One of the most important problems of medical institutions is nosocomial infections. Infection can occur during treatment and diagnostic procedures, as well as naturally - through household contact or airborne droplets. We do not undertake to estimate the frequency and volume of nosocomial infections, but we can talk in detail about those disinfectants that are used in modern medical practice.
In order to prevent the spread of nosocomial infections, modern chemical agents are used to disinfect hospitals based on chlorine, hydrogen peroxide, alcohols, aldehydes and other disinfectants. Their active use for disinfection of premises, medical instruments, and equipment reduces the risk of infection to almost zero. However, the very concept of “disinfection” is somewhat broader than a list of disinfectants and methods of their use. There are other methods of disinfection other than chemical disinfection.
Disinfection methods
Disinfection is a list of chemical, mechanical, and physical manipulations specifically designed to destroy pathogenic agents that cause various diseases in humans and animals.
Disinfection is carried out using the following methods:
- boiling;
- ultraviolet irradiation;
- air ozonation;
- steam, air sterilization;
- treatment with chemical disinfectants.
Depending on the time and place of disinfection, disinfection is divided into:
- Preventive disinfection - carried out if the exact source of infection cannot be identified or does not exist, to protect against possible infection.
- Focal disinfection - performed when the source of infection is identified.
Focal disinfection includes: current treatment, which is carried out in the presence of the patient, and final treatment, which is carried out after the patient leaves (discharge or death) to eliminate foci of the pathogen.
All medical instruments, equipment, surfaces and objects with which the patient has been in contact are subject to chemical disinfection or another disinfection method. Disinfection of surgical instruments followed by sterilization is mandatory.
Disinfectants
Disinfectants used in medicine are classified according to their composition and purpose. They have varying degrees of antimicrobial activity, toxicity, and influence on the object they treat. The following modern disinfectants are officially approved for use in medical institutions:
- Based on chlorine: Chlormisept economy. These products are used to disinfect medical instruments made of plastic, rubber, and glass. Chlorine-containing preparations have low toxicity, but cause corrosion of metals. Among the disadvantages is the presence of the smell of chlorine.
- Hydrogen peroxide solutions: Alphadez oxy. They have low toxicity, are odorless, and are used to disinfect instruments made of rubber, plastic, and glass. Does not have a fixing effect on organic matter.
- Aldehydes: Alfadez forte, Alfadez ortho. They are used for disinfecting endoscopes and related instruments, as well as for cleaning premises and washing equipment. They have high activity against many pathogenic microbes. Aldehyde agents are often used for HLD and chemical sterilization, but they have a fixing effect and therefore require careful pre-cleaning and disinfection.
- Alcohol-containing antiseptics: Miroseptic, Ecobriz antiseptic, Estilodez antiseptic. Used as an antiseptic for treating the skin before injection, for disinfecting the skin and surgical fields.
All objects in contact with blood and in contact with the wound surface are subject to mandatory disinfection. Sterilization of medical instruments is carried out after their preliminary disinfection using chemical solutions or steam sterilization.
Use of new technologies during root canal disinfection
The role of microorganisms as the main etiological factors in the pathogenesis of pulp and periapical tissue pathologies has been proven in many clinical and scientific studies. Thus, the main goal of endodontic treatment is precisely the disinfection of the root system, which involves the elimination of all microorganisms and microbial components from the root canal space, as well as the implementation of appropriate measures aimed at preventing re-infection of the endospace both directly during and after iatrogenic interventions. A similar result can be achieved using chemical-mechanical sanitation using different root canal protocols.
Sodium Hypochlorite
Sodium hypochlorite (NaOCl), known for its antibacterial properties and ability to dissolve organic tissue, is probably the main endodontic irrigant in modern times. Typically, the solution is used during the canal instrumentation phase to maximize its exposure time within the root space, and, as far as possible, to minimize its chemical interaction with other irrigating agents. According to research, the effectiveness of sodium hypochlorite directly depends on its concentration, temperature, pH of the solution and storage conditions. Concentrated solutions (5-6%) heated to 45-60 °C or more are characterized by increased histolytic properties, although it should be remembered that irrigants of such concentrations are much more dangerous in cases of their removal beyond the periapical space. In order to reduce the risk of such complications, it is recommended to use specially designed endodontic needles, as well as an injection technique for introducing the solution without excessive hydraulic pressure.
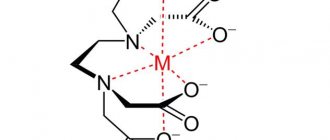
EDTA
The main disadvantage of NaOCl is the inability to remove the smear layer, which is why sodium hypochlorite is recommended to be combined with EDTA (ethylenediaminetetraacetic acid). EDTA has the ability to degrade the inorganic component of intracanal debris and is typically used at a concentration of 17%. At the same time, EDTA reduces the antibacterial potential and solvent activity of NaOCl, therefore it is advisable to use hypochlorite during mechanical treatment of the canal, and EDTA after this for 2 minutes in order to completely remove inorganic particles and the formed smear layer from the walls of the endospace.
Ultrasonic activation of NaOCl
The use of ultrasound both during and after root canal preparation is a mandatory step to improve the effect of endodontic disinfection. The frequency range used in an ultrasonic device ranges from 25 to 40 kHz, with the effectiveness of ultrasound itself during irrigation determined by its ability to produce cavitation and acoustic flow effects. In this case, the cavitation area is limited to the area of action of the top of the instrument, while the acoustic flow is recreated along the entire length of the file, and has a much more significant impact on the process of root canal disinfection. Under the influence of ultrasound, bubbles with negative and positive pressure are formed in the structure of the contacting liquid. Due to their instability, the bubbles burst, collapse and cause implosion, similar to vacuum decompression, while a certain energy of the substance is released, which forms the same washing effect of the irrigant. It has been proven that ultrasonic activation of NaOCl significantly increases the effectiveness of its use during endopreparation, both due to the increase in the magnitude of the fluid flow itself, and due to improved antibacterial and solubilizing abilities, thereby providing better removal of organic and inorganic particles from the walls of the root canal. It is reasoned that 30-60 second ultrasonic activation of hypochlorite in each of the root canals, three 10-20 second cycles, is sufficient, and in each cycle it is advisable to use a new portion of the irrigation solution (photo 1-2).
Photo 1: Ultrasonic activation of a solution with a passive file.
Photo 2: Ultrasonic activation of a solution with a passive file.
As for the combination of ultrasound and EDTA, this approach is less effective than with hypochlorite, although the removal of the smear layer is also noticeably faster and quite reliable. In addition, the use of ultrasound and hypochlorite also helps to get rid of abrasions formed during the instrumental treatment of the canal, even in the most inaccessible places, therefore, the feasibility of such a combined technique has been more than proven. To implement this technique, all that is required is the use of a special root needle, activated by ultrasound, while injecting an irrigant solution into the root canal space.
Chlorhexidine
The use of 2% chlorhexidine, characterized by a wide spectrum of action and sufficient substance, is extremely desirable at the final stage of chemical-mechanical treatment of the root canal after irrigation with NaOCl and EDTA, especially if there was previously a chronic infection in the endospace. However, it should be remembered that the direct interaction of hypochlorite and chlorhexidine produces chemicals, the precipitation of which can provoke tooth discoloration, not to mention their potential mutagenic effect. Therefore, it is prohibited to inject chlorhexidine into the root canal if there is hypochlorite in it, or after it, and indirect contact of these substances can be minimized by first rinsing the canal cavity with alcohol, saline or distilled water.
Activation systems
Mechanical treatment of the root canal helps to significantly reduce the number of bacterial contaminants in the structure of the endospace even without the additional use of any chemicals, but such an approach is simply not able to provide a sufficiently effective and most complete cleansing of the root system. Likewise, the irrigative effect of solutions cannot ensure complete disinfection of the canal without appropriate mechanical support. Consequently, the issue of choosing mechanical activation methods as an integral part of endotherapy protocols remains quite relevant in our time, given the wide range of studies that have been carried out to study this issue.
Manual activation methods
The simplest method of mechanically activating irrigants is their manual mixing, which can be done using various adapted systems. Firstly, you can simply move the passive endodontic file up and down, and this will ensure more effective delivery of the irrigant solution to particularly hard-to-reach areas, and will also help get rid of air bubbles formed in the irrigant. In addition to the file, you can also use a gutta-percha pin selected according to the working length, although there is still insufficient evidence that this technique is more effective. For this purpose, it is, of course, better to use gutta-percha pins with increased taper than standard samples (with a taper of 0.02). Additionally, you can use endodontic brushes and special needles with small bristles on their surface, which, among other things, provide much more effective removal of the smear layer, and, therefore, can be recommended as an additional tool when irrigating with an EDTA solution, which will help improve the quality of treatment the root canal as a whole.
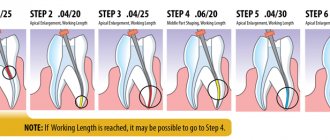
Machine activation of irrigants
The evolution of hand-held endodontic systems has provided instruments that can rotate through mechanical movement in the head of the dental handpiece, thereby allowing the irrigant solution to be slowly mixed within the root canal space. For the coronal and middle third of the root, so-called rotary brushes can be used, while for the apical third it is more effective to use plastic files with a smooth or modified surface, which can be adjusted to the working length of the root canal. In general, taking into account the results of many studies conducted, it can be summarized that the use of machine irrigant activation systems is more effective than conventional manual mixing of a disinfectant solution, but less effective compared to other methods available in practice, such as continuous irrigation, irrigation with a sonic nozzle, laser etc.
Continuous irrigation during canal treatment
This approach is one of the most innovative on the dental market, and involves the use of a specific endodontic instrument with an abrasive surface, which not only expands the canal through vibrating movements, but also ensures the delivery of the irrigating solution through the structure of the instrument itself. This system is particularly promising for cleaning complex anatomical areas of root canals such as isthmuses, or their varieties - oval canals or C-shaped canals. The low cutting ability of this endodontic system limits its effective independent use during endospace treatment, but at the same time makes it highly suitable as an alternative method for final cleaning of the root system after the classical protocol of mechanical and chemical disinfection. This concept was originally developed for mechanical instruments for sonic and ultrasonic devices, but due to its low dissection ability, it had to be abandoned over time.
Sound activation
The latest sonic irrigant activation systems use smooth plastic tips of various sizes to effectively clean the endodontic space, remove the smear layer and treat more lateral root branches. One recent modification of the approach is the use of a syringe with sonic vibration, which provides both delivery of the irrigant solution and its immediate activation. Sound activation of an irrigant differs from ultrasound in that its operating principle is based on the use of lower frequencies in the range of 1-6 kHz, therefore these systems are characterized by slightly lower efficiency than their ultrasonic counterparts.
Apical irrigation using the negative pressure principle
For successful endodontic cleaning, the irrigant must be in direct contact with both the microorganisms of the root canal and with all root walls, especially in the hard-to-reach apical third. To ensure fluid flow along the entire length of the channel and sufficient hydrodynamics of the solution, researchers proposed the use of an apical irrigation protocol based on the negative pressure principle, which allows delivery and removal of the irrigant almost simultaneously. The system consists of a macro-cannula for the coronal and middle parts of the root, and a micro-cannula for the apical third. The cannulas are connected to a syringe for irrigation and a suction system integrated with the dental unit (photo 3).
Photo 3: Irrigation system with apical negative pressure principle to improve the efficiency of endodontic treatment.
During irrigation, a nozzle connected to a syringe ensures the injection of an irrigation solution into the pulp chamber, while the risk of overfilling the endospace with a chemical agent is automatically controlled. At the same time, a cannula placed in the canal space, on the contrary, ensures the removal of the irrigation solution through the aspiration system, and thus a mechanism is implemented for a constant and continuous flow of a new irrigation solution along the entire length of the tooth root, which does not provoke the risk of possible extrusion of a chemical agent into the post-apical space. A large number of studies have proven the superiority of using this endodontic system in terms of the quality of removing debris from the canal space, providing access to particularly difficult areas of the root, as well as the most complete cleaning of the apical third of the canal. From a clinical point of view, apical negative pressure irrigation systems can be effectively integrated with ultrasonic endo-cleaning methods, since their mechanism of action is completely different. The combined use of these approaches will provide opportunities for more complete cleaning of root spaces, especially in the apical third and hard-to-reach areas of the root.
Laser activation
The issue of interaction of the laser with the irrigant inside the root canal is a rather relevant aspect of practical endodontics. Moreover, this concept has two subsections at once: firstly, laser activation of a chemical agent, and secondly, a photoacoustic flow initiated by the activation of photons. The mechanism of interaction between the laser and the irrigant is as follows: NaOCl has the ability to actively absorb light, this, in turn, leads to the evaporation of the irrigant solution and the formation of steam bubbles, which expand and burst, initiating the secondary effect of cavitation. The principle of photodynamic flow is largely based on the role of Er:YAG power, which is quite sufficient to initiate the occurrence of shock waves in the irrigant solution. The photomechanical phenomenon of the laser action on the irrigant solution is also due to the fact that the activation of the solution, as well as the influence of the peak light power, occurs in a limited space for a short period of time of about 50 μs, sufficient for the propagation of the pulse. But some studies claim that the antibacterial effect of laser-activated and non-laser-activated hypochlorite is almost the same, and the reduction in the number of bacterial contaminants occurs to almost the same extent. In addition, the results of individual studies also indicate that laser activation of hypochlorite is not sufficient to ensure the removal of bacterial biofilm from the apical third of the root canal and from the thickness of the dentinal tubules. However, more recent studies demonstrate that the use of a laser ensures that most bacterial structures enter a specifically charged state in which they become inactive, which is extremely important for reliable cleaning of the apical third of the root canal.
Additional disinfection systems
In addition to the above-mentioned methods of root canal disinfection, practical endodontics continues to effectively develop in the direction of increasingly effective and improved approaches to complex root canal treatment, using not only various chemical agents, but also modern technologies.
Photoactivated disinfection
This approach is based on the principle that the photosensitizer inherent in the irrigant solution has the ability to bind to bacterial membranes, and after activation by a light wave of a specific length, free singlet oxygen is formed, provoking the destruction of the bacterial cell wall with which the photosensitized molecule is associated. Extensive laboratory studies have proven that neither the laser nor the photosensitizer alone produces any effect on the bacterial cell or normal human tissue, but only when used in combination do they demonstrate their broad disinfecting properties. The endodontic photoactivated disinfection system was developed based on the combined implementation of the specific characteristics of photosensitizers and a light source adapted for this purpose. First, the photosensitizer attacks the bacterial cell, after which it “sticks” to its membrane and binds closely to its outer surface. When exposed to a certain radiation, the photomolecule absorbs energy and then releases it in the form of oxygen, which turns into its highly active chemical form. The latter is the final weapon that has a detrimental effect on microorganisms. The advantage of photoactivated disinfection is that it is effective not only against bacteria, but also against other microorganisms such as viruses, fungi and protozoa. The affinity of the photosensitizer for the cells of the body is much less than for bacteria, so it can be summarized that this method is not toxic or dangerous in relation to healthy human tissues. The clinical protocol of this method is as follows: the photosensitizer is introduced into the root canal to its full working length using an endodontic needle, after which it is left in the endospace for 60 seconds, allowing the solution during this time to come into contact with microorganisms and penetrate as deeply as possible into the thickness of the bacterial film ; after this, an endodontic attachment is inserted over the entire working length of the canal, through which a light flux is supplied for 30 s in each of the root canals (photo 4).
Photo 4: Disinfection of the canal using a directed light beam.
This method has proven its effectiveness in laboratory studies aimed at studying the level of reduction of bacterial contamination in specially seeded channels with a high concentration of microorganisms. An important aspect of this algorithm is the correct introduction of the photosensitizer and providing sufficient time for the latter to come into contact with microorganisms, otherwise the photosensitization effect will be reduced to zero. In addition, the advantage of photosensitization is that it is equally effective against individual bacteria and their groups in the irrigator solution, and against the biofilm formed on the canal walls. Research is currently underway to improve this approach using bioactive excipients and nanoparticles. So far, photoactivated disinfection cannot be recommended as an alternative to the classical approach, but can be considered a high-quality and fairly successful addition to standard root canal disinfection protocols.
Laser
One of the main disadvantages of current endodontic irrigants is that their bactericidal effect is limited mainly to the space of the main root canal. In practical endodontics, it has been proposed to use several types of lasers for disinfection of the endospace: diode, carbon dioxide, neodymium, erbium. The bactericidal effect of a laser depends on the characteristics of the light wavelength and its energy, and, among other things, is also ensured by the thermal effect. The thermal effect induced by the laser provokes changes in the bacterial cell wall, which, in turn, causes changes in osmotic gradients up to the death of the cell itself. Some studies have concluded that laser irradiation is not an alternative, but rather a possible addition to existing endodontic root canal preparation protocols. Given that the laser energy is directed along the optical fiber, different delivery systems have been developed to distribute it more three-dimensionally: some of them consist of a main tube that has lateral holes that allow the laser radiation to change direction from strictly vertical to more lateral. Such modifications allow the laser to reach bacteria even in the thickness of the dentinal tubules, but be that as it may, the laser itself does not provide such a total cleaning of the root wall from bacterial biofilm as, for example, sodium hypochlorite. In addition, the widespread use of lasers powerful enough for endodontic disinfection is not yet available in wide dental practice due to a number of objective reasons.
Ozone
Ozone is an unstable form of oxygen, easily soluble in water and sufficiently reactive to oxidize microbial cells. It has been suggested that ozone has sufficiently high antimicrobial effectiveness without causing drug resistance in the body. However, the results of existing studies regarding its effectiveness against endodontic pathogens are quite contradictory, especially in relation to biofilm, but are not comparable to the unique capabilities of sodium hypochlorite.
Alternative antibacterial systems
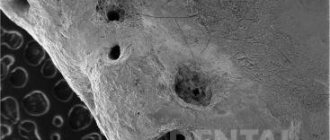
Nanoparticles
Nanoparticles are microscopic particles ranging in size from 1 to 100 nm, which have unique anti-inflammatory and antibacterial properties, and at the same time cause much less resistance in the body compared to traditional antibiotics. For example, nanoparticles of magnesium oxide, calcium oxide or zinc oxide have bacteriostatic and bactericidal properties: they generate reactive oxygen species, which are responsible for the antibacterial effect through electrostatic interaction between positively charged nanoparticles and negatively charged bacterial cells, which results in the accumulation of large the number of nanoparticles on the surface of the bacterial cell membrane with a subsequent increase in its permeability. The latter ultimately provokes the death of the cell itself. Nanoparticles synthesized from silver, copper oxide or zinc oxide powders also have fairly high antimicrobial activity. In addition, nanoparticles can change the chemical and physical properties of dentin, thereby reducing the adhesion strength of bacteria to the root canal wall, thus limiting the opportunities for re-contamination of microorganisms and the formation of a new biofilm structure. In any case, the possible success of using nanoparticles in endodontics will significantly depend on how the mechanism of their delivery to the most inaccessible areas of the root canal will be modified.
Bioactive glass
Recently, bioactive glass or bioactive glass ceramics have increasingly become the subject of significant interest in the endodontic industry, given their fairly high antibacterial properties. But the results of studies on this issue are so far contradictory enough to formulate any clear conclusions.
Natural plant extracts
Among natural plant extracts, substances containing polyphenolic molecules can be obtained, which are often used for long-term storage of food products. Although some of these compounds have little antibacterial effect, some still demonstrate significant ability to reduce biofilm formation, although the mechanism by which this occurs is still difficult to fully explain.
Tool-free processing methods
Lussi was the first to offer a tool-free root canal treatment technique. The author's method did not involve expansion of the root canals or other mechanical cleaning, except for irrigation of the endospace with a low concentration NaOCl solution, followed by removal of the irrigant using a vacuum pump, as well as the use of an electric piston, which recreated areas of variable pressure inside the canal itself. The latter, in turn, caused the effect of implosion of the formed bubbles and the corresponding hydrodynamic turbulence, which contributed to the penetration of NaOCl into the lateral root branches. At the end of such treatment, the channel was filled with cement, but given the low efficiency of this approach, it never found its widespread use. More recently, a new approach has been introduced using a broad spectrum of sound waves propagating through the irrigant structure to effectively remove pulp tissue, endodontic debris and existing microorganisms. One study even proved that this technique provides better processing results than the classic algorithm for chemical-mechanical cleaning of the root space. But to justify the use of this technique, a number of additional studies are required to study the possibilities of the proposed approach as a minimally invasive technique that does not require instrumental preparation of the endospace.
conclusions
According to modern concepts, endodontic pathology is essentially an infectious lesion provoked by a complex of bacteria and, in particular, by the action of their organized structure in the form of a biofilm. From a biological point of view, endodontic treatment should be aimed specifically at eliminating microorganisms and preventing the risk of re-contamination, but, unfortunately, the root canal system with its anatomical features is a rather complex environment, the elimination of bacteria from which is a very difficult clinical task. Chemical-mechanical treatment of the root canal consists of mechanical cleaning of the endospace with parallel irrigation with antibacterial agents. Improvements in the mechanical stage of endodontic preparation have provided new opportunities for improved approaches to creating endodontic space with much fewer procedural complications. In turn, root canal irrigation can also be carried out using a significant amount of chemicals, however, even despite modern advances, problematic issues in endodontics remain aspects of irrigant delivery to the apical third of the root, the most effective activation of the solution, and the predicted reduction in the level of contamination, especially in hard-to-reach areas. areas of the root system, the solution of which will allow achieving the most successful and long-term result of complex endodontic intervention.
Authors: Dr. Gianluca Plotino, Gianluca Gambarini, Dr. Nicola M. Grande