, which consists of a CT scan. This will allow you to determine the angle of germination. The course of further restoration depends on the result.
Before the operation, preparation is necessary. First of all, it is necessary to cure all the teeth in the oral cavity. The doctor gives a painkiller injection.
The essence of the operation is:
- use of orthodontic forceps;
- installing the pin and bracket;
- cementation of the pin;
- installation of elastic fiber and traction;
- cutting the fibers around the tooth (fibrotomy).
After 7-10 days, when everything has healed and the swelling has gone down, the problematic root is moved to the desired position.
Possible complications
Let us warn you right away that if you strictly follow the doctor’s instructions for hygienic care of the oral cavity and teeth, complications almost never occur. However, the process can take much longer and be more painful and problematic if the bone tissue that the orthodontist was able to create during the first stage of treatment is allowed to resorb.
Naturally, after such a problem arises, the only way out is to remove not only the problematic tooth, but those adjacent to it.
About the pros and cons of treatment
The advantages of this type of restorative dentistry include, first of all, the absence of the need to manufacture and install bridges, which significantly saves the patient’s money. In addition, this type of treatment is more aesthetically pleasing. People who do not want to exchange their “native tooth” for an implant insist on tooth extraction.
Disadvantages include exposure of the neck or root of the tooth. Recession is not only considered a defect from a beauty point of view, but can also lead to gum infection.
What is the effectiveness of the method
| Click to sign up for a FREE consultation |
The finale of the restoration marathon occurs after the tooth has been completely pulled out. It is very simple to check how well the doctor managed to cope with the task: you need to show the treated tooth to a stranger. If he doesn’t see the differences between the norm and the once-problem area, then everything is fine!
To increase the operating time of the element, you should regularly visit the dentist’s office and, of course, constantly care for your oral cavity at home.
Tumors and neoplasms associated with wisdom teeth
The most severe consequence of incorrect position and difficult eruption of wisdom teeth is the development of cysts or tumors around them, which leads to the destruction of the surrounding bone tissue and healthy teeth.
In the area of an erupting wisdom tooth, a layer of mesenchymal, immature cells almost always remains, which can cause tumor growth. A small number of these cells make up the tooth follicle or what remains around it after eruption. And, if we quickly get rid of the follicular remains of other teeth during active chewing, then wisdom teeth retain these cells for quite a long time, because are not involved in chewing.
Neoplasms grow asymptomatically and are discovered accidentally during an X-ray examination. They can reach large sizes, destroying jaw tissue, damaging adjacent teeth and anatomical structures.
Wisdom teeth and joint diseases
Since wisdom teeth are often located outside the dentition and, at the same time, do not have an antagonist, dentoalveolar elongation occurs and traumatic nodes appear in the bite, in other words, overload zones. Traumatic nodes disrupt the functioning of the dental system, uncoupling the physiological mechanisms of receptor feedback, thereby leading to diseases of the temporomandibular joints, masticatory muscles, and neurological disorders.
A wisdom tooth growing in the bone tissue causes displacement of the chewing teeth. When the bite has already been formed by this time, a violation of the correct relationship between the dental cusps of the upper and lower teeth occurs, leading to the occurrence of a difficult-to-treat pathology - dysfunction of the temporomandibular joint. The cause of joint pain in the vast majority of patients aged 18-25 years is the rudiments of wisdom teeth growing in the bone.
Deformations of the dentition
The pressure exerted by the erupting wisdom tooth on the dentition when there is not enough space causes crowding of the teeth in the dentition and the development of malocclusion. Aesthetics and smiles are affected mainly in the anterior region, and oral hygiene becomes difficult.
Growing and expanding wisdom teeth are often the cause of reoccurrence of malocclusion after long-term orthodontic treatment. Therefore, it is strongly recommended to remove wisdom teeth before starting orthodontic treatment!
Indications for wisdom teeth removal can be formulated as follows: ANY DISEASE, COMPLICATION ASSOCIATED WITH WISDOM TEETH, AS WELL AS THE RISK OF THESE DISEASES OR COMPLICATIONS IS A DIRECT INDICATION FOR WISDOM TEETH REMOVAL.
Treatment with Damon braces
Orthodontist O.A. Baranova does not welcome the removal of healthy impacted teeth if diagnostics show that the tooth can be returned to its place by restoring correct dental contacts. During treatment with the help of a brace system, a place will be created for the normal position of the semi-impacted tooth.
To correct the bite, the Damon brace system, which is optimal in quality and cost, was chosen. More aesthetic ceramic braces were installed on the front teeth, which are almost invisible on the teeth.
Braces are installed on the teeth:
After installing braces, the patient visited an orthodontist once every two months to monitor and replace the arches. After normalizing the shape of the dentition, the orthodontist connected additional treatment with orthodontic elastics to create correct contacts between the teeth. Correct contacts are a kind of “calling card” of the completed treatment - it is the correct contacts that give the new bite stability, physiology and comfort for the patient. After removing braces, a retention stage is needed to maintain the results obtained. To do this, a wire retainer is attached to the lower teeth, and a mouth guard is made for the upper teeth, which is worn at night.
Wisdom tooth removal: age indications
In world dental practice, it has long been recommended to remove wisdom teeth as early as possible to avoid complications, if there are good reasons for doing so. It is much easier to remove any of the wisdom teeth when their roots are not yet formed, that is, at the rudimentary stage - in early adolescence (late adolescence). The ideal age for removal of wisdom teeth is between 15 and 18 years of age. Then the surrounding bone is also not dense.
The risk of developing complications due to infection and tooth extraction increases in patients over 35 years of age. In patients over 50 years of age, there is a high probability of a wisdom tooth fusing with the walls of the alveolar socket, so the removal of such teeth is more traumatic, and the risk of complications becomes even higher.
Before removing a wisdom tooth, local anesthesia is performed to eliminate any acute pain. It is recommended to remove two wisdom teeth on one side, which is the most rational approach. In the postoperative period, swelling occurs - edema, of varying degrees of severity, which lasts approximately 3 - 4 days. There may be slight discomfort and temporary limitation of mouth opening, so the patient will be able to use the other half of the dentition for a few days while such sensations exist.
In the immediate postoperative period, it is necessary to follow all the doctor’s prescriptions shown in the recommendations after the removal of wisdom teeth.
Prices
Surgical dentistry
| Name | Price |
| Surgery to remove an impacted wisdom tooth in the upper jaw | 9440 rub. |
| Surgery to remove an impacted wisdom tooth on the lower jaw | 11210 rub. |
| Surgery to remove an impacted wisdom tooth (bud) in the upper jaw | 4850 rub. |
| Surgery to remove an impacted wisdom tooth (bud) on the lower jaw | 8340 rub. |
| Surgery to remove an impacted, supernumerary tooth | 8360 rub. |
Make an appointment
An impacted tooth interferes with dental implantation in a 60-year-old patient
Problem: during diagnostics before dental implantation, an impacted tooth (canine) was discovered in the bones of the upper jaw.
Solution: in one operation under sedation, an impacted tooth (canine) was removed, 4 teeth that could not be treated, bone grafting was performed in the area of the impacted tooth to restore bone volume, and Astra Tech dental implants were installed.