Small “ulcers” and inflammations may appear in the oral cavity, causing discomfort, especially when chewing food. These are signs of stomatitis, which is an inflammation of the oral mucosa.
According to scientists, the most common are viral stomatitis.
Of the above types of disease, patients most often consult a doctor with herpetic stomatitis, which is caused by the common herpes virus. There are the following forms of this disease: acute herpetic gingivostomatitis and recurrent chronic herpes.
Let's take a closer look at these diseases.
Causes of stomatitis
Inflammation of the oral mucosa can be caused by various reasons.
- Mucosal injury6.
- Viral, bacterial or fungal infection6.
- Allergy2.
- Immunity disorders (autoallergy, that is, a reaction to one’s own altered tissues2).
- Diseases of the blood, digestive, cardiovascular, nervous and endocrine systems2.
- Hypovitaminosis - lack of vitamins C, B1, B12, E, D32.
- Common infectious processes: measles, rubella, scarlet fever and diphtheria, infectious mononucleosis, tuberculosis and others1.
Only a specialist can understand the causes of stomatitis. Therefore, if symptoms of the disease appear, you should definitely contact your dentist.
Inflammatory diseases of the oral cavity can occur in a child of any age6. Immaturity of the body is the primary factor predisposing to the occurrence of stomatitis in children under one year of age. The mucous membrane of the oral cavity during this period of a child’s life is very vulnerable, its natural protective properties are reduced. The immunity received from the mother during fetal development and which protected the baby immediately after birth weakens every day. Therefore, the infection easily penetrates the mucous membrane and causes its inflammation. Most often at this age, candidal stomatitis occurs, commonly called thrush1,6.
From the age of one to 3 years, children actively develop immune mechanisms to protect the oral mucosa (local immunity), but its permeability to viruses remains extremely high. Therefore, in a 2-3 year old child, stomatitis is more likely to be viral, in the vast majority of cases - herpetic1,3,4.
From 4 to 12 years of age, stomatitis in children is more often caused by allergic and autoimmune reactions. In particular, chronic aphthous forms of the disease occur during this period1.
Up to contents
Symptoms
Common symptoms of stomatitis are pain, burning, swelling of the mucous membrane and redness, and bad breath. Salivation also changes - it can be excessive or insufficient, with dry mouth. In some cases, there may be an increase in temperature and enlargement of the submandibular lymph nodes.
The types of stomatitis in children and treatment methods differ, as do the specific manifestations. For example, with aphthous stomatitis, only one large ulceration may appear, but with viral stomatitis, inflammation almost always takes the form of numerous elements or a rash merging into one focus.
Candidal stomatitis is characterized by the formation of a white or yellowish cheesy coating. It is easier to recognize traumatic stomatitis because it is preceded by damage or the source of injury is nearby - a chipped tooth or a rough filling.
Traumatic stomatitis
Inflammation of the mucous membrane in the mouth can be preceded by trauma: mechanical, thermal, chemical, radiation1,6.
Small children who put everything in their mouths can injure the mucous membranes with the sharp edges of toys or household items. Injuries often occur due to inept use of cutlery as a result of falls. In older children, stomatitis may be associated with a thermal burn, blows to the teeth, or the bad habit of chewing a pencil or pen. Sometimes the cause of inflammation is dental diseases and their treatment: sharp edges of damaged teeth and fillings, braces and aligners1.
When stomatitis develops in a child on the gum, on the inner surface of the cheek or in another place, the mucous membrane becomes red and swollen, and a painful erosion or ulcer may appear in the area of damage. Since there are many microorganisms in the mouth, there is always a risk of a bacterial or fungal infection1.
If the mucous membrane is constantly injured, painless whitish or whitish-gray layers may form on it.
In children under 1 year of age, stomatitis can be the result of using the wrong nipples: long, tight, irregularly shaped. The resulting Bednar aphthae are located in the area of the transition of the soft palate to the hard palate and are round erosions or ulcers1.
Treatment of traumatic stomatitis in children includes:
- elimination of traumatic factors;
- rinsing the mouth, irrigating the mucous membranes and treating wounds with drugs with an analgesic and antiseptic effect1.
Up to contents
Features of treatment
To diagnose a disease, only a visual examination is often sufficient, but in some cases laboratory diagnostics are required to determine the causative agent of the inflammatory process and the sensitivity of bacteria to antibiotics. Treatment should be carried out by a dentist, and the treatment regimen is developed individually, taking into account test results, the age and well-being of the child, the causes of the disease, the area of mucosal lesions and other conditions.
If the question of how to treat aphthous stomatitis in children is decided individually, then recommendations regarding eating behavior and hygiene are general for all cases. Such recommendations include the following:
- avoidance of too hot or cold drinks and foods;
- following a hypoallergenic diet;
- refusal of food that irritates the mucous membrane. This list includes fatty, salty and spicy foods, marinades, solid foods;
- adding pureed and soft foods to the menu. This includes cream soups, porridges, pre-boiled meat;
- drinking enough liquid;
- careful adherence to oral hygiene: using brushes with soft bristles, rinsing the mouth after each meal.
Local drug treatment consists of the use of such agents as:
- rinses or irrigation solutions (for children who do not yet know how to rinse their mouths) with an antiseptic effect;
- ointments and gels that stimulate the restoration of mucous membranes;
- drugs for pain relief and burning sensation.
It is important to test the product before use: apply a small amount to the crook of your elbow. If there is no redness, burning, or rash, we can say there is no allergy - the product can be used for treatment.
In some cases, systemic drug therapy is indicated. Your doctor may prescribe antihistamines to combat the allergic reaction and relieve swelling. In order to increase the resistance of the child's body, immunomodulators may be recommended. The decision on the need for antibacterial therapy is made in the case of an extremely severe course of the disease, a persistent increase in body temperature, and identification of a bacterial pathogen in a smear.
Elevated body temperature and pain are indications for symptomatic therapy. The doctor may recommend non-steroidal anti-inflammatory drugs in a dosage and form appropriate to the age of the young patient. Sometimes it is advisable to use suppositories if taking the medicine in the form of a tablet or syrup causes pain or anxiety.
Treatment of infants additionally includes disinfection of toys and teethers that the baby may put in his mouth. A nursing mother should pay attention to breast hygiene: thoroughly wash her breasts after feeding using warm water and special products.
Sometimes it is advisable to use folk remedies. Thus, rinsing the mouth with chamomile can soothe inflamed mucous membranes and speed up the healing process. However, it is important to remember that such prescriptions can only complement the main course of treatment. Don't forget to consult your doctor about the possibility of using them. Some herbs are strong allergens, so it is important to ensure that you are not hypersensitive to them.
Warming, the use of honey and alcohol tinctures are prohibited, as all this can lead to a worsening of the condition and lead to serious complications. It is better not to self-medicate, but to show the child to a qualified specialist.
Treatment of aphthous stomatitis in children usually takes no more than 7–12 days. It all depends on the state of the child’s immune system, the severity of inflammation, the number and depth of ulcers.
Viral stomatitis
About 80% of all stomatitis in children is caused by herpes viruses3,5. In approximately 70% of cases, the disease develops in children aged 1 to 3 years3,4.
The disease can occur in mild, moderate and severe forms.
With mild herpetic stomatitis, the general condition is practically not disturbed. Body temperature does not exceed 37-37.50 C. Symptoms of inflammation are limited to swelling of the gums and usually the simultaneous appearance of single painful herpetic blisters and erosions on the mucous membrane (no more than 6). After 1-2 days, the contours of the lesions are blurred, the rashes turn pale, and the erosions heal without scarring3.
With moderate stomatitis, the child’s temperature reaches 38-390 C and lasts until rashes continue to appear. General intoxication manifests itself in the form of weakness, headache, nausea. The child becomes capricious, lethargic, refuses to eat and play3.
As the temperature rises, the oral mucosa becomes red and swollen, and the gums begin to bleed. The number of herpetic elements reaches 20-25, repeated rashes are accompanied by fever3.
Severe stomatitis in children looks like a common acute infectious disease and is accompanied by severe intoxication: fever 39-400 C, chills, headache, aching muscles and joints, heart rhythm disturbances, nosebleeds, nausea and vomiting. The number of herpetic elements can reach 100; they are located not only in the mouth, but also on the skin of the face, on the eyelids and conjunctiva of the eyes, and earlobes. In addition, upper respiratory tract symptoms may be present.3
Treatment includes treating the affected area with painkillers and antiseptic drugs, antiviral therapy, drinking plenty of fluids, a balanced diet and proper nutrition3,5.
Up to contents
Causes
Viral stomatitis in childhood develops due to various infections, since the baby has an underdeveloped immune system. He does not have time to recover from his previous illness. It also easily becomes infected from a patient with stomatitis. The situation is worsened by a lack of nutrients and vitamins in the body.
The disease in children is caused by the following pathogens:
- flu;
- HIV;
- mononucleosis;
- measles;
- papillomavirus;
- ARVI;
- enterovirus;
- chicken pox;
- herpes.
Most often, herpes is the causative agent of this disease; it accounts for up to 80% of all cases. Most of these viruses are persistent intracellular parasites. Therefore, this disease often becomes chronic. With this form, there is an alternation of exacerbations and remissions. The acute form can result in the formation of a carrier state, in which the pathogen remains in the cells, but there are no symptoms of the disease.
Most often, the infection affects children under four years of age. But it affects older children and teenagers.
The reasons why this happens are:
- undeveloped immune system;
- insufficient oral hygiene;
- weakness of local immunity;
- injuries to the gums and oral mucosa;
- general weakening of the body after an illness;
- long-term use of certain drugs (glucocorticoids, antibiotics, cytostatics).
Parallel inflammatory processes in other organs and systems also contribute to maintaining the infectious process in the mouth of children.
Candidal stomatitis
In 80% of healthy children, Candida fungi can be found in the oral cavity. They get there during childbirth, from nipples and pacifiers, from care products, in contact with the mother's skin, with food during eating and usually do not cause any problems. Candidal stomatitis, or thrush, occurs when immunity decreases1.
Predispose to the disease:
- prematurity and postmaturity;
- developmental defects and concomitant diseases;
- treatment with antibiotics and hormones;
- artificial feeding;
- poor care and poor feeding hygiene;
- Using the wrong nipples1.
What does candidal stomatitis look like? In children's mouths, whitish or whitish-gray dotted formations appear on the reddened mucous membrane. They merge into films of a cheesy nature; when the films are rejected, bright red painful erosions are formed. Because of the pain, the baby becomes restless, cries often, sleeps poorly, and refuses to eat1.
In severe cases of candidiasis, a cheesy coating may appear on the palate and on the lateral surfaces of the tongue, on the tonsils and the back wall of the pharynx - candidal tonsillitis and pharyngitis develop1.
If your child has a fungal infection, you should always consult a doctor; he will tell you how and what to treat the mucous membrane with candidal stomatitis, so that the child does not have complications and recovers faster. Treatment, as a rule, involves treating the oral cavity with drugs with antifungal activity (chlorhexidine, hexethidine). In severe cases of the disease, antifungal agents, probiotics and immunomodulators are prescribed1.
Up to contents
Treatment of stomatitis using traditional medicine
Medical staff at children's clinics say that when stomatitis is detected, it is best to consult with your doctor. Only a specialist can identify what stage the disease is at and prescribe treatment. However, there are situations when the clinic is not open (for example, evening hours and night time), and the child is very sick and does not feel well. If stomatitis is detected at first, you can resort to traditional medicine. There is no need to think that the disease will go away on its own. If the infection is not eradicated, the child will get even more sick.
In case of stomatitis, the oral cavity should be wiped with a bandage containing a soda solution. Plaque in the mouth is removed with a bandage or a piece of gauze, thereby eliminating the infection. Making a soda solution is very easy: add one teaspoon of soda to one glass of water and mix thoroughly. Before use, the liquid should be stirred so that the soda does not remain at the bottom of the glass. Using soda, you can thoroughly disinfect the oral cavity and mucous membrane, while removing plaque.
You can also try wiping the inside with slimy brilliant green. Procedurally, you need to do the same as with a soda solution. Then soak in brilliant green and thoroughly wipe the child’s mouth.
For older children, you can prepare herbal infusions and give them a mouth rinse after eating. In this case, food particles will be removed, and the mucous membrane will not burst. You can rinse with a chamomile solution, which quickly removes the inflammatory process. It is not uncommon for people to use strong green tea, which is also used as a mouth rinse. This procedure should be carried out several times, and it is not at all necessary to do it after meals.
It is sometimes quite difficult to persuade young children to rinse their mouths, especially if they experience pain there. In this case, they may like rose syrup, which also has a positive effect on eliminating infections in the mouth. You can make this syrup yourself using rose petals, sugar and water. You can easily prepare a decoction of oak bark at home. Herbs you can choose from are burdock, sage, and yarrow. You can prepare a mixture of these herbs and rinse your mouth with the tincture several times a day.
You can also use aloe, which you can simply chew. If a child cannot swallow such a plant, then holding it in his mouth will be enough. Aloe will taste good together with a little honey. However, we must remember that using large amounts of honey for stomatitis can only worsen the disease. When a child is ill, you should use only high-quality products without acid and harsh sensations, which will not cause allergies and irritation of the mucous membrane. It is advisable to limit yourself to a set of dishes that were pleasant to the child and did not cause him discomfort.
Allergic stomatitis
Allergic damage to the mucous membrane most often occurs in the form of contact stomatitis and chronic aphthous form of the disease1.
Allergens can include medications, food products, varnishes and paints that coat toys, toothpastes, mouth rinses, chewing gum, and dental metals included in braces1,2.
With allergic stomatitis in children, erosions and ulcers may appear in the mouth, but more often the matter is limited to redness and swelling of the mucous membrane1.
Treatment is avoiding contact with the allergen, rinsing or irrigating the mouth with antiseptic solutions to prevent infection. If necessary, doctors recommend taking antihistamines1,2.
Chronic recurrent aphthous stomatitis often occurs in schoolchildren and adolescents due to allergies2. In addition, its development can be provoked by diseases of the gastrointestinal tract, upper respiratory tract infections, disorders of the nervous system, and hypovitaminosis1,2.
With aphthous stomatitis in children, itching and burning first appear in the oral cavity. The mucous membrane at the site of the lesion becomes red and swollen, then an aphtha forms on it - a round or oval erosion 0.5-1 cm in diameter rising above the surrounding tissues with a red rim along the periphery and a bottom covered with a grayish-white coating. Aphthae are extremely painful, and if many of them form, they cause significant distress to the child1,2.
How many days does aphthous stomatitis last in children? With a mild course of the disease, the elements of inflammation persist for up to 5-7 days, then they heal without scar formation2 and do not appear for quite a long time. However, in severe cases, aphthae can occur constantly, and then many elements of inflammation can be found on the mucosa at different stages of development1,2.
To treat aphthous stomatitis, doctors use:
- antihistamines;
- immunomodulatory drugs;
- vitamins;
- probiotics2.
As a local therapy, it is recommended to treat the mucous membrane with drugs with analgesic, antiseptic, proteolytic (protein-breaking), anti-inflammatory and regenerating effects2.
Up to contents
Treatment of herpetic stomatitis
Therapy includes the local application of gels with an anesthetic effect, which include lidocaine or articaine (they should be generously lubricated in the mouth).
All kinds of analgesics are prescribed internally, such as ketorol, and, of course, antivirals: Zovirax or acyclovir. Among anti-inflammatory drugs, it is better to choose Cholisal or Metrogyl gel.
Recurrent chronic herpes
In the absence of proper treatment, acute stomatitis becomes chronic - recurrent herpes. The systematic manifestation of single or multiple rashes on the lips, in the mouth area - on the mucous membrane of the eyes, on the palate, genitals and wings of the nose cannot be ruled out.
The appearance of herpetic type rashes is accompanied by a burning sensation. Such a blistering rash subsequently forms merged erosions.
While eating, patients complain of pain and discomfort in the mouth.
The main feature of herpes infection is the likelihood of lifelong infection with the virus.
Hexoral in the treatment of stomatitis
For local treatment of stomatitis in children, drugs from the HEXORAL® line can be used.
For irrigation of the oral cavity, the doctor may recommend aerosol HEXORAL® based on hexethidine, which has antiseptic properties7. Thanks to the fine spray, the drug is evenly distributed over the entire surface of the mucosa7. A solution of HEXORAL®8, similar in composition, is intended for rinsing the mouth. Both medications can be used to treat children 3 years of age and older.
Mint-flavored lozenges HEXORAL® TABS based on chlorhexidine and benzocaine may be suitable for boys and girls over 4 years of age9.
For patients with stomatitis over 6 years of age - HEXORAL® TABS CLASSIC based on the antiseptic amylmetacresol. The assortment includes tablets with lemon, orange, black currant, lemon and honey flavors10.
HEXORAL® TABS EXTRA may be suitable for adolescents aged 12 years and older. The lidocaine it contains can relieve even severe pain11.
The information in this article is for reference only and does not replace professional advice from a doctor. To make a diagnosis and prescribe treatment, consult a qualified specialist.
Up to contents
Diagnostics
If there is a suspicion of damage to the mucous membrane in the mouth, only a doctor, pediatrician or pediatric dentist should make a diagnosis and examine a child. It is important to identify the cause of the disease in order to prescribe effective treatment. Identifying the cause of the disease does not present any difficulties. This pathology is detected during examination due to the characteristic clinical picture, the presence of rashes, and signs of inflammation in the mouth. In addition to an examination to clarify the nature of the disease, the doctor prescribes a general blood and urine test. In severe cases, tissues of the affected mucous membrane are examined to identify the type of pathogen. For this purpose, washouts and scrapings from erosions and ulcers are taken.
The following methods are used to identify the type of virus:
- immunofluorescence method;
- PCR;
- RSK;
- ELISA.
In order to prescribe effective therapy, especially in severe cases, identification of the type of pathogen is required.
Literature
- Khomenko L. A. Therapeutic dentistry of children. Textbook for university / ed. 2007 – pp. 643-722.
- Ismailova G. T. Chronic recurrent aphthous stomatitis // Bulletin of surgery of Kazakhstan. - 2011. - No. 4. — P. 124-125.
- Drobotko L.N., Strakhova S.Yu. Acute stomatitis in children // Issues of modern pediatrics. - 2010. - T. 9. - No. 2. - P. 146-149.
- Suerkulov E. S., Yuldashev I. M., Mamyraliev A. B., Toktosunova S. A., Tsepeleva A. S., Sooronbaev A. A. Prevalence and structure of the incidence of stomatitis in children // Bulletin of Science and Practice. 2022. T. 4. No. 11. — P. 91-96.
- Suerkulov E. S., Yuldashev I. M., Mamyraliev A. B., Zhumashova N. K., Yuldasheva G. I. Complex therapy of inflammatory diseases of the oral mucosa in children // Bulletin of Science and Practice. 2022. T. 5. No. 5. — P. 96-104.
- Pankrusheva T.A., Maravina I.N., Chekmareva M.S. Research on the development of the composition and technology of tablets for the treatment of stomatitis // Scientific result. Medicine and pharmacy. – T.4, No. 1, 2022. – P. 78-87.
- Instructions for medical use of the drug HEXORAL® aerosol: , .
- Instructions for medical use of the drug HEXORAL® solution: , .
- Instructions for medical use of the drug HEXORAL® TABS: , .
- Instructions for medical use of the drug HEXORAL® TABS CLASSIC: , .
- Instructions for medical use of the drug HEXORAL® TABS EXTRA: , .
Up to contents
Symptoms of stomatitis in children
The first symptom of stomatitis in a child that can be seen by relatives is dry, flaky lips. A small white coating may form on the tongue, which over time can spread throughout the mouth. Infants may well become infected with fungal stomatitis, which manifests itself in the form of small white spots. By their nature, the spots resemble milk that has curdled on the tongue. Sometimes such stomatitis can occur as a result of long-term treatment with antibiotics. That is why doctors do not recommend long-term use of such drugs.
An increase in temperature is one of the primary symptoms, which may also indicate that the child is sick. Lack of appetite, lethargy, whims - these are the first symptoms that need to be responded to in terms of diagnosing the oral cavity in a child.
Prevention
It is not possible to completely prevent the development of this infection in a child. Most people are already infected with viruses at birth, but it is quite possible to reduce the incidence of the disease.
To do this, the following measures are used:
- if one of the adults is infected, they should not be allowed to contact the child;
- choose a group in kindergarten with a small number of children;
- If possible, do not attend mass events during epidemics;
- it is necessary to harden the child (walk barefoot at home, go to the pool);
- stop bad habits (sucking fingers, toys, other objects);
- thoroughly wash and treat the child’s toys and dishes;
- treatment of all surfaces in the apartment using antiseptics.
Infectious stomatitis in children is a rather unpleasant disease. If you follow all the doctor’s recommendations and preventive measures, you can minimize the occurrence of this disease in your baby.
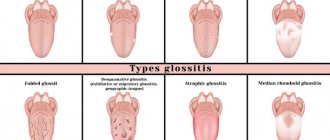
Types of disease
- Bacterial stomatitis. It is diagnosed when the oral cavity is damaged by microorganisms, most often streptococci and staphylococci.
- Herpetic stomatitis. The causative agent is the herpes virus. Small blisters form in the oral cavity, which, after opening on their own, transform into painful ulcers.
- Aphthous stomatitis. It can be a complication of ENT diseases or occur against the background of decreased immunity. It is characterized by the formation of aphthous erosive areas in the mouth.
- Candidal stomatitis. A disease caused by fungi of the genus Candida. The characteristic symptoms include a cheesy coating on the tongue, lips, and cheeks.
- Ulcerative stomatitis. It usually occurs with extensive inflammation of the mucous membrane and the formation of painful ulcers on its surface.
- Allergic stomatitis. The main reason is an allergic reaction of the mucous membrane to food, pollen and other allergens. The disease is one of the symptoms of allergies.
Rarer types of stomatitis are also known - radiation (a consequence of radiation sickness) and chemical (a consequence of acid burns).