Summary
Reconstruction and rehabilitation of patients with defects of the upper jaw are the most difficult in reconstructive maxillofacial surgery, occupying the minds of oncological surgeons working in this area, microsurgeons, plastic surgeons and orthopedic dentists involved in maxillofacial and somatotropic prosthetics.
The fundamental difference between patients who have undergone anatomical reconstruction of the alveolar process of the upper jaw, as well as nasal support with microsurgical grafts and patients who have undergone maxillofacial prosthetics with obturation structures is an increase in the volume of the respiratory space, improved speech, the absence of atresia, frequent acute respiratory viral infections and, fundamentally, in the absence of regular relocation of definitive orthopedic work [1]. An important difference is also the lack of mobility of dentures on dental implants, which avoids chronic trauma to surrounding tissues.
This article describes the experience of rehabilitation of patients with defects of the upper jaw using fibular and Chinese skin-bone flaps with further plastic surgery of bone and soft tissues in order to create conditions for dental implantation, orthopedic conditions and features of fixed prosthetics for this group of patients.
The developed protocols for the use of a particular graft on a vascular pedicle are described in terms of the type of defect and further restoration of bone joints, as well as measures for the formation of anatomically close to normal conditions for implantation and prosthetic dentistry in patients with a reconstructed upper jaw.
Contraindications for prosthetics
The method of prosthetics is always chosen by the attending physician, taking into account many factors, including the general condition of the patient and an assessment of his psychological comfort. Among the contraindications that may cause this procedure to be postponed for some time are the following:
- various blood clotting disorders in the postoperative period or those of a chronic or temporary nature;
- first and last trimester of pregnancy;
- menstruation in women;
- presence of chronic infectious diseases;
- the presence of acute inflammatory processes;
- decreased immunity of various origins, etc.
Even ARVI can make it impossible to carry out prosthetic procedures. Before visiting the dentist, it is recommended to measure your body temperature, and if there are indicators different from the physiological norm, you should inform your doctor. Prosthetics for loose teeth
is carried out only after consultation with a doctor, since it can be difficult due to the lack of supporting teeth necessary for installing a crown. You may be asked to remove loose teeth.
Introduction
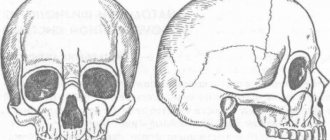
The upper jaw is the most complex area in reconstructive maxillofacial surgery, being more responsible for appearance than others, and due to the presence of such organs and anatomical formations as the eyes, zygomatico-orbital complex, and teeth.
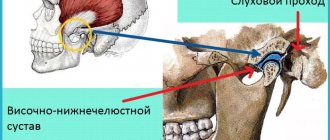
The upper jaw is a support for the lower jaw from the point of view of the stationary container of antagonists, also a zone of concentration of air cavities and a complex of buttresses. Defects and deformations in this area lead to disfigurement and limit or make impossible vital body functions such as chewing, swallowing, breathing, and vision. Restoration of buttresses is necessary from the point of view of optimizing the transfer of stress of the masticatory load, as well as to strengthen the reconstructed alveolar process of the upper jaw. [3]
Despite the positive results of tissue autotransplantation using microsurgical techniques, creating conditions for fixed and conditionally removable dental prosthetics remains a serious problem. The presence of a skin area with an array of subcutaneous fat makes the creation of an orthopedic bed and the attachment of soft tissues around the completed orthopedic structures almost impossible and reduces the functional significance of the work performed aimed at the rehabilitation of the chewing function. [2]
The article is devoted to the synergistic efforts of a maxillofacial surgeon and an orthopedic dentist to create functionally significant conditions and long-term results in patients with reconstructed upper jaws using skin-bone autografts on a vascular pedicle.
In the world literature available to us on the rehabilitation of chewing function in patients with jaw defects, we did not find any descriptions of the formation of a prosthetic bed, features of the choice of orthopedic structures, or long-term results after dental prosthetics.
Key words: jaw defect, lack of occlusion, obstructive prostheses, dental implantation, fixed prosthetics, integrated implants, micro-surgical autotransplantation, bone grafts, fibula, parietal bone, three-dimensional bone augmentation.
When is the best time to undergo prosthetics?
There are different types of dental prosthetics. Emergency prosthetics using removable structures can be performed within 24 hours after surgical removal of the crown and root of the tooth. More often, such procedures are relevant if several teeth have been removed at once or the front teeth have had to be removed, which creates a certain psychological discomfort for the patient. Most removable dentures, which are installed immediately after tooth extraction, are temporary and later require replacement with permanent dentures.
Installation of prostheses for permanent use is carried out on an individual basis, after specific preparation within the time frame established by the doctor after assessing all associated factors. In most cases, such prosthetics can be performed 1-2 weeks after surgery, if the patient has no contraindications. How much does front tooth replacement cost?
, both temporary and permanent, you can check with your attending physician, since this indicator is also individual in nature.
Material and methods
From 2008 to 2014 in the reconstruction of the upper jaw, we used a fibular autograft for the reconstruction of total defects (5 cases) and a radial autograft for the reconstruction of subtotal defects (10 cases). When using a radial skin-bone autograft in the subsequent placement of dental implants, there is a need to recreate the second cortical-spongy layer of the alveolar process on the lingual side, which can be achieved using parietal or mandibular free autoblocks.
With VRGN, relatively small defects of the alveolar process of the frontal part of the upper jaw are noted; more often the problem is the elimination of the defect of the palatal plate. Bone reconstruction requires the alveolar process, represented by genetically modified bone tissue in the projection of the bone cleft. A palatal bone defect does not require repair, since functional loss does not occur in the absence of reconstruction of the bone component. It should be noted that with complete clefts the main problem is communication with the nasal cavity. To eliminate defects of the upper jaw, we have developed a technique for using a free split chin graft and transplanting a fasciocutaneous graft [Application: 2010118686/14, 05/12/2010. Patent No. 2435537 ](4 cases).
In cases where the patient's health condition did not allow microsurgical transplantation, we installed Zygomatic system implants and fixed prosthetics (6 cases).
After a clinical assessment, instrumental diagnostic methods were used to study the pathology of the integrity of the jaw/s: OPTG, TRG, CT (with angiocontrast and soft modes).
If a tumor was present, the extent of resection was assessed and the optimal graft was selected according to the developed algorithm. If the X-ray picture of the tumor was detected, a biopsy was performed and, when the diagnosis was verified, resection of part or all of the jaw was performed. For jaw defects, after clinical and instrumental analyses, treatment planning began.
Preoperative planning was carried out using 3D visualization programs that made it possible to simulate the sizes, shapes, and position of the revascularized autografts relative to the bone structures, taking into account the positioning of the condylar processes of the mandible in the temporal fossae (anterior-superior position in the articular cavities) according to CT studies and the formation of anatomical buttresses for the upper jaw. A special feature of the programs is the absence of distortions in the individual dimensions of the patient’s skull.
We used fibular and radial autografts, since only they allow us to perform 3D modeling of the bone component congruent with the defect in the maxillary defect. Subsequently, when using a radial graft, the technique of transplanting free cortical-cancellous grafts was used to thicken the alveolar process for further dental implantation. Thus, a comprehensive and step-by-step reconstruction of the jaw defect was carried out to create conditions for restoring chewing function with fixed and conditionally removable orthopedic structures, which is important for any jaw defects.
After engraftment and activation of the dental implants, the subcutaneous fat pad of the fibular and radial flaps and the removal of excess skin pad were removed.
Orthopedic rehabilitation consisted of choosing the design of the prosthesis and precise adherence to the accuracy of taking impressions to transfer the complex relief of soft tissues and the position of the implants onto precise plaster models. The usual occlusion and central relationship of the jaws were recorded for the subsequent selection of prosthetic tactics for patients with reconstructed upper jaws. Plaster models were installed into the articulator using a facebow. The existing occlusion and centric relation were assessed. Depending on the type of defect, we selected the desired position of the lower jaw to create optimal chewing function and aesthetic results.
Particular attention was paid to the creation of a prosthetic bed for a future orthopedic design supported by dental implants. In these clinical situations, there is no attached keratinized mucous membrane around the implants in the oral cavity, which makes it difficult to accurately transfer the relief of the soft tissues of the prosthetic bed to create adapted non-removable orthopedic structures.
After the manufacture and fixation of temporary crowns on the implants, the presence of tumor-like growths of the mucous membrane around the installed orthopedic superstructures, which were histologically described as polyps, was noted. Patients complained of bleeding and discomfort around the installed crowns. Attempts to change the eruption profile of structures from implant shafts did not produce a positive result.
We used a method of simultaneous surgical correction of the subcutaneous fat area of autografts with the installation of provisional structures supported by dental implants. In a number of cases, we used a removable compression acrylic plate on the gum formers, which held the surgically created profile until permanent prosthetics or installation of provisional fixed and conditionally removable structures.
After 3 months, we made permanent orthopedic fixed or conditionally removable structures.
For the manufacture of orthopedic structures, we used cobalt-chrome alloy, titanium and zirconium dioxide.
As a rule, after the integration of implants and placement of gum formers at the prosthetic stage, we were faced with the need to modernize the prosthetic elements of the implantation system for specific clinical cases.
The gum formers were needed to be longer and predominantly conical in shape. The cylindrical shape of the gum former created parallel walls of the crater of the mucous membrane, which caused rapid collapse of the walls during the placement of the impression coping and caused severe discomfort to patients during manipulations. We attribute this to the presence of excess connective tissue layer, which is located on the autograft bone.
It is important to note that immediately after corrective operations on the skin-fat part of the flaps, orthopedic compression plates were fixed to prevent further growth of the soft tissue component.
Patients were monitored every seven days and appropriate compression plate adjustments were made.
Depending on the chosen permanent structure, a set of further orthopedic manipulations was carried out to make prostheses.
The results were recorded using a Canon D 60 camera, 100 mm lens, and MR-100 ring flash.
Description of clinical observations
Patient U. , 18 years old, was admitted to the clinic on April 1, 2008 with a diagnosis of osteoblastoma of the upper jaw, a condition after subtotal resection of the upper jaw on the left. From the anamnesis: a neoplasm was discovered and removed in early childhood at the Federal State Institution Central Research Institute of Infectious Diseases and Maxillofacial Surgery. The patient was sent to the clinic of the Russian Scientific Center for Surgery named after. acad. B.V. Petrovsky.
Status localis: the configuration of the face in front and profile is changed, the upper lip is retracted on the left. On palpation, a defect in the alveolar process of the upper jaw on the left is noted.
Mouth opening is not limited, there is a through defect in the alveolar process of the upper jaw with teeth 21-28, the patient wears an obturating denture, the denture teeth are in the bite.
Bite according to the second class according to Angyu.
On OPTG and CT: there is a defect of the zygomatic tubercle, alveolar process on the left, absence of the spine of the upper jaw, the base of the pyriform foramen on the left, defect of the tubercle of the upper jaw on the left. An impacted 28th tooth is noted in the remains of the pterygomaxillary articulation.
Treatment tactics: since the defect of the upper jaw was subtotal and through, a radial skin-bone graft on a vascular pedicle was used. When transplanting a radial cortico-periosteal-skin graft, a zygomatic-maxillary buttress was formed using a free split graft from the branch of the mandible on the right. The second stage involved the formation of the alveolar process using parietal grafts.
Rice. 1. Appearance of the patient, existing defect of the upper jaw, bite, obturating prosthesis, CT scanThe patient was noted to have no nasal lining, and to anatomically restore aeration, before transplanting a microsurgical graft, the nasal lining was formed with local tissues.
Rice. 2. Stages of planning the bone and soft tissue components of the graft Rice. 3. Stages of surgery Rice. 4. Computed tomography of the patient after surgery and condition on the third day
Rice. 5. Scintigram after surgery
In the postoperative period, there was a divergence of the sutures and a reduction in the volume of the flap, and therefore a protective mouth guard was made to protect the soft tissue component of the flap from food getting into the graft. Kappa also pressed the flap into the defect area to allow healing by secondary intention.
Rice. 6. Postoperative mouth guard2 months later, the patient, being a cycling athlete, fell from the “saddle” and received a fracture of the upper limb at the site of collection of the radial skin-cortical-periosteal graft on the vascular pedicle. Therefore, the patient underwent osteosynthesis with the Ilizarov apparatus.
Rice. 7. Condition after osteosynthesis of the upper limb on the left, condition in the oral cavity Rice. 8. 3D reconstruction of the alveolar process using parietal grafts, CT scans after the second operationAfter 5 months, we installed three dental implants in the area of the reconstructed alveolar process using parietal bone autografts. Thanks to this technique for reconstructing the alveolar process, it was possible to obtain adequate bone thickness and height for placing dental implants.
Rice. 9. Implantation in the area of 3D reconstruction with parietal blocksAfter 5 months, we opened the implants and applied a method of one-stage surgical correction of the subcutaneous fat pad of the autograft with the installation of elongated gum formers in dental implants, which simplified the formation of soft tissues during surgery.
After completion of the surgical stage, the alginate impression was removed from the upper jaw and a compression plate was made using cold polymerization at a pressure of 3 atmospheres from acrylic plastic.
The patient was advised to wear the plate constantly, removing it only for hygiene procedures. Inspection and correction of the plate fit were carried out every seven days for a month.
Thus, we were able to form a stable mucosal contour around the gingival formers.
The next stage was the production of a conditionally removable prosthesis supported on a beam structure on implants.
Rice. 10. Correction of the subcutaneous fat area of the autograftConsidering the fact that microsurgical elimination of the jaw defect and reconstruction of the alveolar process was carried out by transplantation of free parietal cortical autografts, the further stage of orthopedic rehabilitation is practically no different from classical prosthetics for patients with an extended terminal defect of the dentition.
In order to be able to produce a conditionally removable beam-type prosthesis supported by implants, it was necessary to produce an accurate plaster model that displayed the entire relief of the prosthetic bed and accurately reproduced the position of the implants. To do this, we took primary impressions of the upper jaw using Clip-transfers for implants. The primary plaster model gave us the opportunity to make a custom impression tray with prepared transfer checks for precise transfer of the position of the implants.
Having made an accurate working model of the upper jaw and a model of the antagonists, we installed them in the articulator according to the average parameters. Registration of the central ratio was carried out using an occlusal hard wax plate with refinement on ALUWAX (soft wax with the addition of aluminum filings for long-term heat retention and elasticity).
Rice. 11. Impressions and plaster modelsAfter analyzing the relationship of the plaster models in the articulator, we manufactured a beam frame supported by three implants. The beam frame was made by vacuum casting from cobalt-chrome alloy. To achieve a passive fit of the frame, we used adapters for external connection with the implants.
We fixed titanium ball locks into the cast part of the frame. Then a model of the upper jaw was made from a fire-resistant mass for modeling and casting the mating part of the prosthesis itself.
Rice. 12. Beam frame and mating part of the prosthesisTaking into account the possibility of changing the relief of the soft tissue component of the autograft, the frame of the response part was modeled in such a way that it was possible to change the acrylic base part, changing the fit of the prosthesis to the bed.
After fitting the beam and frame in the oral cavity, we manufactured the base part of the conditionally removable denture with the installation of acrylic artificial teeth, using the method of cold polymerization of plastic under a pressure of 3 atmospheres and a temperature of 50 degrees Celsius. We took into account all possible characteristics of the patient at rest and when smiling, creating the most natural appearance of the entire orthopedic restoration.
The final fixation of the prosthesis was carried out in a certain sequence:
- Cleaning and disinfection of all components of the prosthetic restoration.
- Removing the gum formers, irrigating the internal shafts of the implants with a solution of 3% hydrogen peroxide and 0.05% chlorhexidine solution, installing adapters on the external connection.
- Installation of the beam structure on three implants, tightening the fixing screws with a force of 30 N/cm2.
- Fixing the actual removable denture on the beam frame, checking the occlusion, teaching the patient about hygienic measures.
Medical Internet conferences
Relevance: Prosthetics for patients with acquired jaw defects is one of the most difficult tasks in dentistry. Due to the complexity of the relief of the prosthetic bed, and the variety of clinical cases, it is necessary to have a clear understanding of the technique of prosthetics for such defects and the design of dentoalveolar prostheses.
Goals and objectives : To become familiar with the technique of prosthetics for patients with acquired defects of the upper and lower jaws. As well as the design features of dentures.
Article: Prosthetic designs used to treat patients with jaw defects, depending on the topography of the defect of the face and jaws, are classified into intraoral dentofacial ones, as well as combined ones, combined with extraoral facial epitheses.
Orthopedic structures are divided into preoperative and postoperative (post-resection) jaw prostheses.
The designs of ectoprostheses used at different stages of prosthetics have significant design differences, which is associated with their functional purpose.
Goals and objectives of direct prosthetics:
— formation of the future prosthetic bed.
- prevention of the formation of keloid scars.
— reposition and fixation of the fragments of the lower jaw remaining after the operation.
- restoration of speech and chewing disorders.
- prevention of severe facial deformations and changes in appearance.
- awareness of the therapeutic and protective regime.
Technique of prosthetics for patients with jaw defects.
The existing principles of providing orthopedic dental care to patients with acquired jaw defects are based on the use of effective design solutions when creating prostheses and methods for their manufacture, and improved dental materials. This concept and model of complex rehabilitation is multi-stage and for almost every stage of treatment of patients with acquired defects of the upper or lower jaw requires the manufacture of several medical devices using special and auxiliary materials and technologies.
Design features of dentures.
Features of fixation.
The effectiveness of orthopedic treatment of patients with facial and jaw defects largely depends on the reliability of fixation of replacement prostheses, which is optimally ensured in the presence of teeth.
When choosing a design and planning treatment stages, you must:
— Make maximum use of remaining teeth, even mobile ones, by splinting them first.
— Take into account the conditions that have formed after surgical intervention, and to improve the fixation of the prosthesis, make maximum use of the retention properties of the alveolar processes, bone fragments, soft tissues, and cartilage that limit the defect.
In the early postoperative period, in the complete absence of teeth and difficult anatomical and topographic conditions of prosthetics, when it is impossible to achieve high-quality fixation of the structure using conservative methods, surgical methods are used to strengthen the disconnecting prostheses.
The number of fixing elements of a dentoalveolar prosthesis should increase as the volume of the structure increases.
Methods aimed at increasing retention and stabilization of dentures are very diverse. As a rule, clasps (retaining and support-retaining), artificial crowns, magnetic retainers, telescopic, locking and beam systems are used as fixing elements of dentures. It is especially important, taking into account the basics of biomechanics, to use indirect fixators (kipmakers), which protect the prosthetic structure from tipping over.
The correct choice of fixation method is determined not only by the fixation characteristics of the device, but also by the ability to redistribute functional loads, which reduces the risk of overloading the periodontal tissues of abutment teeth. The rational use of fixation methods, taking into account existing individual characteristics and anatomical conditions, ensures the restoration of the basic functions of the dental system, facial aesthetics and improvement of the psychological state of patients.
In the case of complete absence of teeth, the structure of the jaw prosthesis is fixed using the remaining anatomical formations. In most clinical cases, fixation of jaw prostheses in the complete absence of teeth is difficult and sometimes impossible, so it is advisable to use dental intraosseous or magnetic implants. Along with this, it is necessary to take into account that creating reliable fixation using artificial supports is not always possible in cancer patients, especially those who have received radiation therapy and chemotherapy, since relatively often they need surgical correction due to the progression of the underlying disease. In addition, the formation of scars and the loss of a large mass of the bone skeleton of the upper jaw do not always allow the use of dental implants in patients with defects of the upper jaw caused by trauma and benign neoplasms. In such cases, the obturating part of the jaw prosthesis can be used as a retainer.
Arutyunov A.S. in 2012, a model of the defect of the upper jaw with different thickness and compliance of the free edge of the mucous membrane of the prosthetic bed for the obturating part of the dentoalveolar prosthesis was proposed, the advantages of one or another configuration of the obturator holding the maxillary prosthesis on the upper jaw with partial and complete absence of teeth were determined. Based on the established dependence of the forces of insertion and removal of the obturator of the jaw prosthesis on the properties of the elastic base materials and in accordance with the individual characteristics of the geometry of the defect of the upper jaw, it is possible to calculate the optimal design parameters of the obturator. This approach makes it possible to design an obturator of a dentofacial prosthesis in the presence of teeth of the “lid” type, without penetrating into the space of the anastomosis between the oral and nasal cavities, and in the absence of teeth of the “plug” type, which increases the efficiency of the jaw prosthesis due to the optimal design parameters of the obturator.
This is especially effective when a rigid base polymer is combined in the design of a prosthesis with an elastic polymer of acrylic nature or a special silicone material.
Often, the clinical situation of a postoperative defect in the complete absence of teeth does not allow the use of obturators made of rigid structural materials due to the thinned mucous membrane lining the anastomosis, to ensure sufficient fixation of the structure of the maxillary prosthetic obturator on the upper jaw. To eliminate this problem, it is recommended to use a jaw prosthetic obturator, the base of which is made of a rigid material, and the full obturator is made of an elastic structural material.
This design allows for retention and stabilization of the jaw prosthetic obturator, taking into account the elasticity of the mucous membrane of the edge of the defect (fibrous ring of the anastomosis) of the upper jaw and the structural material of the obturator.
Along with this, to improve the fixation of jaw prostheses in the complete absence of teeth, the use of fixatives of a chemical nature is indicated - films, adhesive gels, powders that swell in the oral cavity and provide stickiness and adhesiveness, anti-inflammatory and wound-healing effects, capable of compensating for the lack of congruence between the inner surface of the prosthesis base and relief of the mucous membrane of the prosthetic bed. These products are widely used by patients with large plate dentures and complete absence of teeth.
In case of jaw defects, there is often a need for combined prosthetics, when fixed dentures are used to splint teeth and provide fixation of removable dentures.
Features of the manufacture of dentoalveolar and maxillary prostheses for both the lower and upper jaws are that at the first stage it is necessary to make a construction base (metal and plastic) with support-fixing elements, which is carefully fitted in the mouth and used in determining the central occlusion and positioning of teeth and checking the design of the prosthesis. This approach makes it possible to facilitate clinical stages and accurately adjust the boundaries of the prosthesis, especially in the area of scar tissue.
However, in a number of cases, experienced orthopedic dentists make dentures without the fitting stage, if there are antagonizing pairs of teeth that make it possible to fix the height of the lower part of the face and the position of the lower jaw in the usual occlusion.
The objectives of maxillofacial prosthetics, the choice of a replacement structure and the planning of prosthetic features are determined by the volume of surgical intervention:
- on the upper jaw - during resection of the alveolar process, unilateral and bilateral resection of the body of the upper jaw.
- on the lower jaw - during resection of the alveolar part, the chin with loss of continuity of the bone, while maintaining the continuity of its body, half of the jaw and its complete removal.
Prosthetics of defects of the upper jaw.
Resection of the alveolar process, one- and two-sided resection of the body of the upper jaw are the main surgical interventions on the upper jaw, leading to the formation of defects of the same name.
Before taking an impression of the upper jaw, which has an oronasal anastomosis, it is necessary to replace the defect with a long gauze swab, previously soaked in a glycerin mixture. The tampon is placed sequentially in continuous layers, taking into account the remaining anatomical formations, and carefully so as not to push it into the nasopharynx, the defect is completely isolated. With a correctly placed tampon, the impression material does not penetrate into the undercuts of the nasal cavity and maxillary sinus. Otherwise, when removing the impression, part of the impression mass may come off, it may be retained in the niches formed after surgical intervention, which subsequently threatens inflammation, the etiology of which doctors do not immediately and not always recognize. Sometimes only surgical revision allows one to identify the cause of inflammation and stop it.
Using a thermoplastic mass, a standard tray is adapted to the oral cavity, active and passive movements are used, and the edge of the impression is formed along the border of the transitional fold and in the area of the defect. The spoon is inserted into the mouth and pressed all the way to the jaw. Active and passive movements are used to form the edge of the impression along the border of the transitional fold and in the area of the defect. The spoon is removed until the mass has completely hardened and the outer gauze is removed. An impression mass is applied to the surface of the preliminary impression, covered with an inner layer of gauze. The spoon is inserted into the mouth and pressed against the jaw. After structuring the impression mass, the impression is removed from the oral cavity and a plaster model is made from it, on which the areas to be isolated, as well as the remaining teeth, are covered with adhesive plaster or lead foil. If the model has a complex defect relief, then use a parallelometer to fill in the undercut areas. An individual spoon is prepared according to traditional methods
An individual spoon is fitted, the edges are formed with thermoplastic mass. Functional tests are performed under the pressure of the forces of the masticatory muscles and under the supervision of a physician. The impression is made using impression material. After its structuring, the impression is removed from the oral cavity along with a tampon, a fragment of which connected to the impression is cut off. The remaining part of the tampon is removed with tweezers. The upper jaw defect is washed with an antiseptic solution.
There is another method of taking an impression, when the alginate impression mass is applied to a standard tray and then covered with two layers of gauze. The tray is placed on the upper jaw and, after structuring the impression mass, removed from the oral cavity. Despite the simplicity of the method, the orthopedic dentist must have extensive experience in order to avoid the complications described above.
Arutyunov proposed a method for obtaining an anatomical impression with an alginate mass using a standard spoon, according to which a plaster model is made. An obturator is modeled on it by lining the positive image of the palate defect with wax while simultaneously modeling the resected alveolar ridge. The resulting composition is placed in the oral cavity and adjusted by filling any gaps with wax. An impression is obtained from which an individual spoon is made. The resulting spoon is adapted to the oral cavity using functional tests. Retention metal staples are installed in a wax obturator fixed in the jaw defect. A corrective layer of silicone impression mass is applied to the resulting composition, after which an impression is obtained using a previously made individual tray with a base layer of the same mass added to it.
Prosthetics for mandibular defects.
The effectiveness of prosthetics for patients with acquired defects of the lower jaw largely depends on the etiology, topography and extent of the defect in the lower jaw, as well as changes in the mucous membrane.
In the modern world, the approach to replacing defects of the lower jaw has changed significantly. Successfully performed osteoplastic operations make it possible to obtain an optimal prosthetic bed for prosthetics.
However, traditional orthopedic treatment of patients with dentures with polymer bases is not always effective, this is due to the occurrence of functional overloads of the tissues of the prosthetic bed when biting and chewing food. The load falls through the artificial teeth onto the base or frame of the prosthesis, which leads to the appearance of a deflection zone under the saddle or base. In the zone of concentrated load, tension occurs not only in the soft tissues, but also in the bone around the graft or implant, which leads to disruption of tissue trophism and their subsequent atrophy, as well as scarring of the mucosa.
To avoid the above complications, Astashina proposed an alternative method of prosthetics for patients using dentoalveolar prostheses with multi-thickness solid titanium frames after plastic preparation of the prosthetic bed. The use of such a design prevents the occurrence of functional tissue overload.
The technique for making such a design consists of taking an impression, making and analyzing diagnostic models, planning the design of the prosthesis in accordance with the recommendations of the maxillofacial surgeon. Next, a plaster working model is made, and an individual tray is made from it, and it is fitted in the oral cavity. The boundaries of the spoon are clarified visually, and then fixation is achieved using functional tests. The functional impression is obtained using alginate or silicone impression materials, the choice of which is based on the pliability of the mucous membrane. To create volume, the edges of the working print are edged.
Subsequent stages include obtaining a functional impression from the lower jaw and an anatomical impression from the upper jaw, making working models from superplaster, determining the central occlusion or central relationship of the jaws. For microstomia, it is necessary to use wax templates with rigid bases. The dentofacial prosthesis is constructed in an articulator, and the spatial arrangement of the jaws is determined by the upper jaw and transferred using a face bow.
The main difference between creating prostheses of different thicknesses with titanium frames is the peculiarities of the stage of formation of the wax composition. According to standards, the thickness of the saddle part is 0.5 mm, and the dimensions of the arc are 4.0x2.0 in diameter, while the edge of the base is edged with a wax blank in the form of a cord with a diameter of 0.8 mm.
When modeling the frame or base of a prosthesis to replace a defect, it is rational to increase their thickness to 2.0-2.5 mm in the following areas: in the area of the saddle located above the graft or implant, as well as in the zone of transition of the structure’s saddle into the arch. The edge of the base stop must be edged with a wax blank with a diameter of 1.0-1.2 mm. This approach ensures a reduction in the level of developing functional stresses in the area of the graft or implant. Since titanium alloy has a low specific gravity, such an increase in the volume of the structure frame does not negatively affect the functions of the dentofacial system.
After the wax reproduction modeling stage, the frame of the removable structure is cast on a fireproof model. Minor casting defects (cracks, pores) are eliminated using solid-state laser welding and titanium powder.
Next comes the fitting of the frame on the model and in the mouth. Installation of artificial teeth. It is better to carry out this stage in the articulator. When checking the denture in the oral cavity, you should pay attention to the articulation of the lower jaw. Next, the wax is replaced with plastic. Before handing over the work, the prosthesis must be carefully ground and polished.
Conclusion: We examined the technique of prosthetics of jaw defects with dentoalveolar prostheses. The advantage of orthopedic treatment of patients using dentofacial prosthetic structures made on the basis of titanium alloys is their durability, the possibility of reusing frames in case of loss of supporting teeth and correction of the structure in order to reduce the adaptive period.