Fluoridation of baby teeth.
In childhood, caries progresses rapidly. This often leads to tooth loss. Fluoridation takes place at the white spot stage, this helps to avoid the penetration of the disease inside.
The composition of the preparation for fluoridation of teeth includes silver fluoride diamine. Crystals of silver phosphate and calcium fluoride prevent the entry of pathogenic microorganisms and also inhibit the activity of microbes. Process:
Tooth enamel affected by caries is carefully cleaned of plaque, then the drug is applied. This method allows you to avoid too violent a reaction from a small patient. Treatment usually takes place in 3-4 procedures every 6 months.
Sign up for fluoridation
Streptoderma
Ulcer
Diabetes
22792 November 26
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Streptoderma: causes, symptoms, diagnosis and treatment methods.
Definition
Streptoderma (impetigo) is an infectious skin disease that is more common in childhood. Belongs to the group of pyoderma, which is based on purulent lesions of the skin, its appendages, as well as subcutaneous fatty tissue.
Causes of streptoderma
As the name of the disease suggests, the causative agents of streptoderma are usually streptococci.
Exogenous factors contributing to the development of the inflammatory process and its relapses include:
- violation of the integrity of the epidermis (microtraumas, maceration of the skin);
In adult patients, infection can enter the skin as a result of non-compliance with the rules of asepsis and antisepsis when performing cosmetic procedures (mesotherapy, peelings, etc.) or when using contaminated cosmetic instruments. - increased sweating (hyperhidrosis);
- shift of skin pH to the alkaline side, the effect of high and low temperatures;
- skin contamination.
Endogenous risk factors include:
- various endocrinopathies (for example, diabetes mellitus);
- insufficient intake of proteins into the body;
- presence of severe somatic diseases;
- chronic intoxication;
- the presence of foci of infection in various organs and tissues.
Streptoderma is a contagious disease and can be transmitted by contact (through a handshake, contact with a surface on which a streptococcal infection is present, etc.) and by airborne droplets.
Classification of streptoderma
Streptoderma can be superficial and deep.
Superficial streptoderma:
- streptococcal impetigo,
- crevice impetigo,
- paronychia,
- papulo-erosive streptoderma,
- intertriginous streptoderma,
- erysipelas,
- Streptococcal toxic shock syndrome (STSS),
- acute diffuse streptoderma.
Deep streptoderma:
- cellulite,
- ecthyma vulgar.
There are three stages of streptoderma:
- initial, when there are small purulent rashes resembling blisters;
- non-bullous, which develops after the opening of the vesicles and is characterized by the formation of streptococcal ecthyma (ulcerative streptoderma);
- chronic, which develops either due to improper treatment of the disease or as a result of decreased immunity and is characterized by regular rashes.
Symptoms of streptoderma
Impetigo streptococcal
observed in children of different age groups. It is characterized by the formation of conflicts (rash elements) with serous or serous-purulent contents, mainly on the skin of the face. As a result of the opening of the blisters, ulcers are formed, which are covered with dry crusts that fall off after 3–4 days. Scars form after the disease extremely rarely.
For bullous impetigo
characteristic rashes with serous-purulent contents and surrounded by a pink halo. After opening, erosions, covered with a thin crust, form in their place. The rashes are localized mainly on the lower extremities and the back of the hands.
Slit impetigo (jamming)
represents shallow cracks and erosions that tend to macerate (wet). Localized in the corners of the mouth, at the outer corners of the eyes, at the base of the wings of the nose.
Paronychia (superficial panaritium) is a phlyctena on an inflamed base, localized around the nail plate.
Papulo-erosive streptoderma
is observed in infants and is localized on the skin of the buttocks, back and inner thighs, in the perineum, and scrotum. The disease is characterized by dense bluish-red papules surrounded by inflamed skin. Phlyctens form on the surface of the papules, which quickly open with the formation of erosions and crusts.
Intertriginous streptoderma
localized on the contacting surfaces of large folds (inguinal, axillary, cervical, buttock, behind the ears). The bubbles quickly open with the formation of weeping erosions that have clear boundaries. This form of streptoderma often occurs in children and adults with excess body weight, diabetes mellitus, and hyperhidrosis.
Erysipelas
, as a rule, is localized on the legs, arms, torso (in areas of surgical wounds), on the face (as a complication of rhinitis or conjunctivitis), in children - on the cheeks, in the periorbital region, on the neck and limbs. Inflammation is represented by erythema with raised edges, clear boundaries of irregular outline. The source of inflammation is swollen, shiny, hot to the touch, painful on palpation. Sometimes blisters, subcutaneous abscesses, and necrosis form on the surface of the lesion.
Streptococcal toxic shock syndrome (STSS)
characterized by the acute development of shock and organ failure. The patient quickly develops hypotensive shock with renal failure. Soft tissue infection is observed in 80% of patients and in most cases (70%) occurs as a severe subcutaneous infection (necrotizing fasciitis, myositis). Vesicles and blisters on the surface of the inflammatory focus do not appear immediately and not in all patients and are an unfavorable prognostic sign. Mortality reaches 30%.
Early signs of STSS may include hyperemia of the conjunctiva and oropharyngeal mucosa, and a crimson tongue.
Other skin signs include petechial, maculopapular, and diffuse scarlet-like rashes.
Acute diffuse streptoderma
characterized by the presence of conflicts, prone to peripheral growth and fusion with the formation of large erosions, bordered by a rim of exfoliated epidermis. There is pronounced swelling, hyperemia, profuse oozing, and serous crusts. The process is localized, as a rule, on the lower extremities, as well as around infected wounds, fistulas, and burns.
Cellulite
– infectious inflammation of the dermis and subcutaneous fat. The inflammatory focus has a bright red color, unclear contours, swollen, hot and painful on palpation. Within the focus of inflammation, vesicles, blisters, hemorrhages and even an abscess can be observed. Cellulite can appear on any part of the skin, but is more often localized on the skin of the lower extremities and face. Patients complain of malaise and body temperature rises.
Ecthyma vulgaris
– deep tissue damage with ulceration in a limited area. The disease manifests itself with the appearance of blisters with purulent contents, which within a few days become covered with crusts, under which deep ulcers form. Scars form at the site of the ulcers.
Diagnosis of streptoderma
Diagnosis of streptoderma is not difficult; the diagnosis is made based on the clinical picture and laboratory tests:
- bacteriological examination of purulent discharge with determination of sensitivity to antibacterial drugs;
Caries of baby teeth
Many children are limited in their access to sweets, mistakenly assuming: “If there are no sweets, there will be no tooth decay.” However, caries also appears for other reasons:
- improper or insufficient oral hygiene;
- infection by pathogenic organisms;
- genetic predisposition;
- taking medications.
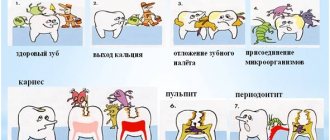
Just like in adults, caries in children is divided into three main stages:
- Caries in the initial stage is a spot.
The disease at this stage is practically asymptomatic. The affected tooth does not respond to stimuli, external damage is invisible.
- Middle stage caries.
At this stage, bad breath appears. A noticeable carious spot appears on the affected area.
- Deep stage caries.
The carious stain spreads faster and faster, and the color of the teeth changes. When exposed to any irritants, acute pain appears, which goes away immediately after the irritants disappear.
Caries of primary teeth has the following features:
- Symptoms may not appear for a long time;
- a child may become vulnerable to caries due to infectious diseases;
- there is a low level of mineralization;
- defeat is possible immediately after teething.
They use a method of treating the affected tooth by blowing it with a mixture of special powder and air.
Sign up for caries treatment
Treatment of caries of primary teeth
Children under 4 years of age are treated with dental fluoridation at the staining stage. Children are often afraid of the sound of a working dental unit, and try in every way to interfere with the doctor. In such cases, there is an alternative to drilling the tooth. A small amount of a special substance is injected into the carious cavity, which softens the pathological mass of caries, after which the doctor cleans the tooth with a hand instrument, then inserts a filling.
They use a method of treating the affected tooth by blowing it with a mixture of special powder and air. This method of treating children's teeth without drilling does not cause pain or anxiety for young patients.
Sign up for caries treatment
Gum inflammation
Inflammation of the gums or gingivitis manifests itself in the form of damage to the tissues of the oral cavity. This disease does not affect the tissues of the tooth itself, the connecting gums and the periosteum.
The main reason for the development of gingivitis is insufficient oral hygiene.
Other reasons:
- unbalanced diet. Lack of important vitamins and minerals, particularly vitamin C;
- diabetes;
- bad heredity;
- infection with viral infections;
- mucosal injuries due to malocclusion;
- burns.
Gingivitis is classified as follows:
- Atrophic.
The tissues and gums become noticeably thinner. Bleeding, exudate, and severe pain appear. The bases of the teeth are heavily exposed at this stage.
- Ulcerative-necrotic. This type of pathology is characterized by unbearable burning pain at the base of the teeth. Small stitches appear and the teeth are partially exposed. The patient may experience general malaise - weakness, nausea and fever.
- Hypertrophic.
The gums of the teeth swell so much that the teeth can be completely hidden in the swelling.
- Desquamative.
In this case, peeling of the mucous membrane and redness of the gums are characteristic.
- Marginal.
One of the varieties of catarrhal gingivitis, which occurs in a milder form. The symptoms of these two forms of the disease are similar, but this one is often confused with teething.
- Catarrhal.
The most common type of disease. It is characterized by itching, burning, swelling of the gums, and redness.
Sign up for gum treatment
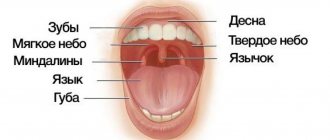
Oral diseases in children and their prevention.
The oral mucosa is constantly exposed to a variety of irritants - chemical, mechanical, thermal, numerous microbial agents and toxins. In addition, the oral cavity is a sensitive indicator, showing the state of the internal organs and promptly signaling the presence of problems in one or another body system.
There is a common name for inflammatory diseases of the oral mucosa - stomatitis.
A characteristic manifestation of stomatitis is the appearance on the oral mucosa of foci of redness, blisters, erosions (afts) or ulcers covered with plaque. These lesions are most often detected on the mucous membrane of the cheeks, floor of the mouth, hard palate, and tip of the tongue. Often there is pain at the location of erosions and ulcers, enlargement of nearby lymph nodes, and sometimes an increase in body temperature. The average duration of the disease is 7-14 days. Stomatitis can recur with decreased immunity, poor diet, hypovitaminosis, infectious diseases, and exacerbations are more common in spring and autumn.
Sources of oral infection
Dirty fingers and toes, dirty small objects and parts of toys, candy that has fallen to the ground - all this can end up in a child’s mouth and serve as a source of infection of the oral cavity with pathogenic microorganisms. Therefore, stomatitis is also called “the disease of dirty hands.” Another source of infection is contact with children who already have an oral infection (for example, herpes). Herpetic stomatitis in children has a long incubation period, reaching 26 days, and the first subtle signs of inflammation may escape the attention of the parents of the child, who is already a source of infection for other children. This leads to the rapid spread of viral infection through airborne droplets and contact.
Treatment and prevention of stomatitis
At the first symptoms of stomatitis, you should consult a dentist. In this case, you should not self-medicate. After all, depending on the type of disease, the doctor prescribes specific treatment. Prevention consists, first of all, in strengthening the child’s immunity - maintaining a proper sleep and rest schedule, carrying out water procedures, and a nutritious and balanced diet. Hygiene standards should be observed: clean toys and utensils, do not lick pacifiers and spoons when feeding the baby. Avoid contact with children and adults who have signs of herpes infection. Correctly select, store and change toothbrushes in a timely manner.
The task of parents, from the appearance of the child’s first teeth, medical workers, and kindergarten teachers, is to teach the child to maintain oral and hand hygiene.
Manager
third pediatric department
O.I.Ivanenko