Fluorosis is a disease of tooth enamel associated with prolonged exposure to excessive amounts of fluoride. It can be endemic and occupational in nature - develop in connection with living in a region where drinking water contains a lot of fluoride or be associated with working conditions and the amount of fluoride in the air.
Endemic fluorosis is common in regions where the amount of fluoride in a liter of drinking water exceeds 1.5 mg. The occupational form of the disease is much less common, usually among employees of the aluminum industry.
Causes of fluorosis
What are the causes of dental fluorosis? The main etiological factor is a long-term increased intake of fluoride during tooth development. The main source of fluoride is drinking water. An adult consumes about 3 mg of fluoride per day: from food - 0.5-1.1 mg and from water - 2.2-2.5. Fluorides dissolved in water are absorbed much better than food fluorides. Therefore, when drinking water with a concentration exceeding 1.5-2 mg/l, mild fluorosis may develop. When the fluoride concentration is above 6 mg/l, hard dental tissues begin to break down. Also, dental fluorosis can occur due to working in enterprises where the air contains a lot of fluoride - occupational fluorosis. This form of the disease is not always accompanied by the appearance of stains on the teeth.
Fluorosis in children
In childhood, the development of the skeletal system occurs. Excessive intake of fluoride during bone formation can contribute to disruption of the structure of the protein matrix of bone tissue and its mineralization. Fluorine binds to calcium, forming the compound CaF2, which is weakly bound to the enamel. The structure of the enamel becomes loose, its optical properties change. Fluorosis in children occurs during the eruption of permanent teeth. Such children most often live or lived until they were 3-4 years old in an area with an increased concentration of fluoride in the water. Milk teeth are rarely affected by fluorosis, since the rudiments of temporary teeth are formed during intrauterine development. The placenta retains excess fluoride. Cases of fluorosis in primary teeth are rare and are observed only in areas where the concentration of fluoride in water is extremely high.
The disease is usually divided into forms
Endemic dental fluorosis (a disease peculiar to a particular area or a particular group of people). It occurs in areas where drinking water (namely, with it the main amounts of fluorine enter the body) contains excess fluorine, according to Russian standards - more than 1.5 mg/l.
Sporadic (irregular) form . It occurs even with normal levels of this microelement in drinking water. The reasons are not yet known.
Professional (industrial) uniform. In people employed in a number of industries and constantly in contact with fluorine compounds (for example, aluminum, cryolite production).
Iatrogenic (caused by improper actions) form. For example, long-term and excessive use of fluoride-containing drugs.
Pathogenesis of fluorosis
The pathogenesis of fluorosis is of interest to many researchers. During the period of tooth formation, fluoride intoxication provokes a disruption of the structure of the protein matrix and subsequent mineralization of tissues. The crystal lattice loses order due to the formation of CaF2 instead of hydroxyfluorapatite. This compound weakly binds to the enamel. Ameloblasts are sensitive to excess fluoride. Excess fluoride leads to cell destruction and stops the development of enamel prisms. This causes a change in its optical properties - the appearance of dull and dark spots, up to the destruction of the enamel. In addition, fluorine reduces phosphatase activity, which leads to impaired mineralization. When the optimal fluorine load is chronically exceeded, systemic fluorosis develops: fluoride accumulates in bone tissue, cartilage and ligaments. Joint mobility is limited, skin aging, skeletal growth stops, and hormonal and immune activity decreases. The more fluoride enters the body, the more severe the disease. Formed tooth enamel is not affected by fluorosis even with prolonged consumption of drinking water with a high concentration of fluoride. But if this value exceeds 6 mg/l, changes may occur in permanent teeth.
Teeth whitening for fluorosis
Is it possible to whiten teeth with fluorosis?
Teeth affected by fluorosis do not whiten well, and in some cases they cannot be whitened at all (with erosive-destructive fluorosis). This is due to changes in the structure of dentin and enamel, which turn out to be oversaturated with fluoride, which leads to the appearance of stains that cannot be whitened.
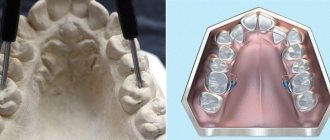
The streaked and spotted forms are bleached more or less successfully. Using laser whitening and remineralization, you can disguise whitish streaks on the tooth surface. It is completely impossible to change color in the chalky-mottled and erosive form. Dark fluorescent stains on teeth can only be removed with the help of dentures, crowns, veneers, and in some cases lumineers.
Classification of fluorosis
The WHO classification of fluorosis includes five degrees of severity: I - very mild - enamel of normal color, almost without changes. II – mild – enamel damage in the form of white stripes and small spots, occupying less than 25% of the crown area. III – moderate - pigmented stripes and spots occupy no more than 50% of the area. IV – moderate severity – the crowns of the teeth are yellow or brown. The enamel becomes dull and there are specks on the entire crown. V – heavy – the enamel is partially destroyed, pits and erosions appear.
Forms of fluorosis
Forms of fluorosis according to V.K. Patrikeev: • Line form - the appearance of strokes - subsurfacely located chalky strips of enamel. More often found on the vestibular surface of the incisors. Corresponds to mild fluorosis (WHO). • Spotted form - multiple chalky spots without stripes. The enamel in the area of the stain is smooth and shiny. Corresponds to a moderate degree of fluorosis. • Chalky-mottled form - the enamel of the entire tooth is matte in color with clear pigmented speckled spots. The bottom of such specks is dirty gray/brown. Corresponds to moderate fluorosis. • Erosive form - pronounced pigmentation + erosion. Deep defects are possible. The enamel wears off quickly, subsequently exposing the dentin. Corresponds to severe fluorosis. • Destructive form - violation of the shape of the crown due to erosion and abrasion. The teeth are more fragile, and part of the crown may break off.
Subtleties of differential diagnosis of fluorosis
It is very important to distinguish fluorosis from enamel hypoplasia, especially from its patchy form. Chalky spots in both diseases are located symmetrically, in areas of the crown that are not typical for caries. As a rule, these are the labial and lingual surfaces, cusps and cutting edge. With fluorosis, they have a pearly white tint, are shiny, do not cause pain during probing, and gradually turn into healthy enamel.
With hypoplasia, the spots are white and dense, also shiny, but with clear boundaries. Under the influence of UV rays, with fluorosis, chalky spots give a light blue glow (pigmented ones - red-brown), with hypoplasia - light yellow. Fluorosis is not prone to changes in spots, while formations with hypoplasia often require treatment for caries in children, since they change and progress.
Fluorosis Clinic
The clinical picture of fluorosis is similar for all forms of the disease. The first sign is mottling of the enamel. Soon after teething, the color of the teeth changes. The enamel loses its transparency and becomes matte with yellowish or brown tints. Spots and stripes of various sizes appear on the crowns. The severity of the disease is determined by their size, color and number.
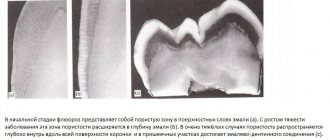
The nature of the changes depends on the clinical form of the disease. Mild and moderate fluorosis is characterized by Gunter-Schröger stripes, Retzius lines, and bulges and depressions are noticeable on the surface of the enamel. The enamel-dentin border has a jagged shape. There is an increase in interprismatic spaces due to resorption of enamel prisms.
In the area of spots, enamel mineralization is reduced. This explains pigmentation: dyes penetrate into areas of increased permeability of the enamel. Pigmentation zones contain large quantities of nitrogenous substances.
Electron microscopy of tooth enamel with mild fluorosis reveals clear structures of hydroxyapatite crystals. In severe cases, clarity is impaired.
Another feature of severe fluorosis is that different groups of teeth in one patient are affected by different forms of the disease. At the same time, one form or another persists throughout life and does not transform into another even with an increased amount of fluorine in the water. At the onset of the disease, fluorosis most often appears on the upper incisors and premolars, and less often on the lower incisors and molars.
Differential diagnosis of fluorosis
Differential diagnosis of mild fluorosis is carried out with initial caries. Caries is characterized by a single spot, while fluorosis is characterized by multiple spots. Also, unlike caries, fluorosis appears from the moment teeth erupt.
The average degree of fluorosis is similar to enamel hypoplasia. The difference is that with hypoplasia, single teeth or groups of teeth are affected, and with fluorosis, the entire dentition is affected.
Severe fluorosis resembles hereditary amelogenesis imperfecta. In this case, anamnesis is important: the development of amelogenesis does not depend on the fluoride content in the water.
Symptoms and manifestations
Endemic dental fluorosis manifests itself as white spots or characteristic stripes on the enamel. As the disease progresses, they acquire a yellow or even brown tint. The incisors of the upper jaw are most often affected, but at high concentrations of fluoride, damage to all teeth occurs. Increased abrasion of the enamel is observed, chips and erosions form. Symptoms depend on the form of the disease.
Line
This form of the disease is characterized by the appearance of white stripes on the outer surface of the incisors. Sometimes they are pronounced, but more often they are noticeable only when the enamel surface dries. In some cases, the stripes merge into large spots, but the doctor will detect separate stripes in the structure of the spot.
Spotted
With this form, multiple white spots appear that merge with each other. The surface of the stain is shiny and smooth, without roughness. There are no clear boundaries of the stain - it smoothly transitions into healthy areas of the enamel.
Chalky mottled
With this form of enamel fluorosis, a matte tint appears on the entire surface of the hard tissues of the tooth. Clearly defined spots and dots appear on the surface. In some cases, the enamel becomes yellow. In addition, areas of destruction may be observed on the teeth: speckled depressions with a diameter of up to 1.5 mm and a depth of up to 0.2 mm. The bottom of such depressions is pigmented.
This form is characterized by increased abrasion of the enamel, which exposes dentin - the deeper tissues of the tooth, which have a dark brown color. Sensitivity of teeth when dentin is exposed is pronounced.
Erosive
This form is distinguished by the presence of larger areas of enamel destruction - erosions. In the area of such a depression, there is no enamel at all, and increased abrasion is observed on the chewing surfaces of the teeth.
Destructive
In the destructive form of the disease, abrasion and erosion occurs not only of the enamel itself, but also of other hard tooth tissue - dentin. Teeth become brittle, large chips occur, and the shape of the crowns is disrupted. The body strives to prevent the opening of the tooth cavity by forming replacement dentin. This is a severe form of the disease that can develop in regions where drinking water contains at least 10 mg of fluoride per liter of water.
Treatment of fluorosis
The method of treating fluorosis depends on the stage of the pathological process.
Bleaching for fluorosis
Treatment of mild to moderate fluorosis is symptomatic. Whitening for dental fluorosis is carried out with solutions of inorganic acids. To eliminate pigmentation, acid is used followed by retherapy (10% HCI + 10% calcium gluconate solution). 1. Isolation of the working field from saliva. 2. Drying the tooth and treating it with a 20-30% solution of hydrochloric/phosphoric acid - 2-3 minutes. 3.Washing off the acid. The tooth should not come into contact with saliva. 4.Treatment of the tooth with a 10% solution of calcium gluconate - 10-15 minutes.
The procedure is repeated at the next visit after 1-2 days. But now only discolored areas of enamel are treated with an acid solution.
During the whitening period, calcium gluconate and glycerophosphate are prescribed orally. The course of treatment is 10-15 procedures. The effect is observed after 6-8 months. A toothpaste containing fluoride is recommended for brushing your teeth.
The technique is difficult to perform and quite unsafe. The treatment effect is not permanent. A repeated course is carried out when new spots appear.
Grinding the enamel
You can grind the enamel using a paste containing hydrochloric acid, carborundum, and silicon gel. The crown is polished, and then a tampon soaked in perhydrol is applied. Then the tooth is irradiated with a quartz lamp for 3-4 minutes and fluoride preparations are applied.
In the treatment of severe fluorosis, aesthetic restoration and prosthetics are indicated.
Clinical researches
Clinical studies have proven that regular use of professional toothpaste ASEPTA REMINERALIZATION improved the condition of the enamel by 64% and reduced tooth sensitivity by 66% after just four weeks.
In addition, it has been proven that in order to eliminate increased sensitivity of teeth in people suffering from type 2 diabetes mellitus, long-term use of the domestic toothpaste “Asepta plus remineralization” is advisable, which is important to consider in the complex treatment of the dental pathology in question to ensure psychological balance, quality of life, restoration of chewing function and satisfaction with treatment of such patients.
Sources:
- Features of personal response in the prevention and treatment of hypersensitivity of teeth against the background of type 2 diabetes mellitus A.K. YORDANISHVILI, Doctor of Medical Sciences, Professor, North-Western State Medical University named after. I.I. Mechnikov, Military Medical Academy named after. CM. Kirova, International Academy of Sciences of Ecology, Human Safety and Nature, N.A. UDALTSOVA, Candidate of Medical Sciences, Associate Professor, St. Petersburg State University of the Government of the Russian Federation; dental clinic No. 29, Frunzensky district of St. Petersburg, O.V. PRYSYAZHNYUK, head. surgical department No. 2, dental clinic No. 29, Frunzensky district of St. Petersburg
- Report on the determination/confirmation of the preventive properties of personal oral hygiene products “ASEPTA PLUS” Remineralization doctor-researcher A.A. Leontyev, head Department of Preventive Dentistry, Doctor of Medical Sciences, Professor S.B. Ulitovsky First St. Petersburg State Medical University named after. acad. I.P. Pavlova, Department of Preventive Dentistry
- Report on determining/confirming the preventive properties of toothpaste “ASEPTA PLUS” GENTLE WHITENING” Author: doctor-researcher A.A. Leontyev, head Department of Preventive Dentistry, Doctor of Medical Sciences, Professor S.B. Ulitovsky First St. Petersburg State Medical University named after. acad. I.P. Pavlova, Department of Preventive Dentistry
Prevention of fluorosis
Fluorosis is a chronic disease and most often endemic, so fluorosis prevention should be carried out in places with a high fluoride content in the water. Especially if the fluorine content exceeds 2 mg/l. Intensive prevention should be carried out during the period of formation and mineralization of teeth.
Preventive measures for fluorosis are divided into collective measures and individual preventive measures. To prevent fluorosis, it is necessary to reduce the fluoride content in water by defluoridating the water or changing the water source. There are various methods of water purification.
Individual prophylaxis begins from the moment the child is born until the end of mineralization of permanent molars. Those. Intensive prevention should be carried out during the period of formation and mineralization of teeth. It is advisable to avoid artificial feeding and early complementary feeding.
Also, a balanced diet can reduce the negative effects of fluoride on the body. Vitamins C, D, calcium reduce the likelihood of fluorosis. You should limit your consumption of foods containing fluoride: sea fish, animal oils, spinach.
Symptoms of disease development
Common symptoms of fluorosis include:
- Loss of the natural shade of tooth enamel.
- The appearance of white spots, yellow or yellow-brown spots, or the appearance of any pigmentation on the surface of the teeth.
- Pigmentation may also appear on the lingual part of the mouth.
- Tooth enamel loses sensitivity to any type of irritant.
- The enamel wears off over time.
- Possible damage to bone tissue, muscles, nervous system and some internal organs. These symptoms usually appear at an advanced stage of the disease.