Fast passage
Hemophilia Hemochromatosis Duchenne muscular dystrophy Huntington's chorea Fragile X syndrome Turner syndrome Klinefelter syndrome
Congenital diseases can be caused by genetic mutations (inherited or spontaneous), maternal infections during pregnancy (cytomegalovirus, chickenpox, rubella), exposure to drugs and chemicals that pollute air, water or food. The causes of many birth defects are still unknown.
About 20% of congenital diseases are caused by genetic or hereditary factors. These include disorders in which the mutation affects one gene (sickle cell anemia); chromosomal disorders in which chromosomes (or parts thereof) are missing (Turner syndrome) or have structural changes (an increase in the number of chromosomes or trisomy in Down syndrome); multifactorial disorders caused by mutations of two or more genes. Birth defects and developmental disorders can cause deletions or duplications of individual genes (changes in mitochondrial DNA). An example of such a disease is cystic fibrosis, characterized by damage to the exocrine glands and vital organs (lungs and gastrointestinal tract). Congenital diseases are also associated with random (new) gene damage, spontaneous (not inherited from parents) mutations (most cases of achondroplasia).
According to statistics, 2–3% of infants have congenital diseases. By the age of 1 year, their number increases to 5%, since not all of these pathologies are diagnosed immediately after birth.
Congenital (hereditary) diseases are also classified according to the type of inheritance. With autosomal dominant inheritance, the disease can be transmitted from parent to child in 50% of cases (Duchenne muscular dystrophy, Huntington's chorea). In autosomal recessive inheritance, the genetic abnormality is passed on to the child only if both parents have the same defective gene (cystic fibrosis, sickle cell anemia). Here the inheritance rate will be 25%, that is, on average, 1 child out of 4 children of these parents will have an autosomal recessive disease.
Pathological conditions can also be transmitted through sex-linked inheritance (inheritance of a gene located on the sex chromosomes). X-linked recessive diseases are almost always limited to the male sex (hemophilia, color blindness, Duchenne muscular dystrophy). X-linked dominant diseases occur in both boys and girls, but in male children they have a more severe course (X-linked hypophosphatemic rickets). Y-linked diseases are quite rare because the Y chromosome contains only a few genes (ichthyosis).
Some congenital diseases are not formally classified as genetic, but have one or another degree of inheritance: risk factors or the gene itself are inherited, but with low penetrance (the frequency of manifestation of the gene in traits).
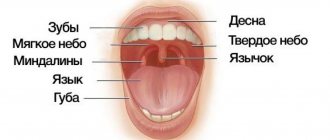
Congenital pathologies of the tongue and frenulum - types and features
Anomalies of the tongue can be either congenital or acquired; they are often the result of certain pathological processes occurring in the body. Currently, malformations of the main speaking organ are quite rare. Many of them are serious problems that often require surgery. Further in this article we will talk about what congenital defects of the tongue and frenulum exist, how they are corrected, and also consider in detail such a pathology as a folded tongue.
Types of congenital anomalies
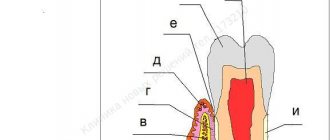
Currently, in medicine and dentistry in particular, a specific list of main pathologies is identified, each of which has its own deviations. Anomalies of the development of the main organ of the oral cavity include the following disorders:
- aglossia is a rare anomaly in which the tongue is completely absent,
- microglossia - the absence of the front part of the organ, due to which it has an abnormally small size, becomes too short,
- macroglossia - in this case the organ grows excessively, which is accompanied by generalized hypertrophy of the jaw muscles,
- splitting - its two parts are separated vertically, they simply do not grow together, remaining completely separate from each other. This tongue resembles a snake's,
- lingual tonsils - enlarged lymph nodes in the root area of the organ,
- rhomboid glossitis - characterized by the formation of an inflamed area in the shape of an oval or diamond at the base, usually blue-red in color,
- folding is a defect in size and shape, in which deep grooves and folds covered with papillae appear on the surface of the organ,
- a villous (hairy) tongue is a rather rare phenomenon, leading to hardening of overgrown filiform papillae. As a result, the area at the root turns brown or even black,
- Tongue goiter is a pathology in which thyroid tissue develops inside the organ and manifests itself as an uneven surface.
Modern medicine in most cases corrects such defects - in such situations, the problem of aesthetics and functionality is solved through surgery and plastic surgery.
Huntington's chorea
Huntington's chorea (Huntington's disease) is a genetic, progressive neurodegenerative disease characterized by the gradual development of involuntary muscle movements affecting the arms, legs, face and trunk, as well as progressive deterioration of cognitive processes and memory, and mental disorders.
The disease is inherited in an autosomal dominant manner (can be transmitted through both the female and male lines) and occurs as a result of mutations in the HHT gene (expansion of cytosine-adenine-guanine trinucleotide repeats).
Symptoms and physical manifestations of the disease result from the degeneration of nerve cells (neurons) in certain areas of the brain (basal ganglia, cortex) and usually appear between the ages of 35 and 45. The life expectancy of a person suffering from Huntington's disease is 15–20 years from the onset of symptoms. They include: choreic hyperkinesis (chaotic, jerky, erratic movements of varying amplitude and intensity), involuntary movements of the eyes (nystagmus) and facial muscles, frowning and raising the eyebrows, decreased cognitive abilities, irritability, anxiety, apathy, hallucinations, depression, anosmia, problems with balance and walking, general weakness, weight loss associated with malnutrition, in the late stage of the disease - muscle rigidity, bradykinesia (slowing of active movements), serious worsening of the choreic syndrome, loss of the ability to speak, move, dysphagia, inability to care for oneself.
There is a less common (5-10% of cases) form of hCG that develops in childhood or adolescence (juvenile Huntington's disease). It is also characterized by hyperkinesis, decreased cognitive abilities, impaired coordination and mental disorders. Children experience a rapidly progressive decline in school performance associated with impaired cognitive abilities. Other symptoms include bradykinesia, tremor, myoclonic spasms, dystonia, muscle rigidity, speech dysfunction, and dysphagia. These symptoms can affect the mental state, causing irritability, bad mood, sadness, fears, and aggression. In some cases, behavioral problems are the first sign of the onset of the disease.
The juvenile form is also inherited in an autosomal dominant manner (but most often from fathers) and occurs as a result of mutations in the HTT gene. Life expectancy (from the onset of symptoms) is no more than 15 years.
The diagnosis of Huntington's chorea is made based on symptoms, family history, and molecular genetic testing.
There are no medications that affect the cause of the disease. Patients with hCG are prescribed symptomatic therapy aimed at alleviating symptoms (in particular, choreic hyperkinesis, dystonia, muscle rigidity, behavioral and mental disorders) and improving quality of life.
Congenital pathology of the frenulum
Separately, it is worth highlighting the independent pathology of the frenulum of the tongue - the part attached to its center from below. There are also frenulums of the upper and lower lips - they join the mucous membrane in the area of the central incisors. In normal development, the hyoid ends right in the center of the organ, while in a disorder called ankyglossia, it is located too close to its tip - this anatomical abnormality is often called a short frenulum.
Congenital pathology of the frenulum of the tongue
On a note! Today, cases of ankyglossia occur in one child out of a thousand. Moreover, this pathology is diagnosed almost three times more often in boys than in girls1.
With this pathology, at the stage of breastfeeding, the baby is unable to latch onto the breast normally. Later, the child will experience certain difficulties in speech, will not be able to pronounce individual sounds and stick out his tongue far. Often there are disturbances in the formation of the dental system as a whole, and displacement of teeth is observed due to improper functioning of the tongue.
“I remember when I was a child my bridle was cut. True, I can’t say that I experienced any serious difficulties while talking or eating. It’s just that at the next examination at the dentist, he said that it was better to trim it so that the jaw would continue to form correctly, it seems like that. In general, the procedure was simple, there was generally no pain..."
Arthur H., Tolyatti, from correspondence on a thematic forum
Today, if this anomaly is detected, it can be corrected in the maternity hospital. At this age, the frenulotomy procedure is absolutely painless and does not require anesthesia, since there are no nerve endings in these tissues. In other cases, the operation is performed in preschool or school age as prescribed by a dentist. There is also an option for the so-called frenulum stretching - a speech therapist works with the problem. However, you should contact this doctor in any case if the frenulum is cut after the child has already learned to speak, because a new pronunciation will be required, taking into account the correct position of the tongue.
What are mouth guards in orthodontics?
Mouth guards are special designs used to correct malocclusion and dental defects. Unlike braces, they are outwardly invisible and do not interfere with diction.
Features and advantages of mouth guards:
- have a transparent plastic or silicone base;
- you can remove it yourself and carry out thorough hygienic care;
- soft structure that does not injure the oral cavity and does not damage tooth enamel;
- aesthetic designs ensure a tight fit to the teeth;
- do not create discomfort for the patient;
- do not require restrictions on food intake.
The only disadvantages of orthodontic aligners include their higher cost compared to braces, as well as a longer treatment period.
Indications for wearing mouth guards:
- slight curvature of teeth;
- rotation, crooked teeth;
- large gaps between crowns;
- elongation or shortening of dental alveoli;
- abnormal position of the upper canines;
- crossbite (effectively handled by McNamara mouthguard
).
Orthodontics
considers other indications for wearing a mouthguard. Such designs have an undeniable mass of advantages, are easy to maintain and completely invisible to others. They are made in dental laboratories individually for each patient using a dental impression. Installing the aligners takes only a few minutes.
Orthodontic aligners are also used to consolidate the results after wearing braces.
What is scrotal (folded) glossitis - the causes of the anomaly
Scrotal glossitis, or simply folded tongue, is one of the most common congenital pathologies of the tongue, in which during its development the organ acquires an irregular shape and non-standard size. This defect occurs in both children and adults, and the grooves can cover not only a limited area of the surface, but the entire tongue.
On a note! The problem in question may be congenital or acquired. In most cases, it does not pose a serious threat, but it significantly increases the risk of infection and, as a consequence, the development of inflammatory processes.
The photo shows a folded tongue
Typically, this deviation is formed at the stage of intrauterine development and becomes a consequence of an acute deficiency of vital microelements or genetic disorders. Experts identify a number of other factors that may contribute to the problem:
- the presence in the human body of chronic diseases of the gastrointestinal tract and liver,
- diseases of the skin and circulatory organs,
- disruptions in the functioning of the endocrine and nervous systems,
- infectious diseases in acute form,
- collagenoses are a group of diseases leading to pathological changes in connective tissues,
- disturbances in the trophic function of the organ mucosa,
- lack of vitamins and microelements important for the health of the body.
Sometimes such grooves can appear against the background of a sharp restructuring of the body, for example, during pregnancy. If the folds on the surface are not very pronounced and the person does not focus attention on this, he may not be aware of the abnormal development of his tongue.
Fragile X syndrome
Fragile X syndrome (Martin-Bell syndrome) is an inherited disorder characterized by a range of developmental problems, including cognitive impairment, decreased intelligence, autism spectrum disorder, learning disability, and delayed language acquisition.
The disease is caused by a mutation in the FMR1 gene located on the X chromosome; the syndrome is inherited in a dominant, sex-linked manner, is more common in men and causes more severe disorders in them. The FMR1 mutation leads to a multiple increase in the number of CHG trinucleotides and subsequent insufficient production of the FMR1 protein, which is responsible for the development of the central nervous system (the processes of formation of neural connections are disrupted, the ability to learn and remember is reduced).
The prevalence of fragile X syndrome is 1:4000 among boys and 1:6000–8000 among girls. Women pass on the mutation gene 4 times more often than men.
Fragile X syndrome is symptomatically manifested by moderate mental retardation in men and mild mental retardation in women. Physical abnormalities are often noticeable already in childhood (in boys), but in some cases they appear only during puberty. Characteristic: head circumference larger than normal, elongated face, protruding forehead and chin, large ears, mobile joints, decreased muscle tone, incoordination, macroorchidism, flat feet, chronic otitis media, strabismus, flat feet, pectus excavatum, scoliosis, attention deficit disorder and hyperactivity, autism spectrum disorder, delayed motor development, rapid and confused speech with repetitions, episodic seizures, stereotypies, self-harm.
More than 99% of patients with fragile X syndrome have a complete mutation of the FMR1 gene. Molecular genetic testing is performed to determine the number of CGG repeats (usually more than 200) and methylation status. At a child’s early age, a pediatrician can pay attention to deviations in physical development, and at the age of 2–3 years, to cognitive, behavioral, mental and speech disorders. Family history of the disease is an essential criterion for the diagnostic search (male relatives are more often affected).
There is no specific treatment for fragile X syndrome. The patient is prescribed symptomatic therapy depending on the individual situation (antidepressants, antiepileptic drugs), psychological and behavioral correction is provided, and assistance is provided in developing communication, speech, reading and writing skills.
Clinic of scrotal glossitis - how to identify an anomaly
It was already noted above that a folded tongue usually does not cause a person discomfort or trouble. However, against its background the following deviations may also appear:
- the formation of pronounced folds and grooves on the surface is an aesthetic problem,
- macroglossia - growth of organ tissue, against the background of which a person experiences certain difficulties while speaking and chewing food,
- thickening of the tongue
- atrophy of taste buds,
- increased sensitivity,
- burning and tingling sensations,
- enlarged lymph nodes,
- the appearance of bad breath.
Folds and grooves cause an aesthetic problem
If a folded tongue causes discomfort, it is better to seek help from a dentist. The choice of treatment method will largely depend on the degree of development of the pathology.
The danger of folded glossitis
Often, in the absence of any discomfort, scrotal tongue is not treated at all - the anomaly itself does not pose a serious threat to health, except that it increases the risk of penetration and spread of infection, and then the development of inflammation. This situation can occur against the background of a weakened immune system, for example, due to a cold. The situation is aggravated by the inability to properly keep the oral cavity clean, since the defect significantly complicates hygiene procedures. In addition, the problem also affects the aesthetic side of the issue.
Treatment methods
In the event that the folding of the tongue began to form in a child when he was still in the womb, it is possible to talk about any treatment, and especially surgical intervention, only from the age of 5 years. The pediatrician refers the small patient to a pediatric dentist, who prescribes therapeutic procedures, including preventive treatment of the oral cavity with antiseptic agents.
If the pathology manifests itself as a consequence of certain disturbances in the functioning of the internal systems of the body, for example, cardiovascular, endocrine or digestive, treatment should be aimed at eradicating the root cause of the problem. As part of symptomatic therapy, experts prescribe:
- immunomodulatory drugs,
- rinsing and treating the oral cavity with anti-inflammatory and antibacterial solutions; decoctions and infusions of medicinal herbs can be prescribed,
- complete sanitation – elimination of all dental diseases, including caries and inflammation of various etiologies.
Rinsing with medicinal herbs will help in treatment.
To solve the aesthetic problem, a laser is actively used today, which, as it were, evaporates and at the same time helps to smooth out overgrown tissue. As a result, the organ noticeably decreases in size, and its surface is leveled. The surgical method is extremely rarely used to correct a folded tongue, and it consists of suturing the grooves.
Hemophilia
Hemophilia is a group of rare inherited bleeding disorders caused by a deficiency of an essential protein (clotting factor).
Hemophilia A (classical) is more common (>80% of cases) and is associated with a deficiency of coagulation factor VIII, hemophilia B (Christmas disease) is less common (>10% of cases), it is caused by a deficiency of coagulation factor IX. Hemophilia C is very rare and is caused by a deficiency of coagulation factor XI; most often it is not mentioned in the classification of the group.
The disease is X-linked with sex and is inherited recessively in the female line. Classic hemophilia is caused by mutations in the F8 gene, located on the X chromosome. In approximately 70% of cases, the disease is inherited in an X-linked pattern, in other cases it occurs spontaneously (a new mutation), and subsequently the spontaneous disease becomes hereditary. Hemophilia A affects almost exclusively men; rare cases of the disease in women, carriers of the defective gene, are almost always characterized by a mild course. Hemophilia B is caused by mutations in the F9 gene, also located on the X chromosome; it is typical for men; women are very rarely affected. In some cases, the disease occurs spontaneously (acquired hemophilia A or B) and is also associated with a deficiency of blood clotting factors VIII or IX. Acquired hemophilia is an autoimmune disease in which the body produces antibodies that attack clotting factors (most often factor VIII). In approximately half of cases of acquired hemophilia, the patient has an underlying condition or disease associated with it (pregnancy, autoimmune diseases, myeloproliferative diseases, inflammatory bowel diseases, etc.), in other episodes the cause remains unclear.
Hemophilia A affects approximately 1 in 5,000 male births, and hemophilia B affects approximately 1 in 25,000. About 60% of patients have severe hemophilia and are usually diagnosed at birth or within the first 2 years of life.
The age of manifestation of hemophilia and the severity of the disease depend on the level of activity of blood coagulation factors. The mild form is characterized by a level of blood clotting factor (VIII or IX) exceeding 5% of normal, moderate - 1-5%, severe - below 1%. In most patients, regardless of the severity of the disease, bleeding episodes are more common in early childhood, childhood, and adolescence than in later adult life.
In mild to moderate forms of hemophilia, prolonged bleeding may only occur as a result of injury, surgery, or a dental procedure. Often, a child is diagnosed with hemophilia by the age of 5–6 years, paying attention to prolonged post-traumatic bleeding, prolonged bleeding during dental treatment or surgery. Other noticeable symptoms of mild to moderate hemophilia include persistent hematomas (bruises), frequent nosebleeds, and bleeding gums.
Severe forms of hemophilia are characterized by episodes of spontaneous bleeding, which lead to hemorrhages of various locations - in soft tissues, muscles, joints. With hemarthrosis (bleeding into the joint cavity), restriction of joint mobility occurs, accompanied by acute pain and inflammation. In patients with severe hemophilia, spontaneous bleeding most often occurs in the muscles and joints, but can affect any internal organ, including the kidneys, gastrointestinal tract, and brain (hematuria, melena, hematochezia, gastrointestinal bleeding, intracranial bleeding). Severe hemophilia A usually appears in early childhood and is most often diagnosed by the age of 2 years. Common symptoms (if the disease is not treated) are bleeding due to minor injuries to the oral cavity (biting lips, tongue, cheeks), subcutaneous hematomas, large bumps after hitting the head, spontaneous bleeding (2-5 episodes per month).
The diagnosis of hemophilia A or B is established on the basis of symptoms, the patient’s personal and family history, laboratory tests (complete blood count, coagulogram assessing the state of the blood coagulation system and the activity of its proteins, molecular genetic research). Couples at risk of having a child with hemophilia should receive genetic counseling at the stage of pregnancy planning. Determining a specific mutation of the F8 (or F9) gene helps not only to identify female carriers of the defective gene in a particular family, but is also useful for prenatal diagnosis of hemophilia (amniocentesis, chorionic villus sampling).
There are no medications that address the cause of hemophilia. Patients are prescribed replacement therapy aimed at replenishing protein deficiency (VIII or IX blood coagulation factors). Ideally, treatment is done prophylactically, with intermittent administration of clotting factor concentrates at regular intervals (to prevent bleeding episodes and associated complications such as joint damage). Treatment “on demand” (directly during bleeding episodes) is possible. Currently, reputable medical organizations recommend the introduction of recombinant factors (they are produced in the laboratory and do not contain human or animal proteins) to reduce the risk of transmission of various viruses during transfusion of blood components.
Some patients with mild hemophilia are prescribed a synthetic analogue of vasopressin, desmopressin, which increases coagulation factor VIII (administered intravenously or intranasally), as well as antifibrinolytic agents, which slow down the breakdown of clotting factors.
In approximately 30% of cases of treatment of severe cases of hemophilia, long-term replacement therapy can lead to isoimmunization - the formation of antibodies to the administered blood clotting factors (the immune system recognizes the administered factor VIII as foreign). This process may be accompanied by allergic reactions (of varying severity), and the risk of life-threatening bleeding increases. In this case, the patient is prescribed alternative treatment - plasmapheresis, immunosuppressants.