Target point of infraorbital anesthesia : the infraorbital foramen, which includes the peripheral branches of the infraorbital nerve. The location of the target point can be determined in 3 ways: 1. The infraorbital foramen is located 5-7 mm below the intersection of the lower edge of the orbit with the vertical line that passes through the pupil of the eye looking forward (see Fig. 70, A).
Rice. 70. Location of the infraorbital foramen (explanation in the text).
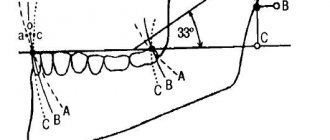
2. In the middle of the lower edge of the orbit, a bony protrusion or groove is palpated - the junction of the zygomatic process of the upper jaw with the zygomatic bone - 5-7 mm below this protrusion is the infraorbital foramen (see Fig. 70, B). 3. The infraorbital foramen is located 5-7 mm below the intersection of the lower edge of the orbit with a vertical line drawn through the middle of the second upper premolar (see Fig. 70, B). It must be remembered that the axis of the infraorbital canal is directed forward, in the middle, down and crosses the axis of the canal of the opposite side above the gingival papilla between the upper central incisors (Fig. 71, 72).
Rice. 71. Direction of the lower orbital canals and the place of their intersection between the upper central incisors
Rice. 72. Insertion of a needle into the canal during intracanal infraorbital anesthesia (V.I. Zausaev et al., 1981)
Modification of intraoral infraorbital anesthesia:
advancing the needle between the canine and the first premolar. In a similar way, you can advance the needle at the level of the canine, first and second premolars (Fig. 74).
Rice. 74. Modifications of intraoral infraorbital anesthesia. Injection site: 1 - between the central and lateral incisors; 2— above the fang; 3— above the first premolar
It was noted that the more distal the injection site, the weaker the analgesic effect due to the fact that the axis of the infraorbital canal does not coincide with the direction of the injection. Therefore, the best anesthesia will be in position 1 (injection point between the central and lateral incisors), the worst position is 3 (injection point above the first or second premolar). When passing the needle at the level of the canine, first and second premolars, it is impossible to enter the infraorbital canal; pain relief occurs due to the diffusion of the anesthetic in the area of the infraorbital foramen. It should be noted that with these modifications there are practically no complications due to injury to blood vessels and nerve endings when the needle is advanced. Therefore, in recent years, the following anesthesia has gained significant popularity.
Execution method
Infraorbital anesthesia provides the possibility of using one of two methods, the choice between which is determined by the specific anatomical structure of the maxillary region, as well as the goals that need to be achieved as a result of the procedure. The drug is administered both externally and internally, but in both cases the doctor requires concentration and attention.
The intraoral method involves determining the position of the desired hole, after which in the projection area the soft tissues are pressed against the bone base, and at the same time the lip is retracted upward. The needle insertion site should be located 5 mm above the fold that marks the transition between the premolar and the canine. After establishing contact, the doctor injects about 1 ml of the drug into the canal, after which he probes the position of the mouth with the end of the needle. The free position means hitting the desired area - the tip is immersed to a depth of up to 10 mm, where another part of the anesthetic is released. The result appears within 4-5 minutes from the moment the drug is administered.
In situations where it is not possible to place a needle in the area between the incisor and the canine, the injection is made at the level of the canine, the first or second small molar. However, in this case, entry into the canal is excluded, and the analgesic effect is the result of diffusion of the composition. It is also worth noting that the intraoral method of anesthesia is characterized by a number of disadvantages, including the technical complexity of implementation, as well as restrictions on the procedure for diagnosed frontal periostitis.
The extraoral method is implemented through the external tissue, in the area located next to the nose. The projection of the position of the infraorbital foramen is built mentally, after which the doctor presses on the tissue with the index finger and retreats about 5 mm downwards, towards the center. The needle is inserted in three directions - until it comes into contact with the periosteum tissue into which the drug is injected. Next, the procedure similar to the first method is repeated.
The use of active anesthetics makes it possible to administer the composition only in the area under the orbit. At the same time, the effectiveness of anesthesia at the site of innervation of the alveolar branches virtually remains unchanged.
Technique for intraoral infraorbital anesthesia between the canine and the first premolar:
1. Using the index finger of the left hand, fix the projection of the infraorbital foramen to the bone; with the thumb, pull the upper lip up to the index finger (Fig. 75, B). 1. The needle is inserted 5-7 mm above the transitional fold between the canine and the first premolar, moved back, up and in the middle so that it approaches the infraorbital foramen (Fig. 75, B).
Rice. 75. Stages of performing intraoral infraorbital anesthesia for an injection between the canine and the first premolar : A - the path of advancement of the needle during intraoral infraorbital anesthesia between the canine and the first premolar, the zone of dental anesthesia for infraorbital anesthesia is indicated (diagram); B: Stage I - soft tissues are fixed with the index finger and thumb; B: Stage II - the needle is inserted 5-7 mm above the transitional fold between the canine and the first premolar, advanced to the mouth of the infraorbital foramen
The following steps are similar to the above intraoral infraorbital anesthesia method. With this anesthesia, the solution is injected into the mouth of the infraorbital foramen, which prevents injury to the neurovascular bundle. It should be noted that when using a strong anesthetic, there is no need to administer an anesthetic solution intracanal.
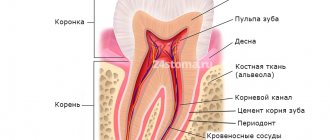
Mandibular canal
The presence of accessory canals in the maxilla has been reported in the literature, calling into question the nature of anatomical variation in their presentation. Recognition of these formations is of great importance in the practice of implantology. The mandibular canal extends from the mandibular foramen on the medical surface of the ramus of the jaw to the mentonal foramen. The mandibular canal contains the mandibular vessels, artery and veins, as well as part of the mandibular branch of the trigeminal nerve. In the analyzed sample, the auxiliary mandibular canal has a low prevalence. It is believed that its presence is related to the independent projection of the incisal branches of the inferior alveolar nerve, the evaluation of which is necessary to avoid its involvement in mandibular implant procedures.
Anatomy of the mandibular canal
The presence of accessory canals in the mandible has been reported in the literature, and recognition of these formations is of great importance in the practice of implantology. The mandibular canal is a formation that begins on the medial aspect of the ramus of the mandible from the mandibular foramen and continues in the inferolateral direction, referring along the roots of the lower molars and premolars. When viewed transversely, the mandibular canal may have an oval, round or piriform shape, within which lies the inferior alveolar neurovascular bundle, consisting of blood vessels and the inferior alveolar nerve, a branch of the third division of the trigeminal nerve. Due to the location and course of the mandibular canal, anatomical analysis using imaging studies allows both its own assessment, the identification of pathological processes, and the assessment of the quantity, height and quality of the bone. These data are considered important for planning and performing surgical procedures for mandibular implantation. Typically, this canal is presented as a single canal, but the presence of a second or third mandibular accessory canal has been reported in the literature.
The presence and formation of the accessory mandibular canal is explained by the fact that during embryonic development, at approximately the 7th week of development, the inferior alveolar nerve consists of three separate nerve branches that are directed to innervate groups of mandibular teeth. These nerve branches fuse during prenatal growth of the mandible to form a single inferior alveolar nerve, which is surrounded by membranous bone tissue to form the mandibular canal. However, when incomplete fusion of any of these nerve branches occurs, tissue ossifies around it, giving rise to the accessory mandibular canal. The presence of an accessory mandibular canal may decisively influence the choice of site for implant treatment due to the risk of damage to the inferior alveolar neurovascular bundle and may also cause postoperative sensory disability. Therefore, knowledge about the existence, position and course of the auxiliary mandibular canal and the thickness of its cortical layer is necessary for correct diagnosis and assessment of the condition of the mandibular region. This will allow you to correctly select and position dental implants to prevent post-operative complications.
Read on topic: Therapeutic decision tree in periodontology
Mandibular canal of wisdom tooth
When we talk about paresthesia, we mean a change in sensation in a limb or other parts of the body, such as the lower jaw. This change is also called numbness of the lower lip, which forces the patient to focus on this problem with all the attendant concerns. The culprit of this problem is almost always a wisdom tooth or lower third molar, which, when inflamed, can come into contact with the inferior alveolar nerve, a nerve located in the mandibular canal. When this nerve is damaged during tooth extraction, it can cause paresthesia after wisdom tooth removal. If lower wisdom teeth are present, tooth extraction must be well planned due to the clinical problems associated with extraction. The lower third molar usually erupts at the age of twenty with a highly variable eruptive path depending mainly on lack of space, obstruction of normal eruption due to cysts and tumors, late mineralization and its inclination expressed as normal, mesial or horizontal inclusion.
These eruptive processes occur in an area where an important nerve structure called the mandibular nerve is located. The listed problems in some situations can lead to the proximity of the roots of the lower wisdom tooth to the mandibular canal and, consequently, to the lower alveolar nerve contained in it. The solution in these cases should not be extraction, as this may disrupt the integrity of the mandibular canal with possible paresthesia. Extractive orthodontics is an innovative technique that allows those teeth that are in contact with the inferior alveolar nerve to move the lower third molar away from the mandibular nerve and then safely extract it without damaging the mandibular nerve in any way. This is a combined technique in which the hook is recessed and lifted upward using orthodontic technique, moving the tooth away from the mandibular canal.
Extraoral classical method of infraorbital anesthesia
Injection equipment: carpule syringe or disposable plastic syringe 2 ml, needle 25 mm long. Anesthesia technique 1. Using the index finger of the left hand, fix the projection of the infraorbital foramen to the bone (Fig. 76).
Rice. 76. Extraoral classical method of infraorbital anesthesia (V.I. Zausaev et al., 1981)
2. Stepping back from the projection of the hole downwards and in the middle by 5 mm, the needle is inserted into the bone, directing it up, back and in the middle. 3. Ahead of the needle, 0.5-1 ml of anesthetic is released. When the needle touches the bone, carefully look for the entrance to the canal. Sometimes the needle immediately falls into the canal. With experience it is often possible to immediately enter the channel. 4. Having entered the infraorbital canal, advance the needle 3 mm and, after an aspiration test, release 0.5 ml of anesthetic. Pain relief occurs instantly. 5. Anesthesia zone - see intraoral method (Fig. 77).
Rice. 77. Zone of anesthesia during infraorbital anesthesia
This anesthesia is used, as a rule, to inject an anesthetic into the infraorbital canal - for high-quality and long-term pain relief during traumatic interventions (surgeries). In case of significant inflammatory processes (periostitis, osteomyelitis) of the upper jaw, when the inflammatory infiltrate spreads to the entire infraorbital region, we used a modification of extraoral infraorbital anesthesia for pain relief.
An effective technique for anesthesia of the lower jaw
Many novice dentists often face the problem of anesthesia of the lower jaw. She has a complex anatomy, and the difficulty in administering anesthesia is that we do not see obvious anatomical areas where we need to inject. With the upper jaw everything is much simpler. We simply numb the area of the tooth that we will treat. Unfortunately, this cannot be done on the lower jaw in all patients. She has a denser bone structure and this makes the passage of the anesthetic more difficult.
There are patients with thin bones for whom only infiltration anesthesia is sufficient. But most have to undergo torus or intraligamentary anesthesia. The latter method is less common, since it requires a special needle and special care when performing the injection.
Technique of mandibular anesthesia
We will tell you how to perform conduction anesthesia on the lower jaw in order to achieve 100% results and work comfortably with the tooth without causing discomfort to the patient.
To determine the injection site, you will have to remember the anatomy of the lower jaw. It has coronoid and condylar processes. Between them there is a notch and a hole where the branch of the nerve enters. This is where you need to get the needle to “turn off” that part of the nerve that enters the body of the lower jaw and innervates the teeth.
First, feel the edge of the coronoid process with your finger. This is not always easy to do if the patient, for example, has large masticatory muscles. To feel it better, ask the patient to cover his mouth a little. The muscles will relax and you will be able to separate the body of the muscle from the coronoid process.
When you find the process, move your finger a little and feel the buccal ridge. It can be easily felt. This is the landmark where the injection point is located.
Holding your finger on the inside, pulling out the corner of your mouth as much as possible with a carpule syringe, inject. At the same time, the patient needs to keep his mouth wide open so that the muscles stretch, the needle passes through them easily and there is no false impression that you are hitting the bone.
Then slowly insert the needle until it makes contact with the bone. To understand whether you have hit a bone, you can lightly tap it, then a characteristic sound will appear.
After this, you need to release about a third of the anesthetic and change the position of the needle: moving it away and reintroducing it at different angles, and so on several times. This, as it were, “spills” the anesthetic over the entire surface between the coronoid and condylar processes.
Completion of the anesthesia procedure
There is no need to enter the carpula completely. Other nerve branches in the thickness of the bone tissue, which also innervate the teeth and do not fall within the zone of anesthesia, can provide the sensitivity that remains after conventional conduction anesthesia.
It is better to apply additional infiltration anesthesia in the tooth area, no more than 1/5 of the volume of the carpule.
With the correct technique of mandibular anesthesia, you can treat several teeth in a row, and your patients will be painless and comfortable.
Material and methods
The study included 2 stages: experimental and clinical. To experimentally substantiate the method, 15 certified HF preparations were used, taken from the archive of the scientific craniological collection of the fundamental museum of the Department of Human Anatomy of Volgograd State Medical University. Specimens without visible bone pathology were selected. The choice of the needle insertion site met the requirements that were placed on it [3]. Next, in the area between the medial and lateral incisors at the level of the projection of the apices of their roots, the cortical plate was trepanned with a bur, after which 2.0 ml of iodolipol was injected into the spongy substance of the jaw using a Record type syringe. To study the spreading of the contrast agent, radiography of the preparation was performed in a lateral projection using the traditional method.
The clinical study consisted of a comparative assessment of the effectiveness of infraorbital anesthesia performed by the traditional method and the method of intraosseous anesthesia. Based on the fact that the best indicator of the effectiveness of anesthesia is the quality of anesthesia of teeth during their depulpation [5], we treated premolars for exacerbation of chronic pulpitis in 100 patients of the 1st period of adulthood (21-35 years). There were 48 (48.0%) men, 52 (52.0%) women. The choice of a group of teeth was associated with the boundaries of the zones of anesthesia during infraorbital anesthesia.
All patients were divided into two groups. Group 1 consisted of 50 (50.0%) patients who were treated using infraorbital anesthesia. In patients of the 2nd group - 50 (50.0%) people - after obtaining informed consent, intraosseous anesthesia was used for this purpose according to the method we developed (RF Patent No. 2427393) [1]. To perform anesthesia, we used a device of our design (RF Patent for utility model No. 98894) [2].
The essence of the technique was as follows. After anesthetizing the site of future injection, the mucous membrane was punctured until the tip of the needle came into contact with the bone. With slight pressure on the drill tip under conditions of low-speed rotation, the injection needle was passed through the cortical plate into the cancellous bone, which was determined by its characteristic “sinking.”
After removing the mandrin from the needle cannula, a Record type syringe with collected anesthetic was fixed in it, which was injected into the spongy substance of the jaw. Next, the needle and syringe were easily removed from the bone. The anesthetic used was a 4% solution of articaine with epinephrine at a dilution of 1:100,000. The volume of anesthetic administered during infraorbital anesthesia was 1.0 ml, and during intraosseous anesthesia - 0.5 ml.
The boundaries of anesthesia zones, depth and duration of anesthesia were studied using neurological and electrophysiological methods. The electrical excitability of the dental pulp was determined by the L.R. method. Rubin (1976), using PULP VITALITY TESTER made in the USA. The criterion for pulpal analgesia was a value of 100 μA, recognized in domestic endodontics and physiotherapy as an indicator of the desensitization (death) of the pulp [7].
Pain sensitivity of the skin of the upper lip and mucous membrane of the alveolar process was studied using a standard method using a sharp probe. The effectiveness of pain relief was assessed as complete, partial and insufficient [5].
Side effects and complications
The cause of complications that arise during infraorbital anesthesia is non-compliance with the technique of administering the anesthetic, which determines the requirements for the qualifications of the doctor performing the procedure. Incorrect administration can lead to damage to the eyeball, bleeding or hematoma formation. In addition, possible problems include:
- Disruption of the natural blood circulation cycle in the area under the eye socket;
- Swelling of the tissues of the lower eyelid;
- The appearance of the effect of diplopia - splitting of visual perception;
- Post-traumatic neuritis, as well as blockade of the muscles of the eyeball.
It is also worth considering that when the lower wall of the canal located under the orbit is perforated, there is a possibility that the solution will enter the sinus of the maxillary region.
Strict adherence to the protocol at all stages of pain relief allows you to avoid negative consequences. You can prevent the formation of a hematoma in the area where the needle is inserted by pressing the area where the vascular bundle exits for 2-3 minutes.