Causes of aphthous stomatitis
Rashes in the form of aphthae on the oral mucosa can be the main manifestation of stomatitis if it occurs as an independent (primary) disease4. In other cases, ulcerations represent a symptom of another disease3,4. But determining the exact causes of inflammation is not so easy, because many different factors can trigger it5.
The development of acute aphthous stomatitis is often associated with a weakening of the body’s defenses after a cold (acute respiratory illness) or sore throat1.
The chronic form occurs under the influence of local and general factors5, among which are the following:
- Infection . The likelihood of aphthous stomatitis increases in the presence of chronic infections, such as tonsillitis (inflammation of the tonsils), pharyngitis (inflammation of the pharynx) and diseases of the gastrointestinal tract8.
- Local trauma. Not every damage to the mucous membrane leads to the formation of aft5. But in people with a hereditary predisposition, its injury quite often leads to ulceration5, especially in those who smoke or use dentures5,7.
- Dry mouth. Changes in the properties of saliva or its deficiency contribute to the aggravation of the symptoms of aphthous stomatitis5.
- Allergic reactions. Allergens can include food products10, components of toothpastes5,10, dust10, worms10, medications10 and materials from which dentures are made, for example, nickel5.
- Deficiency of certain nutrients . Inflammation is promoted by a lack of zinc, iron, folic acid, and group vitamins (B1, B2, B6, B12)5.
- Stress . Difficult experiences, mental overstrain5, chronic stress or frequent change of time zones8 often precede the appearance of new aphthae. In students, the disease often worsens during the session5,7,
- Hormonal disorders. In women, the development of the disease can be facilitated by hormonal changes during menstruation, pregnancy or menopause3.
With chronic aphthous stomatitis, an interesting reaction of the immune system is observed - its sensitivity to certain bacteria10 that inhabit the oral cavity increases7. When the immune response is excessive8, protective antibodies damage not only bacteria, but also their own cells7,8. The reason for this reaction is the presence of structures in the cells of the mucous membrane that are similar to bacterial particles6.
to come back to the beginning
Causes
The most common reasons:
- Presence of infectious diseases.
- Genetic predisposition.
- Increased sensitivity of the mucous membrane.
- Weak immunity.
- Lack of zinc or iron.
- Lack of vitamins.
- Injuries to the oral mucosa.
- Diseases of the gastrointestinal tract.
- Burn of the mucous membrane.
- Allergy to any food product or hygiene product.
- Caries.
- Dry mouth.
- Using the wrong toothbrush.
- Pulpitis.
- Nervous exhaustion.
- Malocclusion.
How does aphthous stomatitis manifest?
The first manifestation of the disease may be a burning sensation in the mouth, which lasts from 2 hours to 2 days5. Later, aphthae5 appear on the mucous membrane - single or multiple12.
Aphthae can be recognized by the following signs:
- they form on the surface of the mucous membrane, representing a shallow defect2;
- covered with a gray-white coating12;
- surrounded by a reddish “rim”2;
- the shape of the ulcers is oval2 or elongated12, and the size in most cases is up to 1 cm in diameter2.
Ulcers can appear on any part of the oral mucosa, as well as on the tongue12. But usually they form where the submucosal layer is pronounced and can easily be damaged2 - this is the area of the cheeks, lips, floor of the mouth (under the tongue) and palate2, 12.
Aphthae are quite painful12, and they cause pain not only during eating or talking, but also at “rest”1, when nothing irritates the mucous membrane.
In addition to pain, aphthous stomatitis causes excessive salivation6 and bad breath1.
to come back to the beginning
Symptoms
The main symptoms of aphthous stomatitis can be detected with the naked eye by looking into the oral cavity.
- Most often, ulcers are located on the inside of the lower lip, but they may be present on the cheeks and gums. Their size can be very small, or cover the entire mucous membrane.
- The resulting ulcers cause pain and discomfort to the child, and bad breath appears. This affects his behavior. Increased irritability occurs, sleep patterns are disrupted, and there is no appetite.
- A white coating may form on the tongue, accompanied by small blisters. They bring a burning sensation. In this regard, children often refuse to eat.
- Body temperature rises. And along with it, the lymph nodes in the neck can become inflamed and enlarged.
The development of aphthous stomatitis in children occurs in several stages. Each has its own characteristics of manifestation. At the initial stage, a cough and runny nose appears, and the throat turns red. Then the body temperature rises and the stage of the appearance of rashes begins. First, single ulcers appear, and then whole groups are formed. They look like yellowish spots with a red border. In its acute form, the disease can even affect the throat.
The disease can occur in both infants and school-age children. Therefore, it is necessary to periodically conduct a diagnostic examination of the oral cavity.
There are several options for the course of the disease:
- Acute is a rapidly progressive form that reaches a peak within a few days. Often accompanied by viral diseases.
- Chronic – occurs in the absence of treatment of the acute form. Accompanied by general malaise. It may disappear on its own, but soon appears again.
- Recurrent - may appear after treatment of a chronic form. Sharply worsens after a long time.
How does aphthous stomatitis occur?
Mouth ulcers appear on the 2-3rd day of illness1. Usually after 7-10 days they heal without leaving marks1. However, when the disease becomes chronic, a relapse may occur1. In this case, a few days or several weeks after healing, aphthae appear again, although in small quantities - from 1 to 31. Although ulcers are painful, general health is usually not affected1.
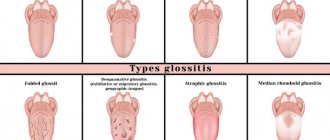
Chronic aphthous stomatitis can occur in different ways2, depending on the size, depth and number of aphthous stomatitis. The following forms of the disease are possible:
- Small. The most common type7, in which elements up to 5 mm in diameter appear on the mucous membrane of the lips, cheeks and floor of the mouth. Aphthae heal without scarring within 10-14 days7.
- Big. This form rarely develops. Its typical manifestation is large ulcers, the size of which sometimes exceeds 1 cm in diameter. Aphthae can be found on the lips, palate and pharynx. They last up to 6 weeks, and after healing, scars remain in their place7.
- Herpetiformis. It is characterized by the appearance of many ulcerations with a diameter of 2-3 mm, which can merge7 (as is observed with herpes3). Their favorite places are the floor of the mouth and tongue7.
In the acute form, the symptoms are very similar to a cold: a person’s body temperature rises, general weakness and fatigue bother him1.
to come back to the beginning
How to treat aphthous stomatitis
Without treatment, the disease can last for many years1. Therefore, if ulcers, pain and burning sensations appear in the mouth, you should consult a doctor. Only a specialist can make a diagnosis and select the optimal treatment regimen. Most often, these patients are managed by dentists, but a general practitioner or family doctor can also help.
Treatment of aphthous stomatitis should be comprehensive, that is, aimed at solving several problems at once8:
- Elimination of foci of infection in the oral cavity using drugs for topical and oral administration8.
- Stimulate healing and support immunity . Wound-healing drugs, immunomodulators and antihistamines, as well as vitamins and micronutrient supplements are used8.
- Treatment of underlying diseases that contribute to inflammation of the oral mucosa, for example, diseases of the gastrointestinal tract and upper respiratory tract8.
During therapy, it is necessary to adhere to a gentle regimen - avoid spicy, rough foods and alcohol, as well as dentures if they injure the mucous membrane8.
To fight the infection, the doctor may prescribe topical medications - antiseptic and antibacterial10. Among them there are also combined agents, such as Metrogyl-Denta®9.
METROGYL DENTA® is a gel that contains metronidazole, which has an antibacterial effect, and the antiseptic chlorhexidine9. This combination can inhibit various types of bacteria and fight infection9.
METROGYL DENTA® is widely used in dentistry; it is approved by the Russian Dental Association11 and is indicated for the treatment of aphthous stomatitis9. The duration of treatment, dose and frequency of use is determined by the doctor, depending on the degree of damage and severity of the disease.
to come back to the beginning
How to treat aphthous stomatitis in children?
Before how and how to treat aphthous stomatitis in children, the child should definitely be shown to a specialist, since self-medication can result in the disease becoming chronic or developing complications. The doctor will conduct diagnostics and tests to determine the specific causative agent of the disease, and then prescribe adequate antibacterial therapy.
The complex also prescribes antipyretics, anti-inflammatory and vitamin preparations, and regular antiseptic treatments of the mucous membrane are carried out. The most commonly used antiseptics are chlorhexidine and hydrogen peroxide; in the past, brilliant green was often used. Some parents still believe that aphthous stomatitis can be treated with brilliant green, but in fact this is just one of the stages of therapy, and is considered outdated, since the alcohol solution additionally injures the mucous membrane.
“32 Dent” clinics provide all types of dental services, including treatment of stomatitis. The professionalism of doctors, coupled with high-quality equipment, guarantees excellent and sustainable results.
Prevention
To prevent aphthous stomatitis, it is important to prevent exposure to risk factors, namely6:
- monitor oral hygiene6;
- quit smoking6;
- exclude allergenic products10;
- if necessary, replace toothpaste10, dentures8 - traumatic to the mucous membrane or made from materials that cause allergies6;
- visit the dentist regularly, every 3-4 months6;
- avoid stress5;
- treat foci of chronic infection in the body6.
Aphthous stomatitis is widespread, and there are many reasons that cause the disease and maintain its chronic course. To prevent the disease from prolonging, you need to eliminate possible provoking factors as quickly as possible and undergo a course of treatment from a specialist.
to come back to the beginning
Treatment
If you detect at least one of the symptoms, you should immediately consult a doctor. Timely detection of the disease allows you to prescribe effective treatment. It is compiled individually, taking into account all the characteristics of the patient. In some cases, tests are required to identify pathogenic microorganisms. Local and general therapy is usually used.
Aphthous stomatitis is not contagious, but in order not to expose the child to additional infections, it is recommended to limit walks in the fresh air during treatment.
Depending on the diagnosis, the following may be prescribed:
- Antipyretics.
- Vitamin course.
- Painkiller.
- Anti-inflammatory.
The initial goal is to eliminate pain and alleviate the condition. For this purpose, antiseptic treatment of the oral cavity is carried out. It prevents the addition of secondary infections. In addition to medications, rinses from decoctions are used:
- Sage.
- Motherwort.
- St. John's wort.
- Daisies.
- Calendula.
- Oak bark.
They cannot replace medical treatment, but these herbs will not hurt as an aid. Before you start rinsing your mouth with herbs, you need to make sure you are not allergic to them.
Treatment of aphthous stomatitis in children is not complete without procedures aimed at strengthening general and local immunity. It is recommended to adhere to proper nutrition and take vitamins. Electrophoresis sessions are possible. Sour fruits, juices, tea, hard, spicy and very salty foods, and carbonated drinks are excluded from the diet. This is necessary in order not to injure areas of inflammation.
If the cause of the disease is dental problems, then dental treatment is prescribed. By treating your teeth, you will be able to quickly get rid of aphthous stomatitis, since the cause of its development will be eliminated.
In infants, aphthous stomatitis is often a reaction to mother's milk. If intolerance is confirmed, the baby must be switched to formula milk.
Literature:
- Aphthous stomatitis. Nurse, No. 5, 2015, p. 21.
- Mikhalchenko V.F., Firsova I.V., Fedotova Yu.M. and others. A new approach to the treatment of chronic recurrent aphthous stomatitis (Setton's aphthosis) using the method of photoactivated disinfection and the immunomodulator Galavit. Modern problems of science and education. No. 6, 2015, pp. 1-6.
- Salomão Israel Monteiro Lourenço Queiroz, Marcus Vinícius Amarante da Silva. Ana Miryam Costa de Medeiros. Recurrent aphthous ulceration: an epidemiological study of etiological factors, treatment and differential diagnosis. (Recurrent aphthous ulcers: epidemiological study of etiological factors, treatment and differential diagnosis). An Bras Dermatol. 2018;93(3):341-6.
- Maksimenko P.T., Skripnikova T.P., Khmil T.A. Nomenclature, clinical classification of diseases, changes in the mucous membrane of the oral cavity, lips and tongue. Ukrainian Dental Almanac, 2008, No. 4, pp. 28-36.
- Sunday O. Akintoye, BDS, DDS, MS* and Martin S. Greenberg, DDS, FDSRCS. Recurrent Aphthous Stomatitis. Dent Clin North Am. April 2014; 58(2): 281–297. doi:10.1016/j.cden.2013.12.002
- Galizina O.A. Main aspects of the occurrence, clinical manifestations, treatment and prevention of chronic recurrent aphthous stomatitis. Russian Dental Journal, 2014, No. 6, pp. 39-42.
- Mahesh Chavan1, Hansa Jain2, Nikhil Diwan1, Shivaji Khedkar3, Anagha Shete1, Sachin Durkar. Recurrent aphthous stomatitis: a review. J Oral Pathol Med (2012).
- Volkov E.A., Butova V.G. Clinical recommendations (treatment protocol) for chronic recurrent aphthous stomatitis. Russian Dental Journal, No. 5, 2014, pp. 35-50.
- Instructions for medical use of the drug Metrogyl-Denta®.
- Strakhova S.Yu., Drobotko L.N. Chronic recurrent aphthous stomatitis (lecture). RMZh, No. 29 dated December 27, 2006, p. 2096.
- Dental gel for gums Metrogyl-Denta® in the treatment of periodontal diseases and oral mucosa. Practical medicine, No. 1(33), March, 2009, pp. 105-106.
- Glukhmanyuk D.S., Malinovsky V.A. Aphthous stomatitis. Proceedings of the scientific and practical conference “Modern problems of pharmacology, cosmetology and aromology.” International Humanitarian University, Odessa Medical Institute, 2015. – 48 p.