Ultrasound of the salivary glands: what are the capabilities of this diagnostic method?
Saliva, one of the most important components of the digestion process, is produced by special glands. What diseases are typical for the salivary glands? How can ultrasound help in their diagnosis? How is this procedure carried out?
These and other questions are answered by Yulia Vasilievna Safronova, ultrasound diagnostics doctor at Clinic Expert, Smolensk.
— Among the exocrine glands, a special place is occupied by the glands that produce saliva, one of the important biological fluids of the body. Yulia Vasilievna, tell us how many salivary glands are in the human body and where are they located?
— There are three pairs of large salivary glands in our body: parotid, submandibular and sublingual. The parotid muscles are located behind the lower jaw, at the level of the earlobe. The submandibular salivary glands lie among the muscles of the floor of the mouth, and the sublingual glands lie in the thickness of the muscle tissue under the tongue. In addition, in the tissues of the lips, cheeks, and palate there are many small salivary glands. All of them secrete saliva, which a person needs for the normal digestion process.
— What diseases can affect the salivary glands?
- For example, inflammatory ones are acute and chronic sialadenitis, abscesses, phlegmons. The salivary glands can be affected by tumors (benign and malignant) and autoimmune processes. Since these glands have excretory ducts, sialolithiasis (stones in the salivary glands) can develop. In addition, children sometimes have congenital anomalies in the development of glands, their ducts, or the complete absence of a gland (or glands).
— What diagnostic methods can be used to examine the salivary glands?
- Parotid and submandibular salivary glands are assessed using ultrasound, magnetic resonance imaging and computed tomography. The sublingual glands are not visible on ultrasound, so they are examined using CT, MRI, or contrast-enhanced X-ray. There are also methods for radioisotope diagnostics of the salivary glands, but they are not widely used due to their toxicity.
Focal lesions of the small salivary glands are more often detected during a dental examination.
— Let's talk in more detail about ultrasound examination. What does an ultrasound of the salivary glands show?
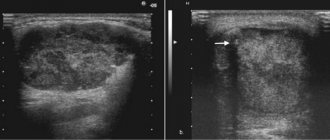
— During an ultrasound examination, we evaluate the structure of the salivary glands and their size. We also see the blood supply to the gland, the condition of its ducts. Ultrasound helps detect inflammation, stones, and neoplasms in the salivary glands.
— To whom and in what cases is this study prescribed?
— Ultrasound diagnostics is, as a rule, the first stage of the study of the salivary glands. Dentists, therapists or ENT doctors refer patients for an ultrasound of the salivary glands if patients complain of pain in the submandibular or parotid region, difficulty swallowing, increased or decreased salivation, or the presence of compactions in the areas of projection of the salivary glands. Sometimes patients come forward on their own.
I would like to emphasize that ultrasound is a kind of screening method for studying the salivary glands. For a more accurate diagnosis, it is sometimes necessary to refer patients for computed tomography or magnetic resonance imaging.
— Yulia Vasilievna, please tell us how an ultrasound of the salivary glands is done
— In the classic version, the patient lies with his back on the couch, and a cushion is placed under the neck. The patient raises his chin high. The doctor applies a special gel to the area under study and, using a linear sensor, examines the submandibular, parotid area, where the salivary glands and adjacent lymph nodes are located. The procedure is carried out on both sides. During the study, the size of the glands, the state of their structure, and the patency of the ducts are recorded. All this data is recorded in the conclusion that the patient receives at the end of the study. The entire procedure takes on average up to 15 minutes.
— Are there age restrictions for this research method?
— No, because ultrasound is a safe method. Therefore, ultrasound of the salivary glands can be performed on both infants and elderly people.
— Are there any contraindications to performing an ultrasound of the salivary glands?
— There are no absolute contraindications. We do not perform the procedure if there are pustular skin lesions or open wounds in the study area.
Interviewed by Sevilya Ibraimova
You can sign up for an ultrasound of the salivary glands here. ATTENTION: the service is not available in all cities
The editors recommend:
MRI of the salivary glands: when is it necessary?
For reference:
Safronova Yulia Vasilievna
In 2006 she graduated from the Smolensk State Medical Academy 2006-2007. – clinical internship in therapy In 2009, she received a certificate in ultrasound diagnostics and minimally invasive technologies under ultrasound guidance. In 2013, she defended her PhD thesis in therapy. Currently, she is an ultrasound diagnostic doctor at Clinic Expert, Smolensk
Physiology of excretion
EXCRETORY (EXCRETORY) FUNCTION OF SALIVARY GLANDS. PARTICIPATION OF SALIVARY GLANDS IN MAINTAINING HOMEOSTASIS OF THE ORGANISM.
Excretory function of the oral cavity
due to the fact that some metabolites, salts of heavy metals and some other substances are released into the oral cavity. The release of metabolic products occurs both with saliva and the mucous membrane of the entire surface of the mouth.
If the excretory function of the main excretory organ (kidneys) is insufficient, the salivary glands are included compensatory in the excretion process. At the same time, due to the release of a large amount of urea with saliva, which, under the influence of salivary substances, turns into ammonia, the patient constantly experiences bad breath. With gout, uric acid is released into the saliva, and with jaundice, components of bile are released.
Analyzers (sensory system).
SENSORY FUNCTION OF THE ORAL CAVITY, ITS FEATURES. CONCEPT OF THE ORAL ANALYZER (I.P. PAVLOV).
Based on the nature of the information that enters the central nervous system from the oral cavity, at least six types of sensitivity are distinguished: gustatory, cold, thermal, tactile, pain and proprioceptive.
According to the specifics of their functioning, numerous receptors in the oral cavity can be divided into three groups
: chemoreceptors
(taste),
somatosensory
receptors (tactile, heat, cold, pain) and
proprioceptors
. Each of these groups is the beginning of a corresponding analyzer.
Concept of the oral analyzer . A set of receptor formations located in the oral cavity, and giving a person an idea not only of the chemical properties of food (its taste qualities) but also of the physical properties of the food taken (its temperature, density, mass, volume), as well as the conductive central conductors serving these receptors nervous structures, I.P. Pavlov suggested calling it an oral analyzer.
However, the structure and functional features of taste, tactile and temperature reception are very different. Therefore, it is advisable to study them separately, remembering, however, that when food enters the oral cavity, a person receives an integral assessment of all its properties, and only after that the question of whether to continue processing it or reject it and spit it out is decided.
PHYSIOLOGICAL CHARACTERISTICS OF TASTE ANALYZER. MODERN IDEA OF TASTE PERCEPTION. METHODS FOR STUDYING THE TASTE ANALYZER. DETERMINATION OF TASTE SENSITIVITY THRESHOLDS.
Taste reception in vertebrates is associated with the functioning of taste buds, or bulbs - special epithelial formations located in the thickness of the multilayered epithelium of the tongue. The cells of the taste buds pass through the entire thickness of the epithelium, perpendicular to it, reaching the basement membrane with their basal ends, and in the apical part forming a taste canal connected to the oral cavity through the taste pore. The taste bud includes 30-80 flattened, elongated spindle-shaped cells, closely adjacent to each other like orange slices.
The epithelial structures of the taste bud are closely related to the nervous elements. After cutting the fibers innervating the taste bud, its complete degeneration and disappearance is observed. Regeneration of the nerve leads to restoration of the taste bud.
In humans, taste buds are located mainly on the dorsal surface of the fungiform, in the leaf-shaped grooves, grooves of the valvate papillae of the tongue, and also in much smaller quantities in the mucous membrane of the palate, pharynx, larynx, tonsils, and velum. Each fungiform papilla contains 3-4 bulbs. In children, taste buds are more widely distributed than in adults, throughout the hard and soft palate, on the larynx, epiglottis, and fungiform papillae in the middle of the back of the tongue. An adult has 9-10 thousand taste buds. After 45 years, some of the taste buds atrophy.
It has been shown that the number of taste buds is related to the nature of nutrition: predators have fewer of them than herbivores.
In most vertebrates and humans, signaling about the chemical composition of substances in the oral cavity enters the central nervous system through the fibers of the facial, glossopharyngeal, vagus and trigeminal nerves. All taste fibers entering the brainstem end in the nucleus of a single fascicle running throughout the entire length of the medulla oblongata in the dorsolateral part of the tegmentum. The question of the localization of taste centers in the cortex has not been completely resolved, but it is generally accepted that the following areas of the cortex are most closely related to taste sensitivity: the lower end of the central gyrus near the Sylvian fissure, the proto-insular region and the tegmental region. Changes in taste are also observed with damage to the base of the temporal lobe, opercular zone, etc.
The sensation of taste occurs only when the substance that comes into contact with the taste bud is dissolved in water. Thus, dry sugar placed on a tongue dried with filter paper appears tasteless.
Under natural conditions, the sensation of taste is very complex, and depends on the combination of four primary taste qualities that arise when taste buds are irritated - sweet, salty, bitter and sour.
.
So far, no strict correspondence has been found between the chemical structure of a substance and the sensation it causes when exposed to the taste buds. The most clearly defined class of irritants causing the sensation of sour taste
. These include almost all acids, since one of the factors determining sour taste is the concentration of free hydrogen ions.
The tip is most sensitive to sweet, the root to bitter, the edge to sour, and the tip and edge of the tongue to salty. The areas sensitive to each of these stimuli overlap each other, and any taste sensation can be evoked from different areas of the tongue. In this case, however, it is necessary to vary the concentrations of solutions. Thus, the sensation of sweetness from the root of the tongue occurs at higher concentrations than from its tip
Salty
taste in its pure form is inherent in only one substance - table salt, sodium chloride.
Other salts, which have a salty taste, provide additional sensations of sweet, bitter and sour .
It is believed that the salty taste is determined mainly by the sodium cation, while at a molecular weight of salts below 110 the salty taste predominates, and above 160 the bitter taste predominates.
Sweet taste
inherent in many organic compounds (sugars, alcohols, aldehydes, ketones, amides, ethers, amino acids, etc.), as well as beryllium and lead salts.
Bitter taste
have substances of very different structures, containing the following groups: (NO2)>2, N=, SH-, -S-,- SS-, CS-.
Many substances have a mixed taste, for example bitter and sweet (saccharin, etc.), sour and sweet (citric acid). Natural stimuli, as a rule, cause very complex taste sensations, which depend not only on the irritation of specialized taste buds, but also on the stimulation of olfactory, pain, tactile and thermoreceptors of the oral cavity, proprioceptors of the tongue and masticatory muscles. An astringent taste occurs when tactile receptors are irritated as a result of stimulation of the mucous membrane by acids or salts of heavy metals. The burning taste is a consequence of stimulation of the pain receptors of the tongue.
Main characteristics of the taste analyzer
.
One of the most important characteristics of the sensory system is the absolute threshold
of sensitivity, i.e. the minimum concentration of a chemical that produces a taste sensation in a person. It is different for different substances. Thus, for sugar the minimum threshold is 0.01 M, for table salt - 0.05 M, for hydrochloric acid - 0.0007 M, for quinine hydrochloride - 0.0000001 M solution.
Threshold values of taste sensitivity vary from person to person. Moreover, it is possible to selectively increase the absolute threshold for individual substances, up to complete “taste blindness.” Differences in taste thresholds are typical not only for different people, but also for the same person in different states (illness, pregnancy, fatigue, etc.).
of differential thresholds has a certain value
, when the magnitude of the minimal perceptible difference in the perception of the same taste stimulus is determined when moving from one concentration to another. It has been shown that the differential threshold decreases when moving from weak to stronger concentrations, and within the limits of average concentrations an increase in discriminative sensitivity is observed. It decreases again when moving to strong concentrations. Thus, a 20% sugar solution is as sweet as possible, a 10% solution of table salt is as salty as possible, a 0.2% solution of hydrochloric acid is as sour as possible, and a 0.1% solution of quinine hydrochloride is as bitter as possible.
Hidden periods of taste sensations
– this is the time between the application of the stimulus and the appearance of the sensation of taste. They depend on the concentration of the solution. At concentrations approaching the threshold, the latent periods of sensation increase, and with increasing concentration they decrease.
Temperature
. For most chemicals, no simple relationship has been found between the temperature of the test solution and the change in absolute threshold, but it does exist. For example, for sugar, sensitivity increases with increasing temperature, but at 50°C it completely disappears. At 0°C there is a sharp decrease in sensitivity to all flavoring substances.
Adaptation
.
Contact of chemicals with the taste bud for some time leads to an increase in the absolute threshold and a decrease in the intensity of the taste sensation. The adaptation time is proportional to the concentration of the solution. Adaptation to sweet and salty substances occurs faster than to bitter and sour ones. When studying cross-adaptation
, i.e. the influence of adaptation to one substance on changes in thresholds to others showed that it does not exist for all substances.
So, if any acid reduces sensitivity to all acids, then for substances with a sweet taste, this pattern is not observed in all cases.
Adaptation to one substance can not only reduce, but also increase sensitivity to other substances, which is referred to as the phenomenon of taste contrast
. Adaptation to sugar or table salt increases sensitivity to compounds with other taste qualities. Adaptation to bitter (quinine) increases sensitivity to sour and salty, but not sweet.
The taste of mixtures is determined by the chemical specificity of their constituent substances. Thus, the sweet taste of fructose is reduced in combination with lactic and acetic acids, but not citric and hydrochloric acids. The sweet taste of sucrose is reduced by citric and lactic acids, but not by acetic and hydrochloric acids.
Theories of taste perception
.
Discovering the mechanisms underlying taste perception is very important for creating a theory of taste. the hypothesis of P.P.
deserves mention. Lazareva . He believed that under the influence of adequate taste irritations, the hypothetical highly sensitive substances of a protein nature contained in the taste buds disintegrate, which leads to specialized irritation of the nerve endings by ionized decomposition products. Each bulb is capable of reacting to all flavoring substances, but to a much lesser extent than to a substance of one flavoring quality
The enzymatic theory of taste by Baradi and Bourne explains the emergence of a specific taste sensation by the activation of certain enzymes in the cells of the taste bud. However, this theory was later criticized.
Of great importance for understanding the mechanisms of taste were hypotheses linking taste reception with membrane processes. According to this hypothesis, the initial stage of taste reception is the adsorption of a molecule of a substance on specialized sections of the protein chain associated with the receptor membrane. The idea that there are specialized active centers on the apical surface of the taste cell membrane that selectively adsorb substances with different taste qualities has been proven by Beidler’s electrophysiological studies. In addition, protein fractions were isolated from homogenates of the tongue epithelium, forming complex compounds, some with various sugars, others with bitter substances.
At the same time, Beidler's theory cannot explain some phenomena associated with taste perception, in particular, the phenomenon of adaptation. It reflects only the phenomena occurring in the receptor at the first stage of the action of the taste stimulus. Subsequently, neural integration mechanisms common to many sensory systems are activated.
Taste sensitivity
. Taste sensitivity varies among people, and in the same person it can change dramatically under the influence of many factors. Thus, it has been shown that the taste for sweets is better developed in women than in men. There is a dulling of taste sensations in smokers.
In our life, taste is of no small importance. Together with the sense of smell, it helps a person determine the quality of food. The oral cavity communicates directly with the nasal cavity, and therefore flavoring substances can easily affect the olfactory system. The taste and olfactory sensations are so closely related that they form an inextricable functional complex, due to which many patients with impaired sense of smell complain more about loss of taste than lack of perception of smells. For the same reason, various aromatic food substances and liquids affect the body not only with their taste, but also with their olfactory irritations. For example, the secret of the effectiveness of Truskavketskaya naftusya lies not only in the concentration of cations and anions, but also in its strong aroma and taste.
Taste sensitivity is closely interrelated with the level of general sensitivity, in particular temperature sensitivity, the connection of which with the taste apparatus is widely known in everyday life. The taste of many food substances is strictly dependent on their temperature. The most favorable food for consumption is considered to be food whose temperature is +24 ° C. To quench thirst, it is better to drink cold water with a temperature below the temperature of the oral cavity.
The question of the correspondence between taste and the body's food needs has been studied by many researchers. It has been proven that the pungency of taste decreases immediately after saturation, and after 1-1.5 hours it is restored to its previous level. In each person, as the feeling of hunger develops, sensitivity to sweets increases noticeably, and to sour and bitter things decreases somewhat. It is generally accepted that taste sensitivity decreases in the dark, in conditions of oxygen deficiency, at low and high food temperatures, at low and high ambient temperatures.
A common symptom of stomach diseases (and not only the stomach) is a coated tongue and loss of appetite (anorexia). I.P. Pavlov called this a protective “self-healing” reflex, since the patient’s refusal to eat creates the necessary rest conditions for the affected stomach. It follows that any plaque on the tongue and the accompanying anorexia is a measure of adaptation and preventive therapy. A measure that must not only be understood, but also supported in every possible way (P. N. Snyakin). Clinical experience shows that force feeding of patients with blocked taste perception and, therefore, with reduced or absent appetite, can bring nothing but complications.
Taste sensations can arise not only under the influence of adequate chemical stimuli, but also as a result of inadequate influences: mechanical, thermal and electrical. Thus, when the tip of the tongue is strongly pressed, an alkaline taste appears. When tapping on the side of the tongue, some people experience a sensation of salty taste, and when pressing with a dry finger on the base of the tongue, a sensation of bitterness occurs. Contact of the tongue with the electrodes of an electric battery causes a sour taste sensation.
The impact on taste buds causes changes in the state of many body systems: performance, metabolism, sexual activity, and vascular tone change. Thus, sour and bitter solutions reduce blood flow to the extremities, increase blood flow to the brain, reduce skin temperature, cause increased heart rate and increased blood pressure. Sweet substances cause an increase in blood flow to the extremities, a decrease in blood flow to the brain and an increase in skin temperature, i.e. act opposite to sour and bitter irritants. An intense salty stimulus most often causes dilation of cerebral and peripheral vessels. This means that all people with severe cerebral pathology should exclude spicy foods from their diet.
According to O.A. Naumova, chewing aromatic chewing gum, affecting taste buds, has a tonic effect on the body.
A change in taste is noted quite often: with infectious and gastrointestinal diseases, with diseases of the oral cavity and nasal cavity, with organic brain lesions, with drug addiction and long-term use of various medications. Psychiatrists know that in the early stages of schizophrenia, many patients complain of unpleasant taste or tastelessness of food. The pathology of the taste analyzer in such patients is apparently associated with partial or complete refusal of food, as well as delusional ideas of poisoning and certain variants of hypochondriacal delusions.
The phenomenon of decreased and perverted taste occurs in 0.5% of all patients. Patients with decreased taste sensitivity usually also suffer from decreased sense of smell and appetite. They, as a rule, lose weight and undergo treatment for a long time, but not always successfully. For some of them, eating often turns into a painful ordeal due to the fact that food products acquire a foul, sometimes foul smell and taste. It has been shown that such conditions may be associated with a decrease in copper and zinc in the body, and in these cases, pills containing zinc sulfate help well.
Salivary glands
Salivary glands
(lat. gladulae salivales) - exocrine glands that secrete secretions into the oral cavity, called saliva. There are minor and major salivary glands.
Minor salivary glands
The minor salivary glands are located in the oral mucosa and are classified by their location (labial, buccal, molar, lingual and palatal) or by the nature of the secretion (serous, mucous and mixed).
The most numerous of the minor salivary glands are the labial and palatine glands. Serous glands are found mainly among lingual glands; the saliva they secrete is rich in protein. The mucous glands are the palatine and part of the lingual; the saliva they produce is rich in mucus. Mixed - buccal, molar, labial and part of the lingual secrete saliva of mixed composition. The minor salivary glands are located deep in the oral mucosa or in its submucosa. The sizes of small glands are varied, their diameter ranges from 1 to 5 mm.
Major salivary glands
The major salivary glands are three pairs of salivary glands distinguished by their size.
The largest of them are the parotid salivary glands, located below and in front of the auricle directly under the skin.
The excretory duct of the parotid gland (stenon duct) opens on the side wall of the vestibule of the oral cavity at the level of the second upper molar. Medium-sized - submandibular salivary glands. An excretory duct departs from the gland - Wharton's duct, which is located at the bottom of the oral cavity and opens with a small hole at the top of the paired papilla, located near the frenulum of the tongue. The submandibular glands, like the parotid glands, secrete a mixed type of saliva.
The smallest of the major salivary glands are the sublingual glands, located under the mucous membrane of the floor of the mouth, on both sides of the tongue. They produce saliva with a predominance of the mucous component. From each of the sublingual glands, a Bartholin duct emerges, opening either separately on the sublingual papilla, or through one common opening with the Wharton duct. In addition, a number of small ducts depart from the sublingual glands, most of which open on the sublingual fold.
Figure used under CCA3.0 license, taken from “Medical gallery of Blausen Medical 2014”. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. Adapted.
Salivary glands in children and adults
The secretion of saliva begins in children immediately after birth. A newborn secretes 0.6–6 ml of saliva per hour, with active sucking - up to 24 ml per hour. Starting from the age of 3 – 6 months, the child’s salivation increases significantly. The weight of the salivary glands also increases (Paikov V.L.):
| Age | Average weight of major salivary glands, g | ||
| parotid | submandibular | sublingual | |
| newborns | 0,9–2,4 | 0,84 | 0,42 |
| 3 months | 1,4–4,8 | 1,54 | 0,84 |
| 6 months | 4,5 (3,1–5,8) | 2,12 | 1,05 |
| 2 years | 8,6 (8,2–9,6) | 4,89 | 2,00 |
| men | 36,6 (26–96) | 13,23 | 5,05 |
| women | 28,8 (22–48) | 9,70 | 4,68 |
Salivary glands in newborns
Features of the salivary glands of a newborn:
- low secretory activity
- secretion of a small amount of thick, viscous saliva (sealing the oral cavity during sucking)
- saliva reaction is neutral or slightly acidic
- amylase concentration is low.
The functional activity of the salivary glands increases at 1.5–2 months; In children aged 3–4 months, saliva often leaks from the mouth. This is due to the immaturity of the regulation of salivation and swallowing of saliva (physiological salivation). The acidity of saliva increases with age. From the first days of life, saliva contains a-amylase and other enzymes necessary for the breakdown of starch and glycogen. In newborns, during the first year of life the content and activity of these enzymes increase significantly (Geppe N.A., Podchernyaeva N.S., 2008).
Diseases of the salivary glands in ICD-10
In the International Classification of Diseases ICD-10, diseases of the salivary glands are classified as “Class XI. Diseases of the digestive system." A separate section “K11 Diseases of the salivary glands” includes the following diseases:
- K11.0 Salivary gland atrophy
- K11.1 Salivary gland hypertrophy
- K11.2 Sialadenitis
- K11.3 Salivary gland abscess
- K11.4 Salivary gland fistula
- K11.5 Sialolithiasis
- K11.6 Salivary gland mucocele
- K11.7 Disorders of salivary gland secretion
- K11.8 Benign lymphoepithelial lesion of the salivary gland
- K11.8 Mikulicz disease
- K11.8 Necrotizing sialometaplasia
- K11.8 Sialectasia stenosis of the salivary duct
- K11.8 Constriction of the salivary duct
Congenital anomalies of the salivary glands and ducts (salivary gland(s) or duct: absence, accessory, atresia; congenital fistula of the salivary gland) belong to “Class XVII. Congenital anomalies [malformations], deformations and chromosomal disorders”, to the heading “Q38.4 Congenital anomalies of the salivary glands and ducts”.
Frame “Methods of functional diagnostics of salivary gland secretion” from a video for medical university students: Khamchiev K.M. (Dr. Kureysh). Video lesson on physiology: Research methods and regulation of digestion. Food center
On the GastroScan.ru website in the “Literature” section there is a subsection “Oral diseases associated with gastrointestinal diseases”, containing publications for healthcare professionals on this topic.
Patient Materials
The GastroScan.ru website also contains materials for patients on various aspects of gastroenterology:
- “Advice from doctors” in the “Patients” section of the site
- “Popular gastroenterology” in the “Literature” section
- “Popular gastroenterology” in the “Video” section
Back to section
Drooling (sialorrhea, hypersalivation, ptyalism) is characterized by an increase in the amount of saliva with its flow from the oral cavity through the border of the lips in such a volume that it negatively affects the social and everyday activities of the patient, leading to damage to the soft tissues of the oral cavity, lips and chin.
Functions of the salivary glands under physiological conditions
Depending on the size, small and large salivary glands are distinguished. The minor salivary glands are localized in the mucous membrane of the lips, cheeks, tongue, hard and soft palate. The large salivary glands are located outside the mouth. Three pairs of major salivary glands (parotid, submandibular, sublingual) produce and secrete most of the saliva [1].
An adult produces about 1 liter of saliva per day [2, 3].
Saliva performs a number of important physiological functions that can be divided: digestive, protective, and excretory [4].
Digestion and swallowing:
provides the initial processes of digestion; moistens the oral cavity, teeth, tongue, food bolus; carries out food tasting; provides amylase breakdown of starch.
Disinfectant and protective role:
is an effective cleanser; maintains homeostasis in the oral cavity; prevents damage and destruction of teeth, the appearance of an unpleasant odor; has bacteriostatic and bactericidal effects; regulates the pH of the oral cavity.
Speech:
moistens the tongue and oral cavity.
Excretory function:
releases urea, uric acid, some medicinal substances, salts of lead, mercury, etc.
Conditioned reflex and unconditioned reflex regulation of the salivary glands ensures their uninterrupted functioning in healthy people. The secretion of saliva is a continuous process. Salivation occurs reflexively when food enters the oral cavity. The secretory activity of the salivary glands is regulated by the salivary zone of the cerebral cortex and the nuclei of the brainstem. The cortical zone is excited by signals coming from taste buds. Next, it interacts with the upper (nucleus of the facial nerve) and lower (nucleus of the glossopharyngeal nerve) salivary center of the brain stem.
The secretory activity of the salivary glands is provided by sympathetic and parasympathetic innervation. However, when eating and swallowing, the activity of parasympathetic innervation is mainly activated. Parasympathetic afferent pathways, receiving a signal from the receptors of the pharynx and esophagus, through the system of the vagus nerve and visceral nerves, reach the stem centers of salivation [3].
Parasympathetic efferentation occurs through two pathways. The glossopharyngeal nerve innervates the auricular ganglia, and subsequently the parotid gland via the auriculotemporal nerve. The facial nerve innervates the submandibular ganglia through the chorda tympani and then through the lingual nerve ensures the functioning of the submandibular and sublingual glands [5] .
The process of salivation is inextricably linked with swallowing. Swallowing is a reflex muscular act in which, as a result of alternate contraction and relaxation of muscles, a bolus of food is transferred through the pharynx and esophagus into the stomach. During the day, an adult makes up to 1200 swallowing movements, of which about 350 are not related to the intake of food and water. The act of swallowing consists of 3 phases: oral, pharyngeal and esophageal. The oral phase is voluntary, while the pharyngeal and esophageal phases are involuntary. The act of swallowing begins with the involvement of more than 30 different muscles of the oropharynx to form and move the bolus of food into the esophagus. Subsequently, the upper esophageal sphincter opens and the food bolus passes from the pharynx into the esophagus, and then into the stomach [6].
The swallowing mechanism is realized through a neural circuit that forms a reflex arc, including sensory fibers of the IX and X pairs of cranial nerves, the sensitive nucleus of the solitary tract (n. tractus solitarius), the motor double nucleus (n. ambiguus), motor fibers of the IX and X pairs of cranial nerves . Voluntary regulation of the act of swallowing is ensured by the bilateral supranuclear influence of the cortical swallowing centers, which are localized in the precentral gyrus, premotor cortex, fronto-parietal part of the tegmentum and in the anterior part of the insula. The most important center, which initiates the entire swallowing process, is considered to be a part of the cortex located somewhat anterior to the zone of cortical innervation of the hand in the motor cortex [7]. The brain stem centers of swallowing are localized in the dorsolateral part of the medulla oblongata and are represented by the already mentioned nuclei (n. tractus solitarius and n. ambiguus), as well as the reticular formation of the brain stem, which performs an integrative function, connecting the swallowing centers into a single system [8].
Sialorrhea in neurological diseases and its consequences
Sialorrhea can be caused by hyperproduction of saliva (true hypersalivation), or insufficient salivation (false hypersalivation). In turn, there are anterior and posterior variants of salivation. Unlike anterior sialorrhea (where saliva pours out of the mouth), posterior sialorrhea (i.e. saliva flows down the tongue into the throat) may increase the risk of unnoticed aspiration in patients who lie supine for long periods of time [9, 10].
In neurological practice, sialorrhea occurs in a number of diseases: Parkinson's disease, stroke, cerebral palsy, motor neuron disease (amyotrophic lateral sclerosis), multiple sclerosis [11-15].
Patients suffering from excessive salivation experience difficulty articulating speech and swallowing, and have bad breath. Constant leakage of saliva from the oral cavity forces one to resort to the use of handkerchiefs or towels, leading to perioral cracking, irritation, and maceration of the skin. Wetting and soiling of clothes and bed linen increases the burden on caregivers. Psychologically, excessive drooling can lead to decreased self-esteem and social isolation [4]. The following is information about the consequences of untreated sialorenia: physical - perioral cracking of the skin; maceration with secondary infection; dehydration; unpleasant odor; aspiration/pneumonia; speech problems; interference with feeding and psychological - isolation; obstacle to learning (saliva drips on books or electronic gadgets); dependency and degree/intensity of bystander care increases; electronic devices are damaged; social interactions are limited; self-esteem decreases.
Pulmonary aspiration is the most serious complication of sialorrhea. In particular, in patients after a stroke, aspiration may occur as a result of impaired swallowing function or due to gastroesophageal reflux [16, 17]. Insufficient protection of the respiratory tract from saliva accumulating in the oral cavity due to dysphagia can lead to its inhalation. The patient develops unexplained lung disease or recurrent pneumonia, which is a significant problem in the rehabilitation department, especially if the patient is lying down for a long time. In such patients, the risk of developing chronic salivary aspiration and pulmonary complications increases significantly [10]. In addition, unlike aspiration during swallowing, aspiration of continuously secreted saliva is difficult to control. In this case, changing the consistency of foods or stopping oral feeding is ineffective.
Sialorrhea during stroke
In patients after a stroke, sialorrhea most often occurs as a result of a violation of the process of swallowing saliva, mainly due to dysphagia. Neurogenic dysphagia during the acute period of stroke, according to various authors [7, 18], occurs in 25–65% of patients admitted for hospital treatment. Mortality among patients with post-stroke dysphagia and tube feeding varies from 20 to 24%, although this rate depends more on the severity of brain damage. In accordance with the recommendations of the European Stroke Initiative (EUSI, 2003), testing swallowing function in all patients who have suffered a stroke is mandatory in the patient management protocol, and correction of dysphagia is an integral part of basic treatment.
The cause of dysphagia and hypersalivation is often a combined lesion of the nuclei of the bulbar group of the medulla oblongata. At the same time, during eating, food is not directed by the tongue to the pharynx. The larynx does not rise upward, and the root of the tongue does not press down on the epiglottis and does not cover the entrance to the larynx, making it difficult for a food bolus to reach the pharynx. The soft palate recedes and oral fluids and food enter the nose.
A stroke in the medulla oblongata occurs due to thrombosis of the anterior spinal artery or its branches, branches of the artery supplying the medulla oblongata, and in the basin of the inferior posterior cerebellar or vertebral artery. Thus, it is necessary to pay special attention to patients with a stroke in the medulla oblongata with the formation of alternating Jackson, Avellis, Schmidt, Wallenberg-Zakharchenko syndromes. Sialorrhea is aggravated by lesions of the accessory nerve nucleus (Schmidt's syndrome), as the resulting weakness of the sternocleidomastoid muscle causes head tilt and saliva leakage from the mouth.
Drooling after a stroke can occur due to central and peripheral damage to the facial nerve. With paresis of the muscles of the lower part of the face and lips that are not tightly closed, saliva may leak from the oral cavity. Central paresis of facial muscles occurs with pathology in the lower part of the precentral gyrus or with damage to the corticonuclear pathway.
Thus, the cause of sialorrhea during a stroke may be difficulties in the efficiency and frequency of swallowing, decreased sensitivity or weakness of the muscles of the face and oral cavity, and impaired head posture.
Methods for assessing salivation
There are many diagnostic methods for assessing the functional activity of the salivary glands. Both sialometry methods and scoring of the frequency and severity of salivation are used. The most common are: 1) visual analogue scale from 1 to 10 (where 1 is the best and 10 the worst possible options); 2) counting the number of standard sizes of paper handkerchiefs used during the day; 3) measuring the volume of saliva collected in a container tied to the chin; 4) weighing the gauze pad dry and for a certain period of time after placing it in the oral cavity; 5) salivary gland scintigraphy; 6) cannulation of salivary ducts and assessment of saliva production, etc. [4]. Most researchers use the Drooling Frequency and Severity Scale (DFS) [19] (see table).
Scale of severity and frequency of drooling
Treatment methods for sialorrhea
Treatment of sialorrhea includes methods aimed at reducing saliva production with the administration of acetylcholine transport blockers, cholinesterase inhibitors, clozapine and quetiapine. However, the effectiveness of these methods is only partial and new pharmacological and non-pharmacological approaches to the treatment of sialorrhea are needed [4].
Various groups of drugs are being studied, including anticholinergic drugs, adrenergic receptor antagonists, and botulinum toxins (BT).
There are no current recommendations for the use of non-pharmacological methods in the treatment of sialorrhea in stroke. However, behavior modification and, in refractory cases, radiotherapy can be considered as additional components of the overall treatment package.
The main mechanism of action of BT is inhibition of acetylcholine release. Local injections into the salivary glands inhibit cholinergic parasympathetic and postganglionic sympathetic activity, causing a decrease in salivary secretion.
BT injections for excessive drooling were first proposed in 1997 [20]. To date, botulinum therapy has established itself as a safe and effective method of treating sialorrhea [21]. In clinical practice, both serotypes of BT, A and B, are successfully used for a number of neurological diseases: cerebral palsy, Parkinson’s disease, stroke, motor neuron disease, mental retardation, dementia and other diseases and conditions [3, 22, 24, 25]. According to numerous studies, the effectiveness of both aboBT and rimaBT injections compared with the initial level is observed in 89% of patients. There was no dependence of the effectiveness of therapy on gender, number of injections or serotype used. The overall average duration of treatment effect is 87 days and is the same for both serotypes. Repeated injections do not affect the duration of the effect [15, 26-30].
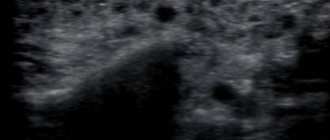
In most studies, BT is injected into the parotid and submandibular glands, less often only one of these glands is injected. In a few descriptions, the administration of BT into the parotid gland was combined with an injection into the sublingual gland (the drug was administered through a catheter into the salivary duct) [31]. More than half of the published studies favored ultrasound-guided injections over anatomical landmarks. The onset of treatment effect in most studies ranged from 1 to 14/15 days. The duration of action ranges from 2 to 36 weeks [32, 33]. The outcome of therapy was assessed using a combination of objective and subjective methods. Studies have confirmed the effectiveness of botulinum therapy, the percentage of respondents varied from 40 to 100%.
Adverse events were classified as transient and mild. The most common complaints were a feeling of sticky saliva followed by dry mouth. Some authors pointed out more severe side effects: dysphagia [15, 31, 34-41], jaw dislocation [15], difficulty chewing [34, 38]; suffocation [36], aspiration pneumonia [36, 41, 42], transient paresis of the facial nerve [13], temporary awkwardness when wearing dentures [43], weakness in the neck muscles [41].
Some of the studies concern the direct use of BT for sialorrhea due to stroke [28, 29, 44-46]. In particular, in one of them, BT-B injections were performed into both submandibular glands under ultrasound guidance [29]. The severity of drooling was assessed using the Drooling quotient (DQ) and the Drooling Impact Scale (DIS) for 16 weeks after injection. All 16 patients included in the study noted clear improvement within 2 weeks after injection. Saliva production rate and DQ decreased within 1 week after injection and persisted for 12 weeks. There was no statistical difference in the duration of the effect between groups of patients receiving different doses of B.T. No adverse events were noted.
A. Lipp et al. their study compared different doses of aboBT (abobotulinumtoxin, Dysport). Patients with sialorrhea after stroke were administered aboBT in doses of 18.75, 37.5, and 75 units. There was a significant improvement compared to placebo only for the 75 U dose [26].
Another prospective, double-blind, randomized controlled trial was conducted over 24 weeks [47]. Among the subjects were 17 patients who had suffered a stroke. Patients with significant drooling were randomly assigned to receive different doses of botulinum toxin type A (Dysport) and placebo injections into the bilateral submandibular and parotid glands. The injections were carried out under ultrasound guidance. BT-A was administered in dosages of 50, 100, or 200 units. The results were assessed by the reduction in saliva amount measured by weighing dry and saliva-moistened gauze before the start of therapy, 2, 6, 12 and 24 weeks after injection. The frequency and severity of drooling were assessed using the DFS scale. A decrease in salivation was observed in response to any dose of BT-A. However, a dose-dependent effect was determined by the duration of the effect. In the group of patients receiving 200 U, aboBT showed a decrease in sialorrhea lasting up to 24 weeks.
The fact of saliva aspiration by a patient with severe consequences of a stroke before treatment with BT-A and its significant reduction was confirmed in a study using a radionuclide salviogram. The authors propose this control method as reliable evidence of saliva entering the respiratory tract and the effectiveness of BT for the prevention and treatment of saliva aspiration in patients with stroke [30].
Drooling after a stroke is a serious complication that requires close attention from medical personnel and caregivers. In association with dysphagia, sialorrhea leads to “silent” aspiration of saliva with the threat of pulmonary complications and death of the patient. Reducing salivary production by injecting BT into the major salivary glands is a proven and most effective method of rehabilitation for patients with sialorrhea who have suffered a stroke.