Root canal treatment is a common dental procedure. A poorly treated tooth contains microbes that the body fights. But if the immune system weakens, toothache appears and gumboil forms. Endodontic treatment will be carried out by our qualified specialists at the dental center.
What diseases are they susceptible to?
If problematic root canals are not treated, there are risks of serious consequences. The inflammatory process will not go away on its own, but can spread to nearby tissues and harm the entire body. It can negatively affect the organs located in the upper and lower jaw. There is a danger that a constant source of infection in the oral cavity will provoke the development of the following diseases:
- lymphadenitis;
- cellulitis or abscess of soft facial tissues;
- endocarditis;
- pyelonephritis;
- orthodontic sinusitis;
- sepsis.
What are the nuances of root canal retreatment?
Before performing the procedure, several preparatory steps are required:
- The channel is “opened” - a hole is drilled to access it.
- The material remaining from the previous filling is removed.
- The specialist examines the work area under high magnification so as not to miss structural features and minor defects.
After this, root canal retreatment is performed:
- Processing them with tools along the entire length
- If necessary, medications with anti-inflammatory effects can be used, which the doctor places under a temporary filling.
- After this, the canals are filled again with a filling compound, and the top is covered with a filling, dental inlay or artificial crown.
Teeth retreatment is carried out under a microscope, which allows the specialist to detect even tiny additional holes and not miss them during the treatment process. High-quality magnification helps the doctor work with pinpoint precision.
The technique has a serious advantage over other techniques because it preserves your own tooth, which works well and looks great for many years.
How do they treat qualitatively and poorly?
Recently, the quality of endodontic treatment has improved. Previously, pastes were used to re-treat root canals. After a couple of years, they resolved, after which granulomas and cysts appeared. They also used formaldehyde compounds, which caused complications, and painted the element a light brown shade. The open space was filled with cement, which did not always give a good result. In addition, there was no suitable tool.
Nowadays, re-treatment of root canals is carried out using gutta-percha. This material makes it possible to tightly heal the desired areas with a minimum of complications. The client is given a guarantee that the filling will not dissolve after many years. Methods for treating dental canals and antiseptic agents for medicinal treatment have also changed. New diagnostic methods make it possible to assess the complex anatomical features of the tooth and choose the right treatment tactics.
When performing root canals, the dentist must fill the space to the top of the root. The material on radiography should look full, of the same shade and consistency, without voids. The bone on top of the incisor should not show signs of inflammation.
High-quality treatment requires a well-equipped office, sufficient skills and qualifications of the doctor.
Why re-treat canals?
Endodontic dental treatment is not always carried out in line with modern trends and requirements. According to statistics, complications in the form of chronic inflammation occur in 60-70% of patients. Treatment of dental canals is a painstaking work that must be performed by an experienced doctor using modern high-precision equipment and functional tools.
The following shortcomings of the previous intervention may serve as a reason for revising the channels:
- the presence of unfilled areas (voids). The reason is incorrect measurement of the channel length and insufficient machining;
- poor-quality filling materials, due to poor fit of which the canals become depressurized and infection opens;
- fragments of pins and instruments stuck in cavities;
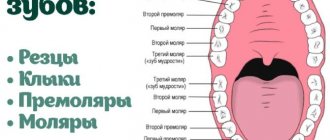
- passage of additional channels and closing them along with the remains of the pulp (creation of an infectious “depot”). Molars usually have three canals, but there are specimens with four or five - they are the ones that remain “unaccounted for”;
- insufficient expansion and poor-quality cleaning of canals, formation of “steps” and root perforations due to deviation of the instrument from the anatomical shape of the course. The result is an under-processed apical part of the root (the apex of the root in dentistry means its lowest point).
As a result, the infection from the canal enters the gum tissue, and foci of chronic inflammation develop at the root tips - apical granulomas and radicular cysts. Such formations were previously considered an absolute indication for tooth extraction (cystectomy).
Endodontic treatment of tooth canals using optics
Such verdicts were completely justified, since a progressive cyst can lead to gum deformation, destruction of bone tissue (osteomyelitis), periodic inflammation and suppuration. Some dentists still consider removing a tooth with problematic roots to be the only rational option.
The IMEZA clinic has the personnel and technological capabilities for complete sanitation of cystic formations while preserving the dental unit. Our specialists have experience treating patients who were previously scheduled for tooth extraction due to the presence of foci of chronic inflammation. But there are cases when cystectomy is really the only option - destruction of more than 2/3 of the root or the impossibility of restoring the functionality of the dental unit.
Timely retreatment of questionable canals will help avoid complications and tooth loss. Our doctors objectively assess the risks and feasibility of manipulation for each individual patient, taking into account the degree of destruction of the crown and roots, the functional load on the tooth, and the possibility of subsequent restoration.
For what reason do you have to re-treat?
Reasons for root canal retreatment:
- pain after filling;
- when tapping, sensitivity appears;
- slight swelling;
- insufficient filling of the canal with paste;
- use of quickly deteriorating filling material;
- ineffectiveness of primary filling;
- incorrectly restored crown;
- re-infection of the root tip;
- mechanical damage or injury.
Unsealing will also be required if a secondary infection of the apex has occurred, the filling has lost its tightness, or a complex anatomical arrangement of the canals is noted.
Reasons for re-treatment
Canal retreatment is carried out if:
- the initial treatment was of poor quality (the roots of the tooth were poorly cleaned or not completely filled);
- re-infection of the tooth occurred;
- inflammatory processes have begun;
- there was pain in the tooth;
- a fistula has formed;
- swelling is noticeable;
- the tooth became sensitive to percussion.
Tooth canals are also re-treated before prosthetics to prevent inflammation and tooth decay.
The reasons for poor quality primary treatment can be:
- unprofessionalism of the doctor or lack of experience;
- lack of knowledge of endodontic treatment protocols;
- lack of necessary equipment;
- use of low quality filling materials;
- incorrect diagnosis;
- instrument fragments remaining in the tooth canal;
- root perforation;
- anatomical features of the canals (narrowness of the canals, atypical location of the inputs, the presence of convolutions or steps);
- morphological changes in dental canals (obliteration, calcification, hypercementosis);
- filling or prosthetics of a tooth after a long period of time after root canal treatment.
How does the procedure work?
Root canal retreatment proceeds according to the following scheme:
- Carrying out diagnostics, evaluating the data obtained.
- Anesthesia is provided, a coffee frame is placed on the incisor, the old restoration is drilled out and all access is opened.
- Removal of early placed material, then clean the root space.
- The open area is treated with disinfectant medications.
- The canals are thoroughly cleaned, then the medicine is put on, usually for several weeks. This is necessary for repeated disinfection.
- Re-sealing, with installation of the necessary structures.
- Restoration of a coronal fragment (prosthetics or direct restoration).
How to increase the effectiveness of retreatment?
For re-treatment to be effective, it is necessary:
- use a special microscope and other equipment;
- use only high-quality filling materials;
- thoroughly clean and fill dental canals;
- exclude any errors and inaccuracies.
Retreatment of tooth canals under a microscope will be necessary if:
- an instrument broke in the dental canal, leaving fragments;
- perforation of the tooth root occurred;
- there are steps in the root canals;
- the channels are not completely sealed.
The microscope allows you to clearly visualize the condition of the dental canals in difficult cases, remove all foci of inflammation and carry out effective tooth treatment.
Canal retreatment is a very complex procedure that does not always end in success. The experience and qualifications of the doctor are of paramount importance in the successful completion of the procedure. Therefore, you should only contact a well-established clinic.
Indications and contraindications
Root canal retreatment is indicated in the following cases:
- X-ray shows a hidden inflammatory focus;
- loose, low-quality filling;
- the infection has spread to the tissues near the incisor;
- pain remains after endodontic treatment;
- being inside a part of the instrument;
- the channel is not completely filled;
Absolute contraindications to the procedure:
- there is no way to restore tooth function;
- the periodontium is absent for 2/3 of the length of the dental rhizome;
- severe general condition of the patient.
Relative contraindications include the inability to gain access to the incisor, poor oral hygiene and restrictions when opening the mouth.
Non-surgical endodontic retreatment of extensive periapical lesions
Apical periodontitis and the accompanying periapical bone resorption are inflammatory lesions of the periradicular region caused by the persistence of microbial infection in the root canal system of problem teeth. Apical periodontitis, which does not go away after root canal treatment, has a more complex pathogenetic mechanism of development compared to the usual analogue of this pathology.
The most common reasons for failure of endodontic treatment are inadequate cleaning of the root canal system from microbial pathogens, or re-infection of the canals due to a violation of the tightness in the crown area, the influence of extra-radicular infection, host reactions to a foreign body and recurrence of true cysts.
In such cases where primary endodontic therapy has failed, a non-surgical endodontic retreat is the best option to achieve successful clinical results. The main difference between primary and retreatment is the different approach to providing access to the apical third of the root canal. Once adequate access conditions have been achieved, the subsequent endodontic intervention protocol is similar: cleaning, preparation and preparation, and root dressing. The most commonly used drug in endodontics is still calcium hydroxide Ca(OH)2. Its antimicrobial properties and high pH value (12.5) provide conditions in which only rare microorganisms can survive. In addition to calcium hydroxide, iodoform (CHI3) has also been widely used for many years, which also exhibits influential antibacterial properties.
Vitapex (Neo Dental International) is a commercial form of calcium hydroxide Ca(OH)2 paste, and can be used as a root dressing in primary and permanent teeth; In addition, this drug contains iodoform CHI3, which inhibits and destroys pathogenic microflora of the root canal. Vitapex is also unique in that it can stimulate bone repair and regeneration, as demonstrated by Xia et al. Despite the fact that calcium hydroxide is reasonably considered to be quite effective against pathogenic bacteria, the disadvantage of pastes based on it is that they are difficult to remove from the root canal area. Passive ultrasonic irrigation (PUI) has been shown to be 63.3% more effective in this procedure than conventional sodium hypochlorite irrigation. This percentage is justified by the effects of cavitation and acoustic effects on sodium hypochlorite NaOCl under the influence of ultrasonic waves. However, whether the PUI procedure is absolutely effective in removing Ca(OH)2 from the root canal wall area is still unknown.
There are cases when calcium paste is unintentionally removed beyond the root apex, which can be considered a medical error. However, in cases of large and chronic periapical lesions, this procedure is even recommended by some researchers, who suggest that calcium excretion beyond the apex promotes healing of periapical lesions and bone regeneration. This approach rather overestimates the capabilities of calcium hydroxide rather than taking into account all aspects and consequences of possible complications.
Clinical case
A 42-year-old female patient was referred to the dental clinic for treatment of a maxillary left lateral incisor. The reason for the appeal was also the fact that endodontic treatment had once been started on this tooth, which had remained unfinished for 2-3 years. During the history taking, it was discovered that approximately 3 months ago the patient experienced pain in the area of the problematic tooth, accompanied by the development of a fistula. The patient also reported pain when chewing that began 3 days ago. Clinical examination confirmed the presence of purulent exudate in the gingival margin; Fillings were also found in the area of the access cavity on the palatal side (Figure 1).
Photo 1. The patient complained of pain when chewing, but no area of contact with antagonists was found on the surface of the tooth. Signs of caries on the palatal surface can be detected using a microscope.
The right lateral incisor was also mildly sensitive to percussion and palpation. Radiographic examination (Schick CDR, Schick Technologies) revealed the results of very acceptable endodontic treatment, as well as the presence of periapical pathology of approximately 10 mm in diameter (Figure 2).
Figure 2. Acceptable endodontic treatment with a periapical lesion (approximately 10 mm in diameter).
The non-surgical retreatment algorithm was agreed upon with the patient by signing an informed agreement. The treatment was carried out without local anesthesia and using a rubber dam. The access cavity was prepared with a No. 2 carbide bur (Mani) and Endo-Z (Dentsply International). Removal of gutta-percha located in the canal was performed using ProTaper files (Dentsply Tulsa Dental Specialties). After removing the calcium hydroxide paste found in the canal, rinsing was carried out using 2.5% sodium hypochlorite. The canal was dried with sterile paper points (Coltene Whaledent Group, Hygenic), after which calcium hydroxide powder (Sultan Healthcare Inc.) was placed into the cavity to control exudation. The tooth was temporarily filled with restorative material (IRM Caulk; Dentsply). Clinical evaluation of the results was carried out after 10 days (Figure 3).
Photo 3. View after removing gutta-percha and placing calcium hydroxide powder into the canal cavity to control exudation. When re-examined 10 days later, no associated symptoms were observed.
No symptoms of pain were noted. Once the rubber dam had been placed and adequate re-entry had been achieved, the working length of the canal was determined (Figure 4) using an electronic apex locator (Root ZX, J. Morita) and a 45 file size (Mani).
Photo 4. Determining the working length using the Root ZX apex locator.
The channel was again flushed with 2.5% NaOCl and similarly dried. Vitapex was placed into the canal cavity as a root dressing, which was deliberately moved beyond the area of the apical foramen (photo 5).
Photo 5. Vitapex was used as a therapeutic material, which was taken beyond the root apex area.
A cotton swab was placed in the pulp chamber area and the tooth was rebuilt with a temporary filling (IRM Caulk; Dentsply). After this, the patient returned for a follow-up appointment 17 months later, because for reasons known to her, she had lost all contact with the clinic. The patient complained of slight pain in the area of the metal-ceramic crown installed on the core inlay (in the area of the tooth in which endodontic treatment was previously carried out but was not completed). After removing the crown and inlay, the canal was further prepared using F4 and F5 ProTaper files (photos 6 - 7).
Photo 6. After 17 months, the patient again sought help due to pain in the area of the crown fixed to the problem tooth. The periradicular lesion decreased in diameter, but still did not completely disappear.
Photo 7. Canal preparation and Vitapex removal were performed using Protaper F4 and F5 files.
After this, obturation was performed using lateral condensation of gutta-percha and using Sealapex as a sealer. At a follow-up visit 1 month later (photo), the patient did not experience any symptoms, and signs of the beginning of restoration of the defect were visualized in the area of the periapical lesion.
At a follow-up visit 1 month later (photo), the patient did not experience any symptoms, and signs of the beginning of restoration of the defect were visualized in the area of the periapical lesion.
Photo 8. View after 1 month: the area of the periapical lesion has almost completely disappeared, the tooth has not yet been restored with a crown.
For preventive purposes, a crown has not yet been made. The patient again disappeared from sight for 1 year, but then returned: no signs of periapical changes were observed, and tooth function was completely restored (Figure 9).
Photo 9. 1 year after treatment, complete recovery of the periapical lesion area is observed.
Discussion
Under the influence of microbial load, necrosis of the dental pulp leads to infection of the root canal system. Microorganisms that live in the oral cavity, such as bacteria and fungi, cause a protective inflammatory response in the periradicular tissues. But cases arise when the cells of the host's immune system are unable to limit the area of bacterial invasion to the space of the canal, and in such cases the inflammatory process leads to the formation of abscesses, granulomas, and/or periapical cysts. This process has been studied in detail by Love and Firth, Soares and colleagues. Such damage can only be detected radiographically when bone loss of the alveolar ridge is accompanied by damage to the cortical plate during the development of the pathological focus. The average diameter of periapical lesions ranges from 5 mm to 8 mm; lesions with a diameter of 10 mm or more are already classified as granulomas or apical cysts. The prevalence of radicular cysts is approximately 15% of all periapical lesions. It was found that in cases of apical periodontitis, repeated endodontic treatment provides an effective result in 80-95% of cases, which proves the fact that successful treatment in such cases can be achieved without surgery. Therefore, a conservative approach to treating such situations should always be considered by the clinician as one of the most effective.
Thomas, Dhanapal, and Simon have shown that surgery is not without its drawbacks: possible damage to adjacent vital teeth and anatomical structures, postoperative pain and discomfort - which is why the surgical algorithm for treating periapical lesions is quite limited. The conservative approach of the retreat focuses more on disinfecting the root canal and eliminating adjacent decay products from the root system. And if you strictly adhere to these approaches, you can ensure successful clinical results confirmed by radiographic data. Based on available research, it has been established that 92-98% of teeth after endodontic treatment are not subject to periapical tissue damage in the future, and 74-86% of teeth with already present signs of apical periodontitis are completely cured after high-quality primary or repeated endodontic intervention. In addition, individual studies indicate that 91-97% of teeth treated with endodontic therapy retain their functional value over time. However, in some cases, restoration of bone tissue in the area of periapical pathology requires a significant period of time, which makes it difficult to reliably predict clinical results after treatment. Sometimes the area of apical periodontitis is replaced by fibrous rather than bone tissue, which has a specific appearance on X-ray photographs. Broon and his colleagues focus on the impossibility of controlling the development of infectious lesions of the root canals during conservative therapy, which can result in a chronic inflammatory process. In such cases, many doctors recommend using intracanal dressings of the Ca(OH)2 type, which, if present in the canal for 1 to 4 weeks, helps to effectively get rid of bacterial contamination. The only disadvantage of pastes based on calcium hydroxide is the difficulty of removing them from the root canal space, which requires the use of not only file tools, but also the use of abundant irrigation with solutions of sodium hypochlorite and EDTA. Passive ultrasonic irrigation (PUI) has been shown to be 63.3% more effective in this procedure than conventional sodium hypochlorite irrigation. This percentage is justified by the effects of cavitation and acoustic effects on sodium hypochlorite through ultrasonic waves.
In this case, removing Vitapex beyond the root apex area may have affected the process of restoration of damaged tissue, but did not disrupt it in any way. The results of this clinical study are consistent with the findings of Arslan, Broon, Soares, Thomas, van der Sluis, and Xia that large periapical lesions can be treated without surgery; deliberate removal of Vitapex beyond the apex promotes healing of periapical lesions, and PUI in combination with sodium hypochlorite is an excellent approach for removing Ca(OH)2 paste from the root canal space.
conclusions
Even in cases where primary endodontic therapy did not allow complete disinfection of the root canal, it is imperative to consider a conservative retreat protocol as an alternative to endosurgery. In this clinical case, the use of calcium hydroxide/iodoform allowed for healing of the periapical lesion area within 1 month and complete restoration of the affected tissue within 1 year. The obtained result confirms the possibility and prospects of treating large periapical lesions using a conservative method without additional surgical intervention.
Authors: Dr. Fernando Munoz Ayon Dr. Jorge Paredes Vieyra Dr. Victor Manuel de la Torre Martinez
Specifics of teeth retreatment before prosthetics
Before prosthetics, a necessary step is thorough sanitation of the entire oral cavity. If bridges are installed, the supporting teeth experience increased stress. The same picture occurs with fixed prosthetics. To avoid inflammation under the prosthesis, so that the supporting teeth last longer, careful retreatment is necessary in compliance with the protocol. When re-treating a tooth for single prosthetics, it allows you to save adjacent teeth from preparation.
The cost of the 6th tooth and all the others during retreatment will not be high if it is done reliably. The patient will live for many years without toothache if the doctor followed all the nuances during retreatment.
Where to go?
Such a high-tech type of assistance, such as re-treatment of previously filled root canals, can only be offered by a few dental clinics in Moscow. And we are glad that ours is among them. The latest equipment and a team of experienced doctors who know advanced treatment methods help us provide modern services at a high level. The principle of our work: if a tooth can be saved, we need to use all methods to fight for it.
Cost of re-treatment of teeth under a microscope
Prices in different clinics vary from 5,000 to 25,000 rubles. The price varies depending on the status of the clinic, the qualifications and experience of the doctor, the chosen treatment method, the quality of the material, and the complexity of the intervention itself. But this is inexpensive compared to if you don’t use a microscope, re-treat not completely, and again encounter an infection in the same tooth. According to statistics, 70% of teeth can be treated under microscope control with a favorable outcome, but previously they were only removed.
Under the compulsory medical insurance policy, you can only receive a limited range of services. And endodontic treatment under a microscope is not included in the list. Private clinics do not work with compulsory medical insurance policies. The cost of retreatment under a microscope is not much different from the same, but without modern equipment. But diagnostics in the case of a microscope are an order of magnitude higher and more accurate. And the result can be used for many years, and no further dental intervention will be required.
On our portal you will find clinics with highly qualified specialists who know how to use a microscope to carry out modern, high-quality treatment.