Depophoresis is a procedure for complete cleaning and sterilization of pulpless tooth canals using calcium copper hydroxide. The substance, penetrating into the affected area under the influence of current, decomposes any sources of infection (including necrotic pulp remains). Anatomically complex root processes (curved, twisted, branched) deserve special attention. In this case, the technique allows you to treat even roots recommended for removal, increasing the likelihood of saving the tooth several times.
The Mitino Dental Center has everything necessary for high-quality depophoresis. The experience and knowledge of the staff, modern equipment, certified drugs and the comfortable atmosphere of dental offices will not only help preserve your teeth, but will also do this with minimal stress on the body and with maximum benefit for your budget.
REFERENCE! Conventional endodontic treatment with pulp removal occurs without complications in only 30-60% (depending on the level of the clinic), while depophoresis with calcium copper hydroxide ensures success in 95% of cases.
Depophoresis: indications and contraindications for the procedure
Main indications for depophoresis:
- dental canals of complex shape (curved, deformed, with an extensive network of microtubules);
- the presence of residual pulp tissue in the canals (especially if gangrenous areas are present);
- the need to correct poor-quality fillings;
- the presence of foreign bodies in the dental canals;
- channels that are too wide or too narrow;
- multiple microholes in the tissue structure;
- radicular cysts and granulomas (the method allows you to treat the problem non-surgically, directing a suspension of calcium-copper hydroxide not only from the smallest nooks of the root system, but also into the cavity of the cyst, completely clearing it of pathogens and damaged tissue);
- standard depulpation procedure (for high-quality disinfection).
Several sessions of depophoresis may be needed to achieve results.
REFERENCE! During the process of depulping canals of complex shape, the tip of the pulp extractor may break off. A stuck fragment often cannot be removed without destroying the root tissue. Root canal depophoresis successfully solves the problem by completely sterilizing the fragment itself and the space surrounding it, after which the foreign object can remain inside the tooth without creating a threat of infection.
In addition to the effect of intensive sterilization, calcium-copper hydroxide ions contribute to the restoration of bone tissue. The effect of electric current stimulates the processes of osteocement synthesis, due to which the root canals are quickly sealed, the tissues restore their structure, and the tooth becomes stronger. The list of contraindications to depophoresis is small. These are mainly pregnancy, individual intolerance to the active substance (possible allergy to copper ions) and the acute phase of periodontitis. The reason for failure may be old silver pins in the tooth (risk of severe corrosion with the release of toxic substances).
IMPORTANT! A risk factor during depophoresis is any metal crowns, inlays and brackets, so the dentist must remain extremely careful and avoid contact of a metal element of the dental structure with one of the electrodes of the device.
Research by scientists has shown the effectiveness of depophoresis not only in adults, but also in pediatric dentistry. In the presence of formed roots, the procedure strengthens the weakly mineralized tissues of the dental canals and prevents early tooth loss (in childhood, loss can lead to improper development of the masticatory apparatus and jaw structure as a whole).
Treatment of cysts with calcium preparations in dentistry
Given the constant and continuous development, modern dentistry successfully combats most diseases of the teeth, gums and the oral cavity itself. One of these problems is a dental cyst.
Tooth cyst
is a disease expressed in the formation of an inflammatory capsule with dense walls, inside of which there is often a mass consisting of bacteria and dead cells. This neoplasm appears in the gums around the root of the tooth, and in the absence of timely and targeted treatment, it can cause undesirable consequences. Over time, the size of the cyst increases, gradually destroying the surrounding bone tissue.
The occurrence of a dental cyst is usually associated with an infection; less often, the cause of the disease can be an injury that can be obtained in a completely trivial way - for example, cracking nuts with your teeth.
To determine the presence of a dental cyst, an X-ray examination of the affected area of the jaw is performed. Most often, the patient does not even suspect the presence and development of a cyst, since it passes painlessly
without causing any discomfort. Only during exacerbation does profuse tissue inflammation occur, accompanied by purulent formations and “flux.”
For successful treatment of the disease, its timely diagnosis is very important. Modern dentistry uses two methods to treat inflammation: surgical and therapeutic.
For therapeutic treatment of cysts, the inflamed tooth is drilled and the root canal is disinfected using a special solution. However, the result of these manipulations is not always successful, therefore, six months after the treatment, a re-examination with X-rays will be required to exclude re-inflammation.
Treatment of cysts with a more modern therapeutic method used in dentistry is the use of depophoresis
.
During the treatment, calcium is used, or rather copper-calcium hydroxide, which is injected into the canal of the diseased tooth. At the same time, the tooth is exposed to a weak electric current - for better penetration of the suspension into the cyst and its removal. After three sessions of depophoresis, the tooth is filled. Also, in the treatment of dental cysts, preparations based on calcium and iodine are used ( Metapex
,
Calasept,
etc.).
When using the surgical method in dentistry, the cyst is removed along with the damaged part of the tooth root (cystectomy), or the entire root and part of the tooth above it are removed (hemisection), subsequently placing a crown on it. The site of the resulting defect in the bone tissue is filled with bone material.
Equipment for depophoresis
The active substance is delivered to the affected area using special equipment. At the moment, highly specialized devices for depophoresis are produced solely by the company HUMANCHEMIE, which produces only one model - ORIGINAL II. The device is officially approved by the developer of the method and has a full functional set for high-quality and convenient performance of the procedure in a modern dental clinic:
- sets the duration of the session;
- sets the current strength;
- controls the stage of the procedure (taking into account the current strength and time).
All other examples of devices are complex devices designed to perform several dental procedures.
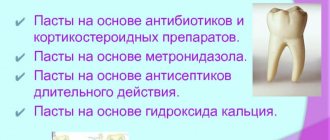
In addition to technology, to perform the procedure efficiently, you will need a set of specific drugs:
- Disinfectant compositions are represented by various suspensions based on copper and calcium hydroxide - cupral. Various versions come in the form of a powder (diluted in water to form a solution for depophoresis) or a paste (used to temporarily seal canals). Taking into account the main active ingredient, the depophoresis technique is also called cupral-depophoresis.
- Atatsamite is a powder preparation of plastic bactericidal cement for final filling of sterile dental canals.
REFERENCE! In some cases, calcium hydroxide is used to disinfect canals, but a mixture of calcium and copper hydroxides increases efficiency tenfold, which makes the use of cupral relevant as the main drug for depophoresis.
Beneficial properties of calcium
Preparations containing calcium have an antibacterial effect. Most dental diseases are caused by bacteria that actively multiply in an acidic environment. But an alkaline environment, on the contrary, kills them.
Calcium helps create an alkaline environment in the tooth cavity that is unsuitable for bacterial activity.
To obtain a filling paste, calcium hydroxide powder is diluted with saline solution. Interaction with liquid leads to the release of hydroxyl ions, which kill pathogenic bacteria.
How is depophoresis performed in dentistry?
The preparatory stage includes radiography of the tooth. The number of roots, the length and shape of the dental canals, the presence and location of infection are assessed. The more detailed the diagnosis, the higher the effectiveness of treatment.
The depophoresis procedure is performed only on “dead” teeth, so preliminary devitalization (pulp removal) will be required.
The depophoresis procedure itself consists of 2-3 sessions, which are carried out with a break of a week. Sequencing:
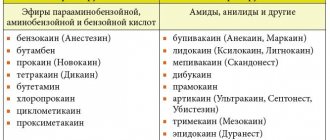
- Local anesthesia is performed using application and infiltration anesthesia.
- The tooth is opened to gain access to the canals and the cavity is expanded to the required size.
- The channels are filled with calcium-copper hydroxide.
- Electrodes are installed (a negative charge is inserted into the dental canal to a depth of 8 mm, a positive charge is placed on the inside of the cheek near the problem tooth).
- Electric current is applied, gradually increasing the power until the patient feels warmth in the affected area. On average, the current level reaches 2 mA - this is enough to start the process of electrophoresis of copper and calcium ions into the adjacent tooth tissue.
- The procedure is completed by washing with distilled water (or a 10% hydroxide solution) and temporarily sealing the canal with a paste, again, with calcium hydroxide.
The whole job takes just over 5 minutes. 1 channel is processed per session.
ATTENTION! Simultaneous depophoresis of several channels is undesirable. This will lead to uneven distribution of current and a decrease in the quality of the procedure.
The last session is the final one. It involves re-processing with disinfection of the smallest tubules and sealing the tooth with a plastic cement composition with an antibacterial effect. Finally, the dentist installs a filling, which can be permanent or temporary (with subsequent replacement with an inlay).
For complete safety, a control x-ray of the tooth is taken.
ATTENTION! In case of increased tooth sensitivity (acute pain during a depophoresis session), the breaks between sessions can be increased to 2-3 weeks.
Procedure for filling teeth with calcium
A filling filled with calcium is temporary and, after a period determined by the doctor, changes to a permanent
one. Installation of a calcium filling involves several stages:
- The doctor mixes calcium powder with distilled water and glycerin to obtain a homogeneous paste.
- Before filling, the doctor cleans the root canal and treats it with special preparations.
- Using a channel filler, the resulting paste is introduced into the recess
- To ensure that the substance adheres tightly to the walls of the canal, it is compacted with a pin, and then the hole is hermetically sealed.
As mentioned above, a calcium filling is temporary. How long it will stay in the tooth is decided by the doctor, based on the specific clinical case. After the prescribed period has expired, the dentist removes the temporary filling and places a permanent one in its place.
How does calcium work?
Staying in the canal for a certain time, calcium completely kills bacteria living in the tooth
After entering the root canal, the calcium mixture begins to interact with the tissues and microflora of the tooth. The oxide penetrates into the dentin and pulp. When the substance remains inside the canal for a long time, it completely kills the bacteria living in it. After such exposure, the doctor can safely carry out further treatment or fill the canal.
Mechanisms of antimicrobial activity
Most endodontic microorganisms cannot survive in the highly alkaline environment provided by calcium hydroxide (Heithersay 1975). Since the pH of calcium hydroxide is about 12.5, the bacterial species commonly found in contaminated root canals can be eliminated after a short period of direct contact with this substance (BystroÈm et al., 1985). The antimicrobial activity of calcium hydroxide is associated with the release of hydroxyl ions into the aquatic environment. Hydroxide ions are free radicals and have high oxidizing capacity, exhibiting high reactivity, reacting with a number of biomolecules (Freeman & Crapo 1982). This reactivity is high and non-selective, so free radicals rarely diffuse out of the localized area. Its lethal effects on bacteria are likely due to the following mechanisms:
Damage to the bacterial cytoplasmic membrane
The bacterial cytoplasmic membrane has important functions for cell survival, such as:
(I) Selective permeability and permeability