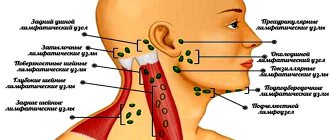
Lymph nodes are located shallow under the skin on the neck, under the arms, and in the groin. They increase in children most often on the neck during infections: colds, sore throats, etc. If the lymph nodes do not decrease after recovery from the infection, remain dense or continue to enlarge, the child should be examined by a pediatrician. You should not feel your child’s lymph nodes more than 2 times a day - this can make them even more swollen and painful.
THE DOCTOR'S CONSULTATION
See your doctor if your lymph nodes are enlarged:
- in a child under 12 months
- longer than 7 days
- and increased temperature
- several groups
- continue to enlarge or the surrounding skin changes
ATTENTION!
If the lymph nodes are enlarged in a child younger than 12 months, it is necessary to have the child examined by a pediatrician.
| ASK YOURSELF A QUESTION | POSSIBLE REASON | WHAT TO DO |
| Does your child have enlarged lymph nodes in the front and sides of the neck? Fever, stuffy nose, runny nose, sore throat, sneezing, dry cough? | ARVI (cold); angina; Infectious mononucleosis | Call a doctor. Give paracetamol to reduce fever. As your child's condition improves, check 1 to see if the lymph nodes are getting smaller. If the increase persists for more than 7 days, contact your pediatrician again (see also Fever, Runny nose) |
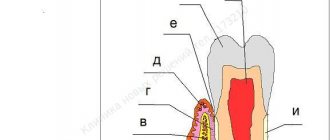
| Are the lymph nodes of the lower jaw enlarged? Does your child complain of pain in a tooth or anywhere in the mouth? | Inflammation of the tooth, gums, cheeks | Contact your pediatric dentist . He will examine the child and prescribe treatment (see Mouth pain) |
| Are the lymph nodes only enlarged in the groin or under the armpit? Is there swelling, redness, or tenderness in an arm or leg on the same side? | Infection (possibly bacterial) | Consult your pediatrician for advice . He will examine the child and prescribe treatment, which may include antibiotics. |
| Did swollen lymph nodes occur while taking medication, particularly antiepileptic drugs? | Side effect of the medicine | Make an appointment with your pediatrician . He will adjust the appointment |
| Did enlargement and tenderness of the lymph nodes occur after the child was scratched by a cat? Slightly elevated temperature, headache? General malaise? | "Cat Scratch Disease" | Contact your pediatrician . He will examine the child and prescribe treatment. Paracetamol can be given to reduce the temperature (see Cuts and abrasions) |
| Are the lymph nodes directly above the collarbone enlarged? Are the lymph nodes of other groups enlarged? | Infection; another disease requiring immediate diagnosis and treatment | Contact your pediatrician immediately . He will examine the child and prescribe the necessary examination and treatment. |
FOR INFORMATION
Lymphoid organs
Lymphoid organs are the basis of the body's defense system in the fight against pathogenic bacteria and viruses. It consists of the spleen (the largest organ) and groups of small lymph nodes connected by lymphatic vessels through which lymph flows. Lymph nodes, located in the neck, armpits, groin and many other places, act as a barrier to the spread of germs. Lymph is a fluid containing large numbers of white blood cells called lymphocytes. Lymphocytes are produced in the bone marrow, then pass through the spleen and lymph nodes and then gain the ability to recognize foreign cells and microbes. Lymphocytes participate in the body's immune defense reactions. They produce antibodies that destroy or render harmless microbes; Antibodies remain in the blood for a long time and when the same microbes re-enter, they are able to fight them. When microbes attack the body, the lymph nodes become noticeably enlarged, as there are more lymphocytes and they actively produce antibodies.
Child's age
Lymph nodes are usually not identified/palpated in newborn babies due to their small size and soft consistency.
In young children, cervical, axillary and inguinal lymph nodes can be identified.
In children under 5 years of age, during a routine examination by a pediatrician, palpable lymph nodes are detected in 44% of cases, in children with any diseases - in 64% of cases [2].
The presence of palpable lymph nodes is not always a manifestation of any pathology. And also palpable formations may not be lymph nodes at all, but, for example, a congenital anomaly (cyst, hygroma).
Normally, lymph nodes in children grow until 8-12 years of age, then decrease slightly [3].
What diseases cause lymph nodes to enlarge?
Most often, enlargement of the cervical lymph nodes in children occurs with:
- colds - acute respiratory viral infections, acute respiratory infections, influenza;
- purulent-inflammatory diseases of the oral cavity and pharynx - sore throat, scarlet fever, tonsillitis and others;
- diseases of the gums and teeth - caries, stomatitis, gingivitis, as well as teething;
- decreased general immunity after illness;
- immune system disorders;
- diseases of the ENT organs - otitis media, inflammation of the auditory nerve, boils in the external auditory canal;
- inflammation of the tonsils with tonsillitis, sore throat, pharyngitis.
Lymph node size
Often the exact size of the lymph nodes is difficult to determine by touch. The size largely depends on the specific group of lymph nodes.
In principle, any lymph node, if it is detected by touch, is already considered enlarged. However, some groups of lymph nodes filter lymph from large areas of the body and can be detected even in healthy children [4].
Thus, in children, cervical, occipital, posterior ear, axillary lymph nodes can be palpated - no more than 0.5 cm - cervical, submandibular - no more than 1 cm, inguinal - no more than 1.5 cm. Occipital and posterior ear lymph nodes can more often be detected in small children, cervical and inguinal - in children over 2 years old.
Lymphadenopathy is a condition characterized by an increase in lymph nodes in size and/or quantity and/or a change in their consistency.
According to many observations, the incidence of enlarged lymph nodes depending on age is [4]:
| Occipital | Posterior ears | Submandibular | Cervical | Absence | |
| 0—6 months | 32% | 13 | 2 | 2 | 62 |
| 7-12 months | 26 | 13 | 3 | 26 | 52 |
| 1 year | 10 | 7 | 18 | 28 | 52 |
| 2 years | 8 | 6 | 20 | 45 | 32 |
| 3 years | 7 | 0 | 26 | 33 | 41 |
| 4 years | 0 | 0 | 25 | 55 | 35 |
| 5 years | 0 | 5 | 21 | 63 | 26 |
Normal size of lymph nodes
It is believed that lymph nodes should be up to 1 cm in diameter (but definitely not exceed 2 cm [2]), inguinal - up to 1.5 cm, ulnar, behind the ear - up to 0.5 cm [5,6].
These sizes are not strict, especially for children in the first years of life (babies are just encountering different antigens and developing their immunity, more details in the article “Causes of enlarged lymph nodes”).
When assessing lymph nodes, it is also necessary to evaluate their consistency, mobility, shape, density, and changes in the skin over the surface.
The concept of “lymphoma” unites many diseases that differ in their clinical manifestations, course and prognosis. All lymphomas are divided into two large groups: Hodgkin lymphoma (HL) and non-Hodgkin lymphomas. The first is named after the scientist Thomas Hodgkin, who first described it in 1832 (and the name itself was introduced by WHO in 2001). Synonyms: lymphogranulomatosis, Hodgkin's disease. HL became the first clinically and morphologically recognizable malignant tumor and the first malignant disease in which patients had a chance of complete cure if only radiation therapy was available to the oncologist. Today, successes in the treatment of HL are among the bright victories of oncology.
Alesya Markovets, researcher at the clinical research laboratory of the Republican Scientific and Practical Center for Pediatric Oncology, Hematology and Immunology. Statistics
According to the Republican Cancer Registry, the incidence of Hodgkin's lymphoma in children in Belarus is 1.34:100,000. The disease occurs at all ages except for children under one year of age, extremely rarely - up to 5 years, most often among adolescents from 15 to 19 years. Every year in our country there are about 30 cases of HL among children and adolescents.
Causes and risk factors
The specific cause of HL remains unknown in most cases. The role of viruses in the etiology of malignant lymphomas (Epstein-Barr, cytomegalovirus, herpes virus type 6) is currently being studied, but indisputable evidence of the viral theory has not been obtained. In addition, factors predisposing to the development of HL include various immunodeficiency conditions (taking drugs that suppress the immune system, HIV infection, congenital immunodeficiencies), exposure to ionizing radiation and genetic factors.
Clinical picture
In HL, the tumor is represented by malignant Reed-Sternberg cells and Hodgkin cells. Various internal organs may be affected, causing disruption of their normal functioning.
Tumor conglomerate of cervical lymph nodes in Hodgkin lymphoma. As a rule, the first sign of the disease is a painless enlargement of one or more lymph nodes, often in the neck, less often in the axillary, groin area. Sometimes the tumor process begins in places inaccessible to inspection - the chest (mediastinum) or abdominal cavity. Then the enlarging lymph nodes can put pressure on neighboring organs, causing a dry cough, shortness of breath, and abdominal pain. The tumor can spread to internal organs (lungs, liver, kidneys, etc.).
In addition to enlarged lymph nodes, symptoms such as fever, weakness, night sweats, itchy skin, and weight loss may be observed. These symptoms are taken into account when determining the stage of the disease.
Diagnostics
To diagnose HL, it is necessary to perform a biopsy of the affected lymph node or its conglomerate, followed by histological and immunohistochemical studies. The tumor substrate of HL is Reed-Sternberg cells (large binucleate cells) and Hodgkin cells, displacing normal cells of the lymph node of any area of the body. Malignant cells are surrounded by a cellular infiltrate consisting of histiocytes, lymphocytes, monocytes, plasma cells and eosinophils. The histological variant of HL depends on the structure of the reactive microenvironment of tumor cells (cellular composition).
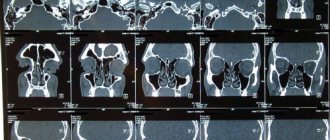
To determine the extent of the tumor process, adequate staging of the disease is necessary before starting treatment. Until recently, ultrasound data of peripheral lymph nodes, abdominal and pelvic organs, CT or MRI were considered standard methods. If necessary, bone marrow biopsy and skeletal scintigraphy were performed.
Currently, the standard examination for HL is positron emission tomography with 18F-fluorodeoxy-glucose combined with CT (PET-CT).
PET-CT allows you to more accurately determine the lymph nodes and areas of the body involved in the tumor process, determine the stage and extent of treatment. In our country, this method has become available to all patients with HL since 2022. The stage of the disease is determined according to the Ann Arbor system (Cotswold revision of staging, adopted at a conference in Ann Arbor, USA). This staging system takes into account the number of lymphatic zones and areas involved in the tumor process, the location of the affected lymph nodes on one or both sides of the diaphragm, the presence or absence of extralymphatic spread of the tumor (E), localized or disseminated process, as well as the presence or absence of systemic symptoms (A or in).
According to the International Clinical Classification, there are 4 stages of HL.
Hodgkin's lymphoma diagnostic cells
Reed-Sternberg cell.
Hodgkin cell.
Forecast
In children and adolescents, HL is one of the most curable tumors. About 85–90% of patients with classical HL are cured in the early stages of the disease (compared to 75–80% of patients with advanced stage). Unfortunately, every year from 15% to 20% of primary cases of HL in children and adolescents in Belarus are detected in an advanced form (stage 4).
Treatment
Treatment of patients with HL is a long process, takes from 3 to 12 months and is carried out according to special protocols. Depending on the stage of the disease, patients are divided into 3 groups (with their own intensity and duration of therapy).
Therapy for Hodgkin's disease consists of two stages: polychemotherapy, aimed at maximizing the destruction of malignant cells and achieving remission with the help of chemotherapy, and radiation therapy, aimed at consolidating and long-term maintenance of remission by destroying residual tumor cells, which may subsequently cause a relapse.
Results of treatment for HL at the Republican Scientific and Practical Center DOGI
Over the past decade, the Republican Scientific and Practical Center for Pediatric Oncology, Hematology and Immunology has used a treatment protocol for HL developed by German pediatric oncohematologists, which has shown to be highly effective. Five-year overall survival is 98%, event-free survival is 90%, but in patients with advanced disease (stage 4 disease) it is significantly lower (89% and 74%, respectively). The most significant factor influencing the effectiveness of treatment is the volume of the original tumor, estimated by the size of the lymph node conglomerates (especially the mediastinal lymph nodes) and the number of affected areas. In recent decades, the proportion of patients with no complete effect or relapse of the disease has remained virtually unchanged and is 25% for adults. Among children and adolescents with HL in Belarus, such patients account for 10%.
In Europe and the USA, attempts have been made to treat this category of patients with more intensive chemotherapy regimens (PCT). Since 2022, the Republican Scientific and Practical Center DOGI has also introduced a new protocol for the treatment of patients with high-risk HL. Intensification of therapy in such patients has shown high efficacy and acceptable toxicity.
The first treatment protocols for HL necessarily included high-dose radiation therapy (RT) (35–40 Gy). Over time, it became apparent that the radiation dose could be lower with combination treatments. In addition, it is the delayed effects of RT that are decisive in the development of adverse long-term effects after treatment for HL (secondary tumors, cardiovascular diseases, pulmonary dysfunction).
With the active introduction of PET-CT in the diagnosis of lymphomas, a new era in the treatment of children with HL began. PET-CT has become actively used not only for staging, but also for assessing remission status and early response to therapy. Rapid achievement of PET negativity is a marker of tumor sensitivity to chemotherapy. A way has emerged to identify patients for whom it is possible to refuse RT. Since 2017, RT has been discontinued in patients with early stages who have achieved complete remission according to PET-CT data after completion of the PCT stage.
Despite significant successes in the treatment of HL in children, a certain number of therapeutic failures remain; 5% of patients with HL are refractory to first-line therapy and 5% of patients have a relapse of the disease, with 90% of cases occurring within the first two years. The return of the disease is much more common in patients with advanced stages. If the child relapses late (more than a year has passed since the end of treatment), then the second course of chemotherapy and radiation gives very good results (10-year survival in more than 90% of patients). If the child has an early relapse (3 to 12 months have passed since the end of treatment), very intensive therapy (high-dose chemotherapy with autologous hematopoietic stem cell transplantation (autoHSCT)) is required to have a good chance of recovery. The use of standard second-line chemotherapy in these patients allows achieve an answer in 50% of cases.
As knowledge in the fields of biology, pathology and immunology has developed, it has become possible to find therapeutic targets and develop new drugs that should not only be effective, but also less toxic. This is especially true for pediatric and young patients. The CD30 receptor on HL tumor cells became such a target. Since 2011, it has become possible to use regimens that include a targeted drug (monoclonal antibody brentuximab vedotin for the treatment of patients with refractory and recurrent HL), which leads to a pronounced and sustained response to therapy. Since 2015, the Republican Scientific and Practical Center DOGI has included this drug in anti-relapse treatment regimens, which made it possible to achieve complete remission in 85% of patients with refractory HL.
Currently, the development of treatment methods that reduce the likelihood of complications and long-term consequences in survivors of the disease continues.
Clinical case
Patient M., 17 years old. Considers himself sick since June 2016, when he experienced a weight loss of about 5 kg in 2 months, itching of the skin of the legs and feet, in the evenings a rise in temperature to subfebrile values (max. 37.9 ° C), pain in the knee joints and lumbar region . He was examined by a rheumatologist at his place of residence. Clinical examination revealed an increase in cervical-supraclavicular and axillary lymph nodes; a general blood test revealed an increase in ESR to 62 mm/h, leukocytosis to 12.4-109/l. Antibacterial therapy was carried out (amoxiclav for 7 days), without effect. According to ultrasound data, OBP is focal changes in the structure of the spleen. Consulted with a hematologist at the diagnostic center, with suspicion of a lymphoproliferative disease he was sent to the Republican Scientific and Practical Center DOGI.
At the time of admission to the center (08/30/16): the condition was of moderate severity. Temperature 37.6 °C. The skin and mucous membranes are of normal color and clean. Peripheral lymph nodes: multiple cervical lymph nodes are palpated on both sides up to 2.5 cm, dense, in the supraclavicular region multiple dense ones up to 1.5 cm on both sides, axillary lymph nodes on both sides up to 2.5 cm, dense, mobile, in conglomerates. Other groups of peripheral lymph nodes are not enlarged. Heart sounds are clear, rhythmic, heart rate - 80 per minute. Breathing is vesicular, wheezing is not heard, respiratory rate is 18 per minute. The abdomen is soft and painless. The liver and spleen are not enlarged.
KBC: Hb 119 g/l, erythrocytes 4.29-1012/l, platelets 329-109/l, leukocytes - 13.02-109/l, e - 1%, s - 87%, l - 7%, m - 3%, ESR - 62 mm/h.
BAC: ALP - 107 IU/l, LDH 248 IU/l, bilirubin -17.8 µmol/l, ALT - 30, AST - 23, CRP - 3.4 g/l (normal up to 0.5), urea - 6.5 mmol/l, creatinine - 72 mmol/l, protein - 86.2 g/l.
Ultrasound of the iliac lymph nodes: the iliac lymph nodes are not significantly enlarged; the structure of the spleen is heterogeneous, single lesions up to 10 mm in the structure of the spleen; lymph nodes at the gate of the liver up to 14 mm.
Ultrasound of peripheral lymph nodes: hyperplasia of the lower cervical, supraclavicular, subclavian and axillary lymph nodes on both sides with pathological changes in structure (ultrasound picture of lymphoproliferative disease).
An open biopsy of the axillary lymph node on the left was performed, morphologically - areas of lymph node tissue with the presence of an erased structure, the formation of fibrous septa and accumulations of lacunar, diagnostic and Hodgkin cells. IHC: CD3(+ background cells), CD30(+++), CD15(++), pax5(++), CD20(-), EBV(-).
Hodgkin's lymphoma, variant nodular sclerosis, mixed cellular composition, grade 1. NOS (9663/3).
PET-CT: in the anterior mediastinum of the upper floor, in the middle with an accent to the right, there is a tumor mass; 36-73-60 mm. Isolated enlarged lymph nodes: paratracheal and bifurcation, up to 15 mm; parasternally on the right, up to 18 mm. According to PET data: accumulation of radiopharmaceuticals in addition to the nodes described above - in the right root (bronchopulmonary l/nodes), in l/nodes - precordially on the right, in the cardiodiaphragmatic region on the left, paraesophageal (node on CT, 14 mm).
No foci of pathological density were identified in the pulmonary parenchyma. The pulmonary pattern is not changed. The lobar and segmental bronchi are patent. The roots of the lungs are not expanded, structural. The axillary nodes are not enlarged. The pleural cavities are free. Soft and bone tissues of the chest without structural changes. There is an increase in retroperitoneal lymph nodes, up to 23 mm; common iliac up to 15 mm. On PET, pathological accumulation of radiopharmaceuticals, in addition to the nodes described above, is in the porta hepatis, in the external iliac nodes, and in the spleen.
No pathological space-occupying formations were detected in the abdominal cavity and retroperitoneal space. The liver is not enlarged and has a homogeneous structure. The pancreas is homogeneous, of normal size and position. Kidneys without visible changes.
In the left ilium, a focus of hyperdense density with finely tuberous contours measuring 10.5-6.6 mm is determined. PET also shows increased accumulation of radiopharmaceuticals in the vertebral bodies C6, Tn4, L5, S1; ribs; pelvic bones.
Conclusion: lymphoproliferative disease with damage to the lymph nodes on both sides of the diaphragm, spleen, and bones.
MRI of the pelvic bones, lumbosacral spine, femurs: multiple different-sized foci of pathological signal are determined in the pelvic bones (pubic, iliac, ischial on both sides), femurs on both sides, sacrum (body with transition to the transverse process on the left of the L5 body vertebra, as well as small ones in the body of L4 (up to 9–10 mm) and L2 (up to 5 mm).
Conclusion: MRI picture of multifocal lesions of the pelvic bones, femoral bones on both sides, sacrum, L5, L4, L2 vertebrae.
Diagnosis: classic Hodgkin's lymphoma (nodular sclerosis variant) with damage to the cervical-supraclavicular lymph nodes on both sides, subclavian lymph nodes on both sides, mediastinal lymph nodes, root of the right lung, axillary lymph nodes on both sides, lymph nodes at the porta hepatis, para-aortic lymph nodes, spleen, iliac lymph nodes on both sides, multiple lesions of skeletal bones. Stage IVB.
The patient underwent 6 blocks of PCT according to BEACOPP-escalated schemes.
A complete metabolic response was obtained according to PET-CT data after the PCT stage. In order to consolidate remission, radiation therapy was performed on the areas of the initial lesion in SOD = 20 Gy.
Special treatment completed on 03/21/17. The patient is still in stable remission and is being monitored by an oncologist at his place of residence.
Localization of lymph nodes
When lymph nodes are enlarged, it is important to determine the cause/source of the changes. Palpation of inguinal or axillary lymph nodes is unlikely to be associated with the disease, cervical - possibly supraclavicular - probably (further assessment and differential diagnosis are required) [2].
Often, enlargement of the supraclavicular lymph nodes on the right is associated with a tumor or infection of the mediastinum, and on the left – with metastases of an abdominal tumor. When palpating the supraclavicular lymph nodes, an additional examination is recommended - CT or MRI of the chest [5]. Read more in the article “Management of lymphadenopathy in children.”
What treatment is prescribed
Therapy should be aimed at eliminating the cause that caused the swelling of the lymph node. For example, for colds, the pediatrician selects medications and physical procedures to fight the virus, relieve inflammation, and increase immunity. If the cause is caries, it is necessary to heal the diseased tooth and eliminate the source of infection.
Sometimes enlarged lymph nodes are a normal reaction of the body, and sometimes they are a symptom of an inflammatory process. Therefore, only a specialist should always find out the reason. The children's medical center employs experienced pediatricians who will find an approach to even the most capricious and fearful patient, help to understand the causes of enlarged lymph nodes and provide effective therapy.
Consistency of lymph nodes
Dense lymph nodes, especially if accompanied by redness, increased local temperature, fluctuation, are often detected in infectious diseases.
Dense lymph nodes and without redness are often detected in viral infections and systemic diseases [5].
Dense, hard, immobile lymph nodes are a finding in malignant diseases.
Normally, the lymph nodes are soft, elastic, mobile (easily displaced upon palpation).
Consolidation of the lymph nodes may be associated with fibrosis or hemorrhage into it, immobility and cohesion are possible with the germination of metastases, or inflammation of surrounding tissues (tuberculosis, sarcoidosis).
Enlargement of lymph nodes can be generalized (enlargement or change in 2 or more unrelated groups of lymph nodes). Often generalized lymphadenopathy is accompanied by an enlarged liver and spleen, and a rash may be present. Generalized lymphadenopathy is not always a sign of serious pathology [5].
Localized lymphadenopathy is often found in children (palpation of the cervical, less often inguinal lymph nodes).
Most often, lymphadenopathy is localized and affects the nodes of the neck and head (3:1) [7].
In most cases, lymphadenopathy resolves on its own or after adequate treatment [5]. If lymphadenopathy does not resolve within 3–4 weeks, it is advisable to consider additional testing [5].
3. Diseases leading to inflammation of the lymph nodes
If the lymph nodes become inflamed and enlarged in more than one area of the body, it is called generalized lymphadenopathy.
This inflammation of the lymph nodes is caused by:
- Viral diseases such as measles, rubella, chickenpox or mumps;
- Mononucleosis, the symptoms of which are fever, sore throat, fatigue, as well as the viral infection cytomegalovirus that causes similar symptoms;
- Bacterial diseases such as strep throat (caused by streptococcus bacteria) or Lyme disease (a bacterial infection spread by certain types of ticks);
- Side effects from taking phenytoin, a medicine used to prevent seizures;
- Side effects from the measles-mumps-rubella vaccine;
- Cancer - leukemia, Hodgkin's disease and lymphoma;
- AIDS, acquired immunodeficiency syndrome;
- Syphilis is a sexually transmitted disease.
About our clinic Chistye Prudy metro station Medintercom page!