In surgical dentistry, one of the most common pathologies is osteomyelitis of the jaw - a purulent-necrotic pathological process that affects the bone tissue of the upper or lower jaw. This is a serious disease that, without timely treatment, can lead to serious consequences. Young men under 40 years of age are at risk.
Why this disease develops, how to recognize it in time and what the treatment is - we will look in more detail in our article.
What causes the disease
The main culprit of the disease is pathogenic microorganisms. These are mainly streptococci and anaerobic bacteria that are present in the human oral cavity. They are the ones who trigger the infectious process that affects the jaw. But how do pathogenic bacteria get into bone tissue? There are several ways:
- An advanced carious process that has destroyed the hard tissues of the tooth and reached the pulp.
- Tooth injury – crack, filling defect, fracture. But not every mechanical damage will become a source of infection. The damage must be serious and deep. This also includes a broken jaw. But in this case, the inflammation is usually caused by a staphylococcal infection.
- Chronic infectious focus in another organ. Harmful bacteria can make their way to the jaw through the lymph nodes or blood vessels from a nearby organ (ear, throat, nose).
Most often, the disease is diagnosed in the lower jaw, since the teeth of the lower row are more susceptible to caries and various traumatic effects.
The risk of developing osteomyelitis increases in the presence of an immunodeficiency state, as well as diseases of the circulatory system. This is due to the fact that a person with such pathologies has poor wound healing, and the body is not able to resist infections.
Other factors provoking the disease include:
- smoking;
- alcohol abuse;
- diabetes;
- fasting or poor nutrition;
- syphilis;
- chemotherapy courses.
If the acute development of the disease is not completely cured, then chronic osteomyelitis of the jaw develops. It is more difficult to respond to conservative therapy and also more often leads to complications.
Acute odontogenic osteomyelitis
The development of an infectious lesion of the jaw most often occurs in an acute form. The clinical picture of acute osteomyelitis of the jaw is pronounced, so treatment, as a rule, begins in a timely manner.
There are three types of acute stages of osteomyelitis of the jaw.
- Toxic. The patient's body experiences severe intoxication due to the activity of the infection. Symptoms occur suddenly without any warning signs of the disease. the course of the disease is severe.
- Septicopyemic. Signs of osteomyelitis are pronounced, but the patient's condition is stable. If left untreated, symptoms expand and become more intense.
- Local. A mild form of inflammation in which tissues are affected locally (usually in the area of the tooth socket).
If acute odontogenic osteomyelitis of the jaw is not treated, a purulent process, abscesses and other complications may develop.
Classification of pathology
Depending on the method of infection, the following types are distinguished:
- Hematogenous - bacteria spread through the circulatory system from other infectious foci. This path is typical for secondary osteomyelitis of the upper jaw, which develops against the background of another disease. This could be scarlet fever, purulent otitis media, tonsillitis, or diseases of the larynx. First, the infection affects the bone tissue of the jaw, and then only the teeth and gums.
- Odontogenic – external route of infection. The cause is an infected pulp or tooth root. Predisposing factors include advanced dental diseases. These are pulpitis, periodontitis, the presence of cystic formations, alveolitis.
- Traumatic – fractures and injuries of the jaw joint with damage to soft tissues and the presence of fragments of the dentition. Often occurs due to late seeking medical help.
According to the course and nature of the manifestation of symptoms, the pathology can be acute, subacute and chronic. Based on the area of distribution, local (limited) and diffuse (diffuse) forms are distinguished.
General information
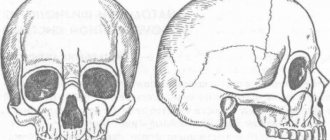
Osteomyelitis of the mandible is more common, more severe and has more complications. With chronic osteomyelitis of the lower jaw, the bone is affected deeper, which can lead to jaw fractures. Inflammation affects a dangerous area - the jaw processes. Acute osteomyelitis of the lower jaw easily turns into subacute and then chronic.
Osteomyelitis of the upper jaw develops more rapidly and can lead to inflammation of the maxillary sinuses. However, since the bone tissue here is less dense, abscesses and phlegmons develop less often with osteomyelitis of the upper jaw, and the disease itself is easier.
The entry point for infection is a diseased tooth, and the causative agents of inflammation are Staphylococcus aureus and Staphylococcus alba, pneumococci, Escherichia coli and typhoid bacilli. This microflora is usually located in areas of chronic infection of the tissues surrounding the tooth.
Inflammation in osteomyelitis does not occur suddenly; initially, a chronic infection develops in the gum for a long time - for example, in periodontitis or periodontitis. Then, if the outflow of waste products from the infection is disrupted, the microflora from the lesion spreads to the surrounding tissue.
Osteomyelitis of other parts of the skeletal system is caused by only one type of pathogen - staphylococcus (streptococcus), which penetrates the tissue through the bloodstream. Since osteomyelitis of the jaw can be caused by different pathogens, the course of the disease has much more distinctive features than with ordinary osteomyelitis.
Osteomyelitis of the upper jaw: symptoms and diagnosis
The disease develops slowly. The first symptom of a sluggish chronic inflammatory process is pain in the area of the damaged tooth.
The following manifestations are added:
- as the infection spreads, the pain intensifies and covers the area of several teeth or the entire jaw;
- swelling and redness of the gums;
- tooth mobility;
- local pain in the temple area, in the ear;
- numbness of the chin;
- difficulty swallowing and chewing;
- speech disturbances due to numbness or burning of the jaw;
- putrid odor from the mouth;
- enlarged lymph nodes as a reaction to severe inflammation;
- change in the shape of the face (swelling due to the pathological process).
Symptoms arise gradually in a chronic course.
Acute osteomyelitis of the lower jaw develops sharply. Accompanied by high body temperature and chills. If the outflow of purulent contents is disrupted, then purulent abscesses are formed, and the formation of perimaxillary phlegmon is possible. Such formations are dangerous and require surgical intervention. This dental pathology is often confused with another acute infectious disease - mumps (mumps).
Important! If your health suddenly deteriorates, you must call an ambulance.
On average, the acute period lasts 7–14 days. Then the symptoms subside and the subacute period begins. It occurs after the formation of a fistula to release pus from the source of infection. During this phase, the general condition improves, the pain becomes tolerable. But tooth mobility not only remains, but also gets worse. This leads to problems with chewing food and becomes a risk factor for the development of gastrointestinal diseases.
The subacute form often becomes chronic with a sluggish course that can last several months. The outcome is the rejection of all necrotic areas of bone tissue with the formation of sequesters (fragments of dead tissue). They are removed through the resulting fistula. This is a favorable outcome, which still requires examination and treatment by a specialist. However, the outflow of purulent contents is often difficult, which leads to damage to soft tissues, deformation of the jaw and the spread of the purulent process.
Which doctor should I contact: diagnosis of the disease
If you experience toothache of an unclear nature, as well as pathological changes in periodontal tissue, you should contact a dentist.
If necessary, he will refer you to a specialist - an orthodontist, surgeon or orthopedist.
The initial stage of the pathology may not yet be visualized using x-ray diagnostic methods. Therefore, collection and study of anamnesis and external examination are used.
The doctor pays attention to the following points:
- Degree of tooth mobility.
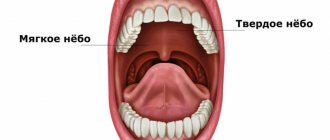
- Condition of the oral mucosa and gums.
- The presence of a painful syndrome when tapping.
Since osteomyelitis is a purulent infectious process that affects many processes in the body, it is advisable to prescribe laboratory general blood and urine tests. Also, to accurately determine the type of pathogenic pathogen, bacterial culture of the purulent contents is carried out.
In advanced forms of the disease (chronic or subacute stage), changes in bone tissue are already significant and noticeable, so an X-ray or computed tomography of the jaw is recommended. Such methods help to see the formed areas of dead tissue (sequestra), as well as to understand how deeply the inflammatory process has spread.
If there is a fistula tract with purulent contents, biomaterial is taken for laboratory testing. This is necessary to exclude actinomycosis of the maxillofacial area.
Important! The acute form of osteomyelitis must be differentiated from similar pathologies: purulent periostitis, festering cyst, acute periodontitis. Therefore, the experience and professionalism of the doctor is important here.
Diagnostics
Osteomyelitis cannot go away on its own; without medical help, the patient’s condition will worsen.
Periodontitis, cysts and tumors of the jaw, as well as lesions of oral tissue due to syphilis, tuberculosis, and fungal skin infections have similar symptoms. Therefore, self-diagnosis is highly not recommended.
When visiting the clinic you must:
- Undergo an initial examination of the jaw by a dentist. With osteomyelitis, tapping and palpating the affected areas will be painful.
- Take an x-ray. In the acute form, it is not very informative, but in subacute and chronic pathology, areas of change in bone density and areas of dead bone tissue will be noticeable.
- Take a general urine and blood test, a biochemical blood test, and bacteriological culture to identify the type of pathogenic microorganisms.
- Get a CT scan.
Prognosis and possible complications
With timely consultation with a doctor, accurate diagnosis and properly selected therapy, the prognosis is favorable.
Otherwise, the pathological process can spread along the descending and ascending paths. This threatens the development of the following complications:
- Meningitis
- Brain abscess.
- Phlegmon of the orbit.
- Sinusitis.
- Thrombophlebitis of the facial vein.
- Sepsis.
- Lung abscess.
- Mediastinitis.
These conditions have an acute onset and require immediate medical attention. Delay often ends in death for the patient.
The chronic form with sluggish inflammation negatively affects the condition of the soft tissues and bones of the jaw, and is accompanied by:
- fractures,
- deformation of the temporomandibular joint;
- formation of intra-articular adhesions;
- the formation of scar contractures of the masticatory muscles.
These pathologies significantly limit the mobility of the jaw or lead to its complete immobility.
Chronic osteomyelitis
Most often, chronic osteomyelitis of the jaw is a consequence of poor-quality, incomplete or untimely treatment of the acute form of the disease. In this case, the development of infection is considered a secondary type.
In the chronic form of the disease, until the moment of exacerbation, pathological processes occur hidden. After the acute stage of osteomyelitis of the jaw, in which bone tissue is destroyed, subsides, areas of necrotic tissue form at the site of the lesion.
Since the infectious process is not eliminated, after some time the next stage of osteomyelitis of the jaw occurs, characterized by a purulent process and the formation of fistulas. This period can last up to several months. Remission is mostly short-term. If treatment is not carried out, the pathology may result in the spread of infection to the brain, lungs, blood and other organs or systems.
Acute and chronic odontogenic osteomyelitis of the jaw requires mandatory treatment. The consequences of the infectious process can lead to severe complications that can lead to disability and death. Dentists recommend not only seeking help in a timely manner, but also completing all treatment until it is completely completed.
Toothache after caries treatment
Constant pain after filling can occur for many reasons. A common cause of discomfort is the application of an insulating lining made of glass ionomer cement (GIC) and filling on the same day with a composite. The polymerization times of GIC and composite differ, which can result in displacement of the gasket and its pressure on the pulp.
If the pain is short-term in nature as a reaction to cold, sour or sweet and quickly passes after removing the irritant, it may be due to the fact that during the treatment there was a mechanical effect on the pulp. After 2-3 days, the pulp will return to normal functioning and the pain will stop.
If you experience pain when biting, you need your dentist to grind the filling to fit your bite.
Treatment
The effectiveness of therapy depends on the initial causes of the formation of the inflammatory process. Therefore, in osteomyelitis of the jaw, comprehensive treatment is important, not only by a dentist, but it is recommended to go for a consultation with doctors of medical specialties.
- Sanitation of the oral cavity with antiseptic solutions. Further spread of infection to surrounding structures is prevented. Also, necrotic soft tissue formations are eliminated.
- Anti-inflammatory drugs. Minimize intoxication of the body.
- Immobilize the fracture, and if there is a tooth in it, then remove it.
- Taking antibiotics, regardless of provoking factors.
- Intraosseous lavage may be necessary and will provide positive results. Minimizes the occurrence of complications and quickly prevents the growth of a harmful process.
- In case of a fistula, sequestrectomy is performed - necrotic areas of bone tissue are eliminated under anesthesia, taking into account the extent of the damage.
- If the teeth are mobile, they are splinted.
- After eliminating symptoms and carrying out all interventions, physical therapy, vitamins and immunomodulators are recommended.
Prevention of such pathology consists only of timely and regular visits to the dentist’s office and treatment of pathological processes in the oral cavity. Do not treat yourself at home, so as not to make it worse. Also, it is necessary to strengthen the body’s immune system, avoid injuries and not let the pathological process become chronic.
Symptoms
Acute osteomyelitis appears very suddenly. If children are small, then they are noted to be moody and lethargic. They don’t want to eat, they don’t sleep well, and their temperature rises. If the child is older, then he may feel unwell, general weakness, and may complain of toothache.
When the disease is still in its early stages, the following manifestations may be present:
- bone pain. Initially it has a local character, and then diffused;
- the oral mucosa swells, hyperemia is noted;
- on the side that is affected, the soft tissues become swollen;
- the face becomes asymmetrical;
- chewing muscles may spasm.
If an injury occurs, signs of the disease appear after 3-5 days. The child feels much worse, the temperature rises, and pus may also be released if the mucous membrane has been damaged.
Prevention
Preventive measures are not only the key to preventing the development of osteomyelitis, but also a factor that reduces the risk of complications and shortens the recovery period if the disease cannot be avoided:
- Timely treatment of caries, even if it has no clinical manifestations.
- Maintaining normal immune status through regular physical activity, rational and nutritious nutrition.
- Sanitation of all chronic foci of infection in the body.
- In case of injury, in the postoperative period or after tooth extraction, compliance with all preventive medical prescriptions.
In conclusion, it should be noted that, despite all the achievements of modern medicine, osteomyelitis of the jaw in adults and children does not lose its relevance. Timely detection of its signs and adequate treatment increase the patient’s chances of a full recovery and maintaining a high quality of life.
»
Content:
- General information about the disease
- Types of osteomyelitis of the jaw
- Why does it occur
- How does the disease manifest itself?
- If left untreated
- Treatment of osteomyelitis of the jaw
- Prevention measures
Osteomyelitis of the jaw is an infectious-inflammatory dental disease in which all structural components of the jaw bone are affected.
Pathology can lead to osteonecrosis - focal death of hard tissue. According to statistics, osteomyelitis of the lower jaw occurs twice as often as the upper jaw. It is impossible to cure the disease on your own. It is necessary to make an appointment with a dentist and undergo therapy selected by a specialist.